
Chest radiograph prevalence of vertebral deformity among young and middle-aged population of mixed city dwellers and rural residents
Introduction
The bone composition of the spine, which is predominantly trabecular bone, is more prone to the thinning and microarchitectural changes associated with osteoporosis than regions of the hip that are richer in cortical bone. Osteoporotic vertebral fracture (OVF) is the most common osteoporotic fracture. Assessment of OVF status, in addition to bone mineral density (BMD), provides important information to aid in predicting fracture risk in older women and men. Some ‘mild’ OVF can also be clinically relevant. Siris et al. (1) reported that at any given BMD T-score, the risk of incident vertebral, non-vertebral, and any fracture depended heavily on prevalent radiographic OVF status. Johansson et al. (2) reported that, in older women and after adjustment for clinical risk factors and BMD, Genant grade-1 OVFs identified on lateral spine imaging with dual-energy X-ray absorptiometry are associated with incident major osteoporotic fractures. In the Canada-wide STeroid-Associated Osteoporosis in the Pediatric Population (STOPP) study, Alos et al. (3) noted that the presence of Genant grade-1 vertebral fracture at baseline in children with leukemia was independently associated with an increased risk of new fractures in the first 12 months following chemotherapy initiation (3). OVF can be considered as a “gateway” to other more serious fractures, such as hip fracture (4,5). Some guidelines recommend spine imaging as a screening tool for osteoporosis (6,7). It is important to identify OVF, so that appropriate investigation, prevention, and treatment can be instigated, both for women and men.
Despite the importance of OVF, till today there is no consensus for radiographic diagnosis of OVF, particularly for more ‘milder’ grades of OVF (8-17). In the early ‘90s, Genant and colleagues at the University of California at San Francisco (UCSF), USA, proposed the semi-quantitative (SQ) grading scheme to evaluate OVF (18). Genant et al. (18) described mild OVFs have 20–25% height loss, and OVFs without achieving this threshold are classified as SQ grade-0.5. However, while for epidemiological studies, it is acceptable to only count those OVFs with ≥20% height loss as long as the criterion is clearly defined to allow inter-study comparison, in clinical practice OVFs with <20% vertebral height loss can be sometimes relevant (12,14,19-21). In our MsOS (Hong Kong) year-14 follow-up, out of 150 female participants, the small number of women were identified as having baseline minimal OVF (<20% height loss) had incident OVF risk similar to that of the subjects with baseline apparent OVF (i.e., ≥20% height loss), higher than female subjects without baseline OVF (21). In a recent study, we reported that more than 2/3 of the minimal radiographic osteoporotic wedgings with height loss of <20% had recognizable endplate depression on CT, thus suggesting these deformities were osteoporotic (22). In fact, for OVFs truly without a trauma incident, the fracture or vertebral deformity (VD) process may be a slowly progressive process without a distinct event. From this point of view, there is no distinct separation between elderly women without OVF and elderly women with mild OVF. Thus, diagnosing a woman to have mild OVF or not have an OVF would depend on the chosen criteria for OVF (17).
The term ‘short vertebra’ has been frequently discussed (23,24). We define short vertebrae as those with decreased vertebral anterior and middle heights, while without anterior wedging or bi-concave changes, i.e., middle height and anterior height are reduced to a similar extent (17,22). In addition, other apparent OVF mimics, such as apparent osteoarthritic changes, are excluded. In our recent report on elderly women, our limited experience suggests that, singular acquired short height vertebra is often associated with CT endplate depression and thus likely to be osteoporotic, while multiple acquired adjacent short height vertebrae are without CT endplate depression and are likely due to other causes such as degenerative changes (22). However, we admitted that more studies are required to confirm our finding.
In this study, using a convenient sample of young and middle-aged subjects who had lateral chest radiographs other than spine disorders, we try to answer the following questions: (I) Is minimal grade vertebral deformity uncommon among young and middle-aged women? (II) How often ‘short vertebrae’ are seen among young and middle-aged subjects? (III) How vertebrae in young and middle-aged men differ from those of women of similar age and at what age the differences start to appear? It was reported that the vertebrae of men may be physiologically more wedge-shaped than those of women (25,26). Threshold to define OVF in older men, which is different from the threshold to define OVF in older women, has been proposed (27-29). However, what is the best threshold to diagnose prevalent OVF among older men has not been reliably confirmed.
