Prolonged mechanical ventilation and chronic critical illness
Intensive care medicine has grown effectively in recent decades, parallel to multiple scientific and technological advances of our society. However, patients who survive the initial insult may have significant functional dependency, with slow recovery and high mortality rates (1-3).
Recently, Damuth et al. (4) have conducted an extensive meta-analysis of 124 studies comprising more than 300,000 chronically critically ill patients requiring prolonged ventilatory support, defining it as the need for mechanical ventilation (MV) for more than 14 days, the need for tracheostomy, or are discharge to a weaning unit. Although the analysis of the data was troubled by significant heterogeneity resulting from the pooling of data from heterogenous populations from different countries and healthcare systems, the results are alarming: around 30% of the patients, requiring prolonged MV did not survive to hospital discharge (totalling to a 60% mortality at 1 year). In addition, the study reported significant differences between the US and non-US studies. In summary, US studies reported significantly lower survival rates in the post-acute care hospitals and higher 1-year mortality together with less liberation rates from MV at hospital discharge.
The study raises several important issues that need to be addressed in future studies. In the accompanying editorial, Kahn (5) suggests further research to improve treatment that result in improved survival but also to address outcomes other than survival. These are two important directions to improve overall efficacy of treatment of critically ill patients requiring prolonged MV. In addition, Kahn identifies the need for research aimed to improve decision-making by the patient and/or relatives. In the presence of these poor outcome data, this is relevant in many ways. Especially since outcome data in post-acute care facilities don’t seem to improve much over time (6) and communication about the preferences of patient and surrogates is frequently poor and seldom (less than 10% of the cases) involves discussion about the patient’s values regarding autonomy, independence and physical function that are especially relevant to prolonged dependence on MC (7).
In addition, Kahn also addresses the need for a definitive definition of prolonged MV. We think that the whole multifaceted syndrome of prolonged MV in the context of chronic critical illness (CCI) needs to be addressed. In a recent process, the Research Triangle Institute developed a preliminary definition of CCI that when applied to 2009 Critical Care in the US resulted in a staggering health care expenditure of $26 billion. The definition of CCI was the presence of either of the following 5 conditions in patients admitted to an ICU for at least 8 days: MV for at least 4 days; tracheotomy; sepsis and other severe infections; severe wounds; and multiple organ failure, ischemic stroke, intercerebral hemorrhage or traumatic brain injury. As the main reason for this definition was a need to standardize the payment methods and sites of care for these patients, we don’t think this definition will help the clearly define the problem at hand. Nor the prolonged MV or even the presence of organ failure as such, really defines the problem as many patients dependent on dialysis or even MV have an acceptable quality of life. In the Center for Home Ventilation from the Department of Intensive Care Adults of the Erasmus MC University Medical Center, the patient requiring the longest duration of MV with tracheostomy has been ventilated for more than 60 years while having an active life. A few patients of the Center require both dialysis and MV. In the Netherlands, 96% of the patients requiring any mechanical ventilatory support are at home. So while prolonged MV has been thought of as the key element of CCI this clearly needs a better-defined context outside of the payment methods. A broader definition, based not only on the number of days of MV but also on the underlying pathophysiologic alterations, may best identify CCI and help for a more targeted research.
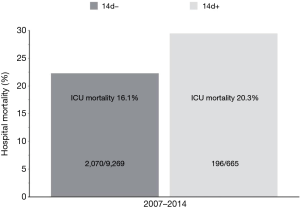
Another important issue from the study by Damuth et al. (4) is the poor performance outcome of the US studies when compared to the non-US studies. As the use of long-term-care facilities in the US keeps rising with a stable poor outcome (6) the question raised is “What is the best facility to take care of patients requiring prolonged MV?” In an analysis of the outcome of patients requiring prolonged MV (>14 days) at the Intensive Care Adults at the Erasmus MC University Medical Center from 2007–2014 we found that of the 9,934 patients requiring MV, 665 (6.7%) required prolonged MV. ICU mortality of these patients was 20.3% with an extra mortality on the general ward of 9.2% adding to a hospital mortality of 29.5% (Figure 1). Although these numbers don’t seem that much different from the data by Damuth et al. and especially from the US-studies included in the meta-analysis, almost all surviving patients requiring prolonged MV were discharged while liberated from MV. Improved outcome for completely weaned patients and removed tracheostomy has also been shown in US-studies of prolonged MV (8). As little is known about the care for patients requiring prolonged MV at post-acute care hospitals in the US (9), and the outcome of these patients can be improved by using specific treatment protocols in these facilities (10), a more detailed assessment of the differences between the care for patients requiring prolonged MV in different health care systems might help to resolve important efficiency issues before the results of large multicenter studies are available.
