
A retrospective study: do patients with left ventricular ejection fraction ≤50% benefit from heart valve surgery?
Highlight box
Key findings
• In patients with a low LVEF of ≤50%, cardiac surgery favors survival with significant improvement in cardiac systolic function compared to preoperative.
What is known and what is new?
• In some patients, a lower LVEF is a contraindication to heart valve replacement surgery and is associated with higher operative mortality and complications.
• The low LVEF group, moderate LVEF group and retention of LVEF group had similar degrees of postoperative valve anatomic recovery, with patients with lower LVEF showing more significant improvement in myocardial remodeling after heart valve surgery.
What is the implication, and what should change now?
• For patients with low LVEF, physicians should appropriately relax the range of indications for heart valve surgery and give aggressive surgical treatment.
Introduction
Left ventricular ejection fraction (LVEF) is calculated from end-diastolic volume (EDV) and end-systolic volume (ESV) measurements with the following formula: LVEF = (EDV − ESV)/EDV ×100%. LVEF is the most commonly used clinical index to evaluate LV systolic function, with normal values of 54–74% in women and 52–72% in men. In general, LVEF 40–50% is considered mildly reduced, 30–40% is considered moderately reduced, and <30% is considered severely reduced (1). Low LVEF reflects decreased cardiac function [decreased cardiac volume, elevated pro-brain natriuretic peptide (pro-BNP)], LV remodeling (enlarged LV, increased EDV and ESV, etc.), and carries a very high risk of perioperative surgery and postoperative mortality (2,3). In the Society of Thoracic Surgeons cardiac surgery risk model (STS-CSRM), a 10% reduction in LVEF was associated with a 1.09-fold increase in surgical mortality (4). The survival of patients with valvular heart disease (VHD; including aortic stenosis, aortic valve closure insufficiency, mitral stenosis, and mitral valve closure insufficiency) is impaired when LVEF <60%, so aggressive surgical procedures, especially surgical treatment of heart valves, are of great importance (5). Typically, LVEF ≤40% was previously considered a contraindication for heart valve surgery; however, with recent improvements in anesthesia and extracorporeal circulation techniques, as well as improved postoperative monitoring, more and more cardiac centers have relaxed the contraindications, allowing more patients with severe valvular disease and low LVEF to be effectively treated. Yammine et al. (6) found that in patients undergoing repeat aortic valve replacement (AVR), low LVEF (≤35%) was associated with increased operative mortality compared with LVEF >35% and the presence of renal insufficiency, resulting in very low cumulative survival. Macedo et al. (7) found that in patients with poor LVEF, the results of heart valve beating replacement surgery were similar to those using conventional heart surgery. Current studies on whether patients with low LVEF benefit from cardiac surgery have mostly focused on coronary artery bypass grafting (8,9), however, studies related to heart valve disease have not been elucidated. In addition, the exploration of low LVEF thresholds for patient benefit from surgery has rarely been reported.
As a result, this study evaluates the clinical efficacy of heart valve surgery in patients with VHD and low LVEF by means of a retrospective analysis, thus providing a basis for clinical practice. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1345/rc).
Methods
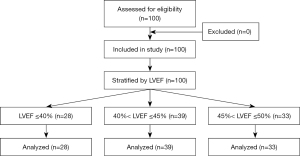
A total of 100 patients with VHD with low LVEF (≤50%) who had undergone valve surgery in the Department of Cardiothoracic Surgery of the First Affiliated Hospital of Guangxi Medical University from January 2019 to December 2021 were collected, including 69 males and 31 females. There were 97 cases with a median chest incision and 3 cases with a small right anterolateral incision assisted by thoracoscopy, and valve surgery was performed under general anesthesia with medium and low temperature extracorporeal circulation. AVR was performed in 46 cases, mitral valve replacement (MVR) in 33 cases, double valve replacement (DVR) in 31 cases. The patients had 20 MVRs and 28 tricuspid valvuloplasty. A total of 22 cases has a preoperative history of hypertension, 9 cases had a history of diabetes mellitus, 2 cases had a history of hyperthyroidism, 2 cases had a history of cerebral infarction, 39 cases had a history of smoking, 40 cases had a history of arrhythmia, and 37 cases had a history of pericardial effusion. Patients were divided into three groups according to LVEF measured by the last cardiac echocardiogram before surgery, with LVEF ≤40% for group A, 40%< LVEF ≤45 for group B, and 45%< LVEF ≤50 for group C. There were no statistically significant differences in the baseline clinical characteristics of the three groups. Due to the study design as an explorative pilot trial, no formal sample size calculation was performed. Figure 1 shows a flow chart of this study.