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of the First Hospital of Jiaxing (Approval No. 2022-LY-379), and individual consent for this retrospective analysis was waived. All patient data were from Jiaxing First Hospital, Zhejiang province, China. The hospital is a general hospital and located in Jiaxing, a medium-sized city in the economically developed eastern coast region of China. Conveniently, from the period of Jan 9 2018 to Jul 30, 2018, and the period of Jul 4 2021 to Apr 30 2022, we retrieved 417 female cases and 430 male cases who had chest digital radiographs (frontal view plus lateral view). The selection of cases was on a random basis but with a preference for the targeted age ranges. The patients were referred for chest radiography due to mild illness or routine healthcheck or as part of standard pre-surgery examinations. The indications were all other than spine disorders, trauma, malignancies, or metabolic disorders. Lateral radiographs of insufficient image quality or coverage did not include L1 vertebra were excluded. Vertebral T12 was identified according to the 12th pair of ribs, and then L1 was checked for its visibility. In addition, two male cases with ankylosing spondylitis were also excluded from further analysis. For women, included for final analysis were 97 cases aged ≤20 years (group 1, range: 7–20 years), 144 cases aged 21–34 years (group 2), 101 cases aged 35–44 years (group 3), and 66 cases aged 45–59 years (group 4), totaling 408 cases. For men, included for final analysis were 58 cases aged ≤20 years (group 1, range: 7–20 years), 150 cases aged 21–34 years (group 2), 70 cases aged 35–44 years (group 3), and 96 cases aged 45–67 years (group 4), totaling 374 cases. For the female cases, the top six indications for chest radiography were cough or sore throat (36.3%), chest pain or chest tightness (10.3%), fever (10%), breast benign lesions (8.2%), biliary system inflammation and/or stone (4.9%), and routine health check (3.6%). For the male cases, the top six indications for chest radiography were cough or sore throat (36.1%), fever (23.3%), chest pain or chest tightness (13.5%), routine health check (3.6%), biliary system inflammation and/or stone, or gallbladder polyps (2.9%), and ureter stone (2.2%). The patient population includes a mixture of local city dwellers, residents from surrounding rural areas, and a small portion of migrant workers. Based on the recorded home address, for those aged >20 years, 27.2% of the females had family roots from farming communities. Based on the recorded profession or the home address, for those aged >20 years it was estimated that 26.4% of the male cases had a history of being a farmer or physical laborer. For males aged ≥45 years and >60 years, 36.1% and 42.8% respectively had a history of being a farmer or physical laborer.
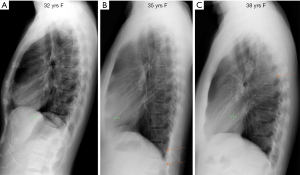
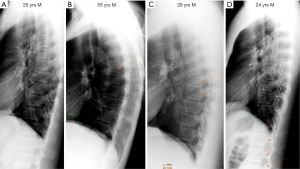
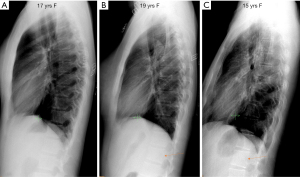
The lateral chest radiographs in DICOM format were initially read by a radiologist reader-A (YXJW), to identify all vertebral deformities (VDs), and frontal view radiograph was also checked when necessary. The existence of a deformity is mostly apparent (see examples in Figures 1,2), with a distinct deviation from the expected normal shape (though the extent of deviation might be mild). Congenital VDs were diagnosed based on their unique morphology (see three examples in the results part). Fracture shaped vertebral deformities (FSVDs) were VDs radiographically indistinguishable from vertebral fracture according to the best of the readers’ experience. Examples of fractural deformity have been extensively published (17-20,22,30-34). FSVDs was graded following the principles of the extended version semi-quantitative criteria (eSQ, 34). FSVD minimal grade was with less than 20% vertebral height loss, mild grade was with ≥20–25% vertebral height loss, moderate grade was with ≥25–33% vertebral height loss, moderately severe grade was with ≥1/3–40% vertebral height loss, severe grade was ≥40%–2/3 vertebral height loss, and collapse grade was ≥2/3 vertebral height loss. Endplate depression was recorded if existed (30,31). FSVDs were divided into biconcave shaped or non-biconcave shaped (no crush type of FSVD was noted in this study). By definition, biconcave shaped FSVDs had a certain extent of endplate depression, and middle height of a vertebra was more reduced. Non-biconcave shaped VDs had both anterior and middle heights reduced, mostly with anterior heights reduced to a greater extent, occasionally anterior height and mid height reduced to a similar extent (17,22). These FSVDs were classified as being wedged. A small portion of ‘mixed’ type VDs were noted to be a combination of wedging and anterior ‘stair-step’, while without endplate depression [explained in (17)]. These ‘mixed’ type VDs were considered the same as ‘wedged’ in this study. For the radiographs of subjects younger than 20 years, attention was made to those associated with pediatric vertebral development changes (33), and not considered them to be deformity.
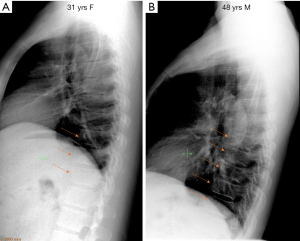
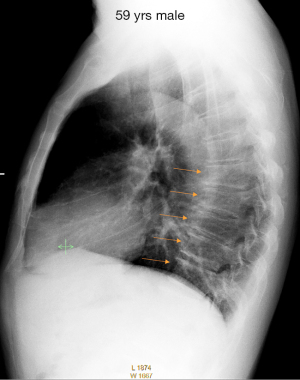
Short vertebrae were those with decreased vertebral anterior and middle heights, while without anterior wedging and bi-concave changes, i.e., middle height and anterior height were reduced to the same extent (22). Except for congenital short vertebra, in this study the diagnosis of ‘short vertebrae’ required at least two short vertebrae (and they were commonly adjacent) in the same subject (see examples in Figure 3). These vertebrae with short vertebral height would not include those with known causes such as degenerative osteoarthritis (OA). OA wedging was diagnosed according to Abdel-Hamid Osman et al. (35), typically appearing as anterior wedging involving more than one adjacent vertebra with similar appearance while without endplate depression (see an example in Figure 4), and can be associated with intervertebral disc space narrowing and formation of osteophytes (11,17,35).