In addition to a clear definition of prolonged MV and CCI the early recognition of patients at risk of ending up in this condition is of key importance to optimise patient and family communication, recognising patient values and expectancies, identifying patterns for limiting treatments or DNR orders, and agree a rational management plan for the time to come. Identifying predictors of evolution to chronicity will also allow to develop preventive approaches, and advise family members on the problems facing chronic critically ill patients. In this sense, Carson et al. (11) identified four independent predictors of death in patients who required MV for 21 days or more: the need of vasopressors, platelets ≤150,000/mm3, age ≥50, and requirement of hemodialysis. Patients with more than 2 of these risk factors had a 3-month mortality of 90% and 1-year mortality of 97%.
In conclusion, patients requiring prolonged MV are part of the conundrum of chronically critically ill patients. Clear definitions of this syndrome lack and limit our understanding of the important context sensitive presence of long term single or even multiple-organ failure. Given the enormous impact on health care expenditure in different health care systems, the frequently limited survival beyond 1 year and the significant impact on the surviving patient’s and relative’s quality of life significant resources should be allocated to study the understanding of this syndrome and the optimization of care for patients and relatives alike.
AcknowledgementsOther Section
None.
FootnoteOther Section
Provenance: This is an invited Editorial commissioned by the Section Editor Wenhui Gong (Department of Cardiac Surgery, Ruijin Hospital of Shanghai Jiaotong University, School of Medicine, Shanghai, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
ReferencesOther Section
- Nelson JE, Cox CE, Hope AA, et al. Chronic critical illness. Am J Respir Crit Care Med 2010;182:446-54. [Crossref] [PubMed]
- Estenssoro E, Reina R, Canales HS, et al. The distinct clinical profile of chronically critically ill patients: a cohort study. Crit Care 2006;10:R89. [Crossref] [PubMed]
- Lamas D. Chronic critical illness. N Engl J Med 2014;370:175-7. [Crossref] [PubMed]
- Damuth E, Mitchell JA, Bartock JL, et al. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med 2015;3:544-53. [Crossref] [PubMed]
- Kahn JM. Improving outcomes in prolonged mechanical ventilation: a road map. Lancet Respir Med 2015;3:501-2. [Crossref] [PubMed]
- Kahn JM, Benson NM, Appleby D, et al. Long-term acute care hospital utilization after critical illness. JAMA 2010;303:2253-9. [Crossref] [PubMed]
- Scheunemann LP, Cunningham TV, Arnold RM, et al. How clinicians discuss critically ill patients' preferences and values with surrogates: an empirical analysis. Crit Care Med 2015;43:757-64. [Crossref] [PubMed]
- Engoren M, Arslanian-Engoren C, Fenn-Buderer N. Hospital and long-term outcome after tracheostomy for respiratory failure. Chest 2004;125:220-7. [Crossref] [PubMed]
- Kahn JM, Carson SS. Generating evidence on best practice in long-term acute care hospitals. JAMA 2013;309:719-20. [Crossref] [PubMed]
- Jubran A, Grant BJ, Duffner LA, et al. Effect of pressure support vs unassisted breathing through a tracheostomy collar on weaning duration in patients requiring prolonged mechanical ventilation: a randomized trial. JAMA 2013;309:671-7. [Crossref] [PubMed]
- Carson SS, Kahn JM, Hough CL, et al. A multicenter mortality prediction model for patients receiving prolonged mechanical ventilation. Crit Care Med 2012;40:1171-6. [Crossref] [PubMed]