The location of the VDs was recorded, with mid-thoracic region recorded as covering T6-T9 and thoracolumbar junction region recorded as covering T11-L2 (if L2 was visible).
A vertebral deformity index (VDI), which defines the overall number and severity of FSVDs visible on lateral chest radiograph, was calculated for each subject. For each vertebra, a score of 0, −0.5, −1, −1.5, −2, −2.5, and −3 was assigned for no FSVD or FSVD of <20%, ≥20–25%, ≥25%–1/3, ≥1/3–40%, ≥40%–2/3, and ≥2/3 vertebral height loss, respectively (21, 36). However, two adjacent minimal FSVDs were assigned as −0.5, and three adjacent FSVDs were assigned as −1 (36). VDI was calculated by summing up the scores of vertebrae T4 to the lowest visible vertebra.
The readings by the primary reader (reader-A) were then forwarded to the secondary reader (reader-B, JBM) for the second reading. Final consensuses were reached for all cases. Reader-A is considered to be very experienced in reading OVF, while Reader-B is an experienced general radiologist.
As this was not a study of stratified sampling with a predetermined statistical power, the results are presented descriptively. The focus was on observed trends rather on statistical significance.
Results
Congenital VDs were observed in four cases, including one case with block vertebrae (male, aged 35 years, Figure 5A) and three cases with congenital short vertebra [female, aged 18 years; male, 18 years (Figure 5B,5C); male, aged 27 years]. One case (female, age 30 years) was diagnosed with traumatic VD (with disc space narrowing and formation of large osteophytes). Other FSVD information is listed in Table 1, and the age-related trends are shown in Figure 6.
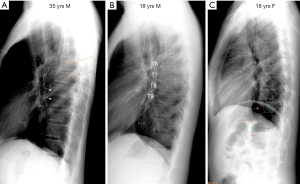
Table 1
| F/M | Groups [n] | Age (yrs), mean [range] | Prevalence, % [n] | Region-T/L# | Multi V# | ≥ mild, % [n] | ≥ mod, % [n] | Endplate D, % [n] | Biconcave, % [n] |
OA wedging, % [n] | Short V, % [n] |
|---|---|---|---|---|---|---|---|---|---|---|---|
| F | Group-1 [97] | 16.0 [7–20] | 13.4% [13] | 92.3% | 53.8% | 0 | 0 | 1.0% [1] | 1.0% [1] | 0 | 0 |
| Group-2 [144] | 29.4 [21–34] | 8.3% [12] | 75% | 16.7% | 0 | 0 | 1.4% [2] | 0.7% [1] | 0 | 1.0% [1] | |
| Group-3 [101] | 38.9 [35–44] | 11.8% [12] | 75% | 8.3% | 2.0% [2] | 0 | 2.0% [2] | 1.0% [1] | 1.0% [1] | 0 | |
| Group-4 [66] | 50.2 [45–59] | 25.8% [17] | 82.4%A | 29.4% | 12.1% [8] | 1.5% [1]B | 7.6% [5] | 4.5% [3] | 0 | 1.5% [1] | |
| M | Group-1 [58] | 15.9 [7–20] | 29.3% [17] | 88.2% | 52.9% | 1.7% [1] | 0 | 0 | 0 | 0 | 0 |
| Group-2 [150] | 28.1 [21–34] | 26% [39] | 92.3%C | 56.4% | 2.7% [4] | 0 | 0.7% [1] | 0 | 0.7% [1] | 0 | |
| Group-3 [70] | 38.7 [35–44] | 34.3% [24] | 79.2%D | 58.3% | 4.3% [3] | 1.4% [1] | 2.9% [2] | 1.4% [1] | 0 | 1.4% [1] | |
| Group-4 [96] | 54.1 [45–67] | 44.8% [43] | 79.1E | 58.1% | 22.9% [22] | 6.3% [6]B | 9.4% [9] | 3.1% [3] | 2.1% [2] | 15.6% [15]F |
In female group-2, one case (aged 30 years) had mild grade VD at T12, which was diagnosed to be traumatic deformity, T12/L1 disc space was narrowed together with adjacent osteophyte formation of L1. Congenital vertebral deformities are not listed in this table. #, percentage of the study cases with FSVD; A, one case had both mid-thoracic region and region-T/L involvement; B, one case with severe grade FSVD; C, three cases had both mid-thoracic region and region-T/L involvement; D, two cases had both mid-thoracic region and region-T/L involvement; E, four cases had both mid-thoracic region and region-T/L involvement; F, for those aged ≥60 yrs, prevalence was 21.7%. F: female; M: male; prevalence: prevalence of fracture shaped vertebral deformities (FSVD, all grades); Region-T/L: thoracolumbar region; multi V: more than one FSVD in one case; ≥ mild: FSVDs no less than mild grade (≥20% vertebral height loss), including those of moderate and severe grades; ≥ mod: FSVDs no less than moderate grade (≥25% vertebral height loss); Endplate D: FSVDs with endplate depression; Biconcave: FSVDs with biconcave shape; short V: acquired short vertebrae. OA, osteoarthritis.
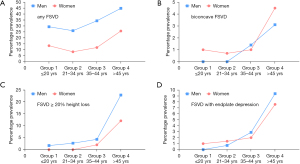
For the groups 1, females and males had FSVD prevalences of 13.4% (Figure 7) and 29.3%, respectively. The male-female difference was noted during the adolescent age. The youngest case to have FSVD was 12 years for females and 13 years for males. For the groups 2, females and males had an FSVD prevalence of 8.3% and 26%, respectively. From groups 1 to groups 2, there was no increase in FSVD prevalence, instead a reduction was observed for females. Also, from female group 1 to group 2, cases involving multiple vertebrae decreased from 53.8% to 16.7%. From groups 2 to groups 3, and from groups 3 to groups 4, an increase of FSVD prevalence was noted, both for females and for males (Figure 6). Particularly, in the male group 4, FSVD prevalence reached 44.8%. The most common location of FSVD was the thoracolumbar junction. For all age groups, not only FSVD prevalence was higher among males, FSVD was also more likely to be multiple among the males. Among the younger cases, males were more likely to have ≥ mild FSVD (Figure 6C). For cases ≤34 years, no female case had ≥ mild FSVD, while five male cases had ≥ mild FSVD. Among cases ≤44 years, endplate depression and biconcave FSVD were noted, though rare (Table 1, Figure 6B,6D). Among the group 4 subjects, endplate depression was noted among 7.6% of the females and 9.4% of the males.
Majority of FSVDs were wedged shaped (Table 1). A weak trend was noted that biconcave VDs were more common among females than among males (Figure 6B).
The VDI for non-zero cases are shown in Figure 8. For females younger than 50 years, none had a VDI score of less than −1 (Figure 8A). However, for males, VDI scores less than −2 were common (Figure 8B).

Acquired short vertebrae were rare except in the male group 4. Among the cases aged ≤44 years, there was only one male and one female had acquired short vertebrae. For the male cases, acquired short vertebrae prevalence was 15.6% in the group of >45 years which had a high proportion of physical laborers. Spine OA change was rare among our cases (Table 1).
Discussion
To address several questions we listed in the introduction, we reviewed the spine of a convenient sample of 408 women and 374 men who had lateral chest radiograph for indications other than spine disorders. A study of similar methodology as ours have been conducted by Yu et al. (37). In a study of later chest radiographs, Yu et al. noted that vertebral shape change was very rare among young subjects, and vertebral shape changes seen among older adults are less likely to be due to normal variation or congenital deformities. Yu et al. concluded that, mild or wedge-shaped vertebral body changes identified among adults should be managed as osteoporosis or at least considered as a risk factor for osteoporotic fracture. We conducted this additional investigation with a number of considerations. Yu et al. applied conventional Genant SQ criteria, it is unknown how the deformities of <20% vertebral loss were counted in their study. While the male-female differences in vertebral morphology have been recognized by earlier works, the work of Yu et al. did not emphasize this difference among the young and middle-aged subjects. In addition, Yu et al. noted that, after 70 years of age, the prevalence of vertebral fracture in men began to plateau, which differs from our experience. In our Hong Kong Chinese data, OVF prevalence increases exponentially with aging, both among older men and older women, with prevalence of OVF among women being approximately double of that of men (38).
Vertebral minimal wedgings with less than 20% height loss are commonly seen among older women. These wedgings, after excluding OVF mimics, could be classified as Genant grade-0.5 (18). However, Genant grade-0.5 is rarely reported, and how to address SQ grade-0.5 OVF has not been well addressed. To our knowledge, osteoporotic VDs without achieving the 20% height loss threshold have been commonly classified as Genant grade-1 OVF by colleagues trained in UCSF (17). We expect at least some of the minimal FSVDs in the current study would be reported as Genant grade-1 OVF by other readers. We argued that Genant grade-0.5 wedgings among older women mostly represent ‘mild’ OVF (17). To interpret the importance of minimal and mild VDs among elderly subjects, we need to know their prevalence in non-osteoporotic subjects. In this study, a high prevalence of FSVD was noted among adolescent cases, and FSVD was also more common among boys than among girls (Table 1). Note that, for subjects younger than 20 years, we already excluded the changes associated with pediatric vertebral development (33), and not counted them as deformity. We postulate our observed FSVDs were due to micro-fracture associated with physical stress. The location of these FSVDs was mostly at the thoracolumbar region, consistent with this region being under most external stress during spine movement. That boys had a higher FSVD prevalence than girls is consistent with boys being more often associated with physical stress and trauma. On the other hand, 86.6% of the girls and 70.7% of boys did not have any of these FSVDs on lateral chest radiograph according to our assessment. It is interesting that from female group 1 to group 2 there was a reduction of FSVD prevalence from 13.4% to 8.3%, and FSVD multiplicity from 53.8% to 16.7% (Table 1). A similar yet very weak trend was noted for males, from group 1 to group 2 FSVD prevalence changed from 29.3% to 26%. We suspect that these FSVDs can repair and heal. If none of the FSVDs repair, then from groups 1 to groups 2 we expect to see an increase of FSVD prevalence and multiplicity both for females and males. Indeed, in our clinical practice, we noted that minimal or mild VDs recovered to normal shape can be observed even among elderly subjects (Figure 9). Both Lauridsen et al. (25) and Matsumoto et al. (26) reported that vertebral shape was more physiologically wedged in men and in women. While we did not conduct a quantification on this aspect, our experience is that while wedge shaped vertebrae (i.e., minimal/mild FSVDs) were more common among men, for those vertebrae considered to be normal shaped, no apparent difference was noted between the vertebrae in women and vertebrae in men (Figures 1A,2A). Overall, our observations suggest that, if without micro-fracture, physiological vertebral body is not wedged at T4-L2 levels, i.e., while wedged vertebrae are a common observation among community population, the wedged shape of a vertebra is not physiological.

Though we did not have BMD status of our subjects, except for the female group 4, it is very unlikely that a substantial portion of our subjects had osteoporosis. For the point that FSVDs seen in female groups 1, 2, 3, and all males would be most likely due to micro-fracture, an analogy can be made to intervertebral disc degeneration (IVD). Differing from normal disc ageing, intervertebral disc degeneration is not congenital nor physiological. In the meaning time, IVD occurs at young age. Łebkowski (39) studied 308 lumbar discs taken during autopsy from 57 females (mean age 41.8 years) and 79 males (mean age 42.1 years). It was shown that 240 had degenerative changes. In males, degeneration occurs a decade earlier than in females, and was observed in the second decade of life. Takatalo et al. (40) studied the prevalence of lumbar IVD among young Finnish adults (325 women, 233 men) aged 20 to 22 years. IVD was significantly more frequent in men (54% vs. 42%). The prevalences of disc bulges and radial tears were 25% and 9.1%, respectively, without gender differences. Herniations were significantly more common among men (5.6% vs. 2.5%). It has also been well noted that, at the individual patient’s level, the association between IVD and clinical symptoms tends to be weak. However, at the group level or in statistical terms, IVDs are associated with clinical symptoms (41,42). In the current study, for the male group 2, all-inclusive FSVD prevalence was 26%, and mild FSVD prevalence was 2.7%. In contrast, there was no ≥ mild FSVD in the female group 2. FSVD prevalence was not very different between the female group 2 and group 3. Not surprisingly, FSVD prevalence and severity increased among the group 4 cases, both for females and males. The group 1 cases were mostly students, and with the recent development of economy in China, were unlikely involved in heavy physical labor. We also expect few of the cases in the female group 2 had heavy physical labor history. Their FSVD prevalence may represent ‘baseline noises’ for OVF assessment among the elderly. For the clinical significance of minimal wedging, it is highly likely that minimal wedging among young and middle-aged adults (<45 years) has little significance. However, it is expected among older women a large proportion of minimal FSVDs represent an osteoporotic phenomenon and may have clinical significance [(21) and our unpublished data of MsOS (Hong Kong) year-18 follow-up]. Our recent report suggests that, while minimal VDs in men likely have no long-term consequence, minimal VDs in women are more likely to be osteoporotic and associated with increased further fracture risk in the long term (21). Most of the FSVDs observed in this study were wedge shaped (Table 1). With European Prospective Osteoporosis Study subjects, for a mean follow-up of 3.8 years, Lunt et al. (43) reported relative OVF risk during follow-up differed according to the shape of the prevalent VD at baseline, ranging from 5.9 (95% CI: 4.1, 8.6) if the anterior and mid heights were reduced, 3.3 (2.3, 4.8) if the mid-height was reduced, and 1.9 (1.0, 3.4) if the anterior height was reduced. It is noted that the prevalence of biconcave FSVDs was not higher among men compared with that of women (Figure 6B).
Jiang et al. (44) proposed that all OVFs should demonstrate endplate fracture. However, radiograph is not a sensitive method to detect ECF, due to its resolution and due to the projectional overlay (15,17). In a recent study conducted among older women, we reported among 38 vertebrae in 27 cases which had anterior wedging deformity with height loss of <20% while without radiographic endplate depression, 28 vertebrae (28/38, 73.7%) demonstrated endplate depression on CT (22). We consider radiographic endplate depression as an additional sign of OVF, but radiographic endplate depression is not an essential sign of OVF (17). In the current study, endplate depression was also seen among cases in the female groups 1 and 2, and also among the male group 2, though the case number was few. Though we could not exclude the possibility that these cases had compromised bone strength, but it is more likely endplate depression (endplate fracture) can occur in subjects with normal bone strength. A vertebral endplate consists of perforated cortical bone with a layer of hyaline cartilage bonded to its disc surface. The cortical bone layer contains a network of small cavities which allow bone marrow to lie adjacent to calcified hyaline cartilage for approximately 10% of the central endplate area, which is an important route for metabolite transport into the discs. The nutritional demands of the discs result in that central vertebral endplates are thin and porous, and which can be subject to fracture under stress force even bone strength is normal. Among the group 4 subjects, endplate depression was noted among 7.6% of the females and 9.4% of the males. While some of the group 4 females could be osteoporotic, it is expected few of the group 4 males could be osteoporotic. We estimated that the senile osteoporosis prevalence based on lumbar BMD, femoral neck BMD, total hip BMD would be 2.0%, 3.8%, and 3.4% for Chinese male population aged ≥50 years (45). In fact, males younger than 60 years are unlikely to have primary osteoporotic fracture (29). Therefore, while endplate fracture or biconcave deformity is common among osteoporotic fractures, these may not be pathognomonic signs for OVF.
Due to the known non-osteoporotic vertebral wedging among men, more stringent criteria for the definition of OVF in men than in women have been suggested (29). Leidig-Bruckner et al. (46) applied an algorithm for radiological differential classification (RDC), and their RDC’s reading were compared with BMD measurement as well as morphometric criteria. They noted the agreement between RDC and morphometric methods was poor, and more so for elderly men than for elderly women. In men, 62–86% of cases with morphometric VD were classified by RDC as non-osteoporotic, compared with 31–68% in women. Leidig-Bruckner et al. suggested the criteria derived from women are likely to be unsuitable for men. Consistent with the general perception, FSVD was more common among male cases in this study. Our results in the current study further support more stringent criteria for the definition of OVF in men.
This study showed both congenital and acquired short vertebra(e) are rare among young and middle-aged subjects (<45 years). Acquired short vertebra could be an osteoporotic phenomenon or associated with OA (22). In a recent analysis of 46 female cases aged 67 to 94 years (mean: 76.7 years), we noted that acquired short vertebrae according to the definition in the current study was observed in four cases (8.7%). In the current study, a high prevalence of acquired short vertebrae was noted among the group 4 males, with 21.7% of those aged ≥60 years having acquired short vertebrae (Table 1). We suspect this phenomenon and the high prevalence of vertebral deformities seen among this group could be due to a high proportion of subjects were farmers and had a history of weight-bearing activities. However, we did not have longitudinal data to confirm this hypothesis. Spinal OA wedging also appeared to be uncommon among our study subjects.
There are several limitations to this study. We used lateral chest radiographs to evaluate vertebral body shape in our subjects as opposed to standard thoracolumbar radiographs. In our study, VD occurred from L3 and downwards could not be evaluated, L2 also could not be systematically assessed. However, with our earlier estimation, >70% of OVFs occur among vertebrae T4-L1 (36). Another limitation is that we used convenient samples of patients who visited a hospital, in theory how the results in this study can be generalised to the general population remain unknown. However, we expect that the characteristics of our patients would be largely similar to the general population in the local area. As noted in the method section, the patients visited a regional general hospital mostly for mild illnesses, and the complaints were unrelated to spine disease. One feature of our subjects is that, according to the estimation, for those aged >20 years, 27.2% of the females had family roots from farming communities, and 26.4% of the males had a history of being a farmer or physical laborer. For males aged ≥45 years and >60 years, 36.1% and 42.8% respectively (both according to estimation) had a history of being a farmer or physical laborers. Considering our own experience with MrOS (Hong Kong) and MsOS (Hong Kong) study subjects who were mostly city dwellers (21), we suspect this feature contributed to a somewhat higher FSVD prevalence among the cases in the current study. Since our results suggest higher ‘background noises’ of vertebral deformities among subjects being farmers or physical laborers, this point is relevant in real-world practice. On the other hand, we admit that the percentage of subjects who had the history of being a farmer or physical laborer was only based on approximate estimations. As this was a retrospective study, the estimations only considered the self-claimed profession and the home address. We could not quantify the amount or intensity of physical labours the study cases experienced. It was also possible that some of the farmers migrated to the city and later become office workers and city dwellers. Finally, as this study did not have a predetermined statistical power estimation, the results are presented descriptively, we avoided using statistical analysis. However, despite our sample size remains small, our sample size mostly addressed our study aims and the results appear to be reasonable.
In conclusion, in the age groups of ≤20 years, 20–34 years, 35–44 years, and ≥45 years (up to 59 years for women and 67 years for men), in this study women had all-inclusive FSVD prevalence of 13.4%, 8.3%, 11.8%, 25.8% respectively, while men had all-inclusive FSVD prevalence of 29.3%, 26%, 34.3%, 44.8% respectively. Our results support more stringent criteria for the definition of OVF in men than in women. Our results suggest, though not confirm, that FSVD may heal and repair, and physical labour is associated with an increased prevalence of FSVD.
Acknowledgments
Funding: None.
Footnote
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1386/dss
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1386/coif). YXJW serves as an unpaid editorial board member of Journal of Thoracic Disease from April 2022 to March 2024. YXJW is the founder of Yingran Medicals Ltd, which develops medical image-based diagnostics software. JBM has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of the First Hospital of Jiaxing (Approval No. 2022-LY-379), and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Siris ES, Genant HK, Laster AJ, et al. Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporos Int 2007;18:761-70. [Crossref] [PubMed]
- Johansson L, Sundh D, Magnusson P, et al. Grade 1 Vertebral Fractures Identified by Densitometric Lateral Spine Imaging Predict Incident Major Osteoporotic Fracture Independently of Clinical Risk Factors and Bone Mineral Density in Older Women. J Bone Miner Res 2020;35:1942-51. [Crossref] [PubMed]
- Alos N, Grant RM, Ramsay T, et al. High incidence of vertebral fractures in children with acute lymphoblastic leukemia 12 months after the initiation of therapy. J Clin Oncol 2012;30:2760-7. [Crossref] [PubMed]
- Kadowaki E, Tamaki J, Iki M, et al. Prevalent vertebral deformity independently increases incident vertebral fracture risk in middle-aged and elderly Japanese women: the Japanese Population-based Osteoporosis (JPOS) Cohort Study. Osteoporos Int 2010;21:1513-22. [Crossref] [PubMed]
- Black DM, Arden NK, Palermo L, et al. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res 1999;14:821-8. [Crossref] [PubMed]
- The Committee of the Japanese Society for Bone and Mineral Research for Development of Diagnostic Criteria of Osteoporosis. Diagnostic criteria of primary osteoporosis. J Bone Miner Metab 1998;16:139-50.
- Cheng X, Yuan H, Cheng J, et al. Chinese expert consensus on the diagnosis of osteoporosis by imaging and bone mineral density. Quant Imaging Med Surg 2020;10:2066-77. [Crossref] [PubMed]
- Szulc P. Vertebral Fracture: Diagnostic Difficulties of a Major Medical Problem. J Bone Miner Res 2018;33:553-9. [Crossref] [PubMed]
- Prior JC, Oei EHG, Brown JP, et al. Where's the break? Critique of radiographic vertebral fracture diagnostic methods. Osteoporos Int 2021;32:2391-5. [Crossref] [PubMed]
- Lentle BC, Prior JC. Osteoporotic vertebral fracture (OVF): diagnosis requires an informed observer. Osteoporos Int 2022;33:1409-10. [Crossref] [PubMed]
- Wáng YXJ. Osteoporotic Vertebral Deformity: Radiological Appearances and Their Association With a History of Trauma and the Risk of Further Fragility Fracture. Can Assoc Radiol J 2021;72:585. [Crossref] [PubMed]
- Sugita M, Watanabe N, Mikami Y, et al. Classification of vertebral compression fractures in the osteoporotic spine. J Spinal Disord Tech 2005;18:376-81. [Crossref] [PubMed]
- Diacinti D, Vitali C, Gussoni G, et al. Misdiagnosis of vertebral fractures on local radiographic readings of the multicentre POINT (Prevalence of Osteoporosis in INTernal medicine) study. Bone 2017;101:230-5. [Crossref] [PubMed]
- Wáng YXJ, Che-Nordin N. Some radiographically 'occult' osteoporotic vertebral fractures can be evidential if we look carefully. Quant Imaging Med Surg 2019;9:1992-5. [Crossref] [PubMed]
- Wáng YXJ. Osteoporotic vertebral endplate and/or cortex fracture is not always radiographically detectable. Osteoporos Int 2022;33:1407-8.
- Lentle B, Koromani F, Brown JP, et al. The Radiology of Osteoporotic Vertebral Fractures Revisited. J Bone Miner Res 2019;34:409-18. [Crossref] [PubMed]
- Wáng YXJ. An update of our understanding of radiographic diagnostics for prevalent osteoporotic vertebral fracture in elderly women. Quant Imaging Med Surg 2022;12:3495-514. [Crossref] [PubMed]
- Genant HK, Wu CY, van Kuijk C, et al. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993;8:1137-48. [Crossref] [PubMed]
- Pham T, Azulay-Parrado J, Champsaur P, et al. "Occult" osteoporotic vertebral fractures: vertebral body fractures without radiologic collapse. Spine (Phila Pa 1976) 2005;30:2430-5. [Crossref] [PubMed]
- Kim YJ, Chae SU, Kim GD, et al. Radiographic Detection of Osteoporotic Vertebral Fracture without Collapse. J Bone Metab 2013;20:89-94. [Crossref] [PubMed]
- Wáng YXJ, Che-Nordin N, Leung JCS, et al. Elderly men have much lower vertebral fracture risk than elderly women even at advanced age: the MrOS and MsOS (Hong Kong) year 14 follow-up radiology results. Arch Osteoporos 2020;15:176. [Crossref] [PubMed]
- Du EZ, Wáng YXJ. CT detects more osteoporotic endplate depressions than radiograph: a descriptive comparison of 76 vertebrae. Osteoporos Int 2022;33:1569-77. [Crossref] [PubMed]
- Ferrar L, Jiang G, Cawthon PM, et al. Identification of vertebral fracture and non-osteoporotic short vertebral height in men: the MrOS study. J Bone Miner Res 2007;22:1434-41. [Crossref] [PubMed]
- Ferrar L, Jiang G, Armbrecht G, et al. Is short vertebral height always an osteoporotic fracture? The Osteoporosis and Ultrasound Study (OPUS). Bone 2007;41:5-12. [Crossref] [PubMed]
- Lauridsen KN, De Carvalho A, Andersen AH. Degree of vertebral wedging of the dorso-lumbar spine. Acta Radiol Diagn (Stockh) 1984;25:29-32. [Crossref] [PubMed]
- Matsumoto M, Okada E, Kaneko Y, et al. Wedging of vertebral bodies at the thoracolumbar junction in asymptomatic healthy subjects on magnetic resonance imaging. Surg Radiol Anat 2011;33:223-8. [Crossref] [PubMed]
- Szulc P, Munoz F, Marchand F, et al. Semiquantitative evaluation of prevalent vertebral deformities in men and their relationship with osteoporosis: the MINOS study. Osteoporos Int 2001;12:302-10. [Crossref] [PubMed]
- Cawthon PM, Haslam J, Fullman R, et al. Methods and reliability of radiographic vertebral fracture detection in older men: the osteoporotic fractures in men study. Bone 2014;67:152-5. [Crossref] [PubMed]
- Wáng YXJ, Lentle BC. Radiographic osteoporotic vertebral fractures in elderly men: a brief review focusing on differences between the sexes. Quant Imaging Med Surg 2020;10:1863-76. [Crossref] [PubMed]
- Wáng YXJ, Santiago FR, Deng M, et al. Identifying osteoporotic vertebral endplate and cortex fractures. Quant Imaging Med Surg 2017;7:555-91. [Crossref] [PubMed]
- Wáng YXJ, Deng M, He LC, et al. Osteoporotic vertebral endplate and cortex fractures: A pictorial review. J Orthop Translat 2018;15:35-49. [Crossref] [PubMed]
- Du MM, Che-Nordin N, Ye PP, et al. Underreporting characteristics of osteoporotic vertebral fracture in back pain clinic patients of a tertiary hospital in China. J Orthop Translat 2020;23:152-8. [Crossref] [PubMed]
- Jaremko JL, Siminoski K, Firth GB, et al. Common normal variants of pediatric vertebral development that mimic fractures: a pictorial review from a national longitudinal bone health study. Pediatr Radiol 2015;45:593-605. [Crossref] [PubMed]
- Wáng YXJ, Diacinti D, Yu W, et al. Semi-quantitative grading and extended semi-quantitative grading for osteoporotic vertebral deformity: a radiographic image database for education and calibration. Ann Transl Med 2020;8:398. [Crossref] [PubMed]
- Abdel-Hamid Osman A, Bassiouni H, Koutri R, et al. Aging of the thoracic spine: distinction between wedging in osteoarthritis and fracture in osteoporosis--a cross-sectional and longitudinal study. Bone 1994;15:437-42. [Crossref] [PubMed]
- Wang YXJ, Diacinti D, Leung JCS, et al. Conversion of osteoporotic vertebral fracture severity score to osteoporosis T-score equivalent status: a framework and a comparative study of Hong Kong Chinese and Rome Caucasian older women. Arch Osteoporos 2022; In press. [Crossref]
- Yu W, Lin Q, Zhou X, et al. Reconsideration of the relevance of mild wedge or short vertebral height deformities across a broad age distribution. Osteoporos Int 2014;25:2609-15. [Crossref] [PubMed]
- Deng M, Zeng XJ, He LC, et al. Osteoporotic Vertebral Fracture Prevalence in Elderly Chinese Men and Women: A Comparison of Endplate/Cortex Fracture-Based and Morphometrical Deformity-Based Methods. J Clin Densitom 2019;22:409-19. [Crossref] [PubMed]
- Łebkowski WJ. Autopsy evaluation of the extent of degeneration of the lumbar intervertebral discs. Pol Merkur Lekarski 2002;13:188-90.
- Takatalo J, Karppinen J, Niinimäki J, et al. Prevalence of degenerative imaging findings in lumbar magnetic resonance imaging among young adults. Spine (Phila Pa 1976) 2009;34:1716-21. [Crossref] [PubMed]
- Brinjikji W, Diehn FE, Jarvik JG, et al. MRI Findings of Disc Degeneration are More Prevalent in Adults with Low Back Pain than in Asymptomatic Controls: A Systematic Review and Meta-Analysis. AJNR Am J Neuroradiol 2015;36:2394-9. [Crossref] [PubMed]
- Raastad J, Reiman M, Coeytaux R, et al. The association between lumbar spine radiographic features and low back pain: a systematic review and meta-analysis. Semin Arthritis Rheum 2015;44:571-85. [Crossref] [PubMed]
- Lunt M, O'Neill TW, Felsenberg D, et al. Characteristics of a prevalent vertebral deformity predict subsequent vertebral fracture: results from the European Prospective Osteoporosis Study (EPOS). Bone 2003;33:505-13. [Crossref] [PubMed]
- Jiang G, Eastell R, Barrington NA, et al. Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int 2004;15:887-96. [Crossref] [PubMed]
- Wáng YXJ, Xiao BH. Estimations of bone mineral density defined osteoporosis prevalence and cutpoint T-score for defining osteoporosis among older Chinese population: a framework based on relative fragility fracture risks. Quant Imaging Med Surg 2022;12:4346-60. [Crossref] [PubMed]
- Leidig-Bruckner G, Limberg B, Felsenberg D, et al. Sex difference in the validity of vertebral deformities as an index of prevalent vertebral osteoporotic fractures: a population survey of older men and women. Osteoporos Int 2000;11:102-19. [Crossref] [PubMed]