Inclusion and exclusion criteria
The inclusion criteria were based on patient history and signs, and all patients (age >18 years) had cardiac echocardiography receipts collected by two senior cardiac ultrasonographers at our hospital (The First Affiliated Hospital of Guangxi Medical University, Nanning, China) after outpatient and hospital admission, with a clear diagnosis of heart valve disease and two ultrasound findings suggesting LVEF ≤50%. Patients were excluded according to contraindications for surgery, otherwise they had undergone heart valve surgery. The ultrasound machine model used was the Philips IE33. The exclusion criteria were as follows: patients who were extubated with ventilator-assisted breathing before surgery; patients who had undergone concurrent coronary artery bypass grafting; patients who had undergone a second valve replacement; patients who had undergone nonstop valve replacement; and patients who had undergone valve interventions (e.g., transcatheter aortic valve implantation, transcatheter edge-to-edge repair technique).
Data collection
The patients’ clinical data were retrospectively analyzed. The general data included gender, age, height, body mass index (BMI), diabetes mellitus, hypertension, cerebrovascular disease, hyperthyroidism, smoking history, preoperative arrhythmia, combined pericardial effusion, New York Heart Association (NYHA) classification, and pro-BNP level. The collected surgical data included time of extracorporeal circulation, time of aortic block, intraoperative blood transfusion (red blood cells and plasma), and type of surgery. The postoperative clinical data included oxygenation index, albumin (ALB), total bilirubin (TBiL), supersensitive C-reactive protein (CRP), procalcitonin (PCT), maximal vasoactive drug score (VAS) on the first postoperative day, vasoactive-inotropic score (VIS), duration of postoperative ventilator use, length of stay in the care unit, and the use of an intra-aortic balloon pump (IABP). The echocardiographic measurements included cardiac output (CO), LVEF, left ventricle end-systolic dimension (LVESD), and left ventricle end diastolic dimension (LVEDD). The number of deaths of patients in the three groups was collected. All the patients who died from any cause during hospitalization after heart valve surgery and the patients who died outside the hospital after the family members of critically ill patients gave up treatment and signed for automatic discharge were classified as death cases.
Statistical analysis
SPSS 26.0 statistical software was used for data analysis, and the Kolmogorov-Smirnov test was used for each group to analyze whether the data conformed to the normal distribution. Measurement data conforming to the normal distribution were expressed as mean ± standard deviation. Differences between two groups were compared using the independent samples t-test, preoperative-postoperative comparisons were performed using the paired samples t-test, and comparisons between 3 or more groups were performed using ANOVA. Measurement data with a non-normal distribution were expressed as median M (P25, P75). Differences between two groups were compared using the two independent samples nonparametric test, and differences between 3 or more groups were compared using the multiple independent samples nonparametric test. Statistical data were expressed as composition ratio (%), and the chi-square test was used for comparisons between groups. Differences were considered statistically significant at P<0.05.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the First Affiliated Hospital of Guangxi Medical University [No. 2022-KY-E-(308)]. Individual consent for this retrospective analysis was waived.
Results
Comparison of baseline data among the three groups
According to LVEF grouping, there were 28 patients in group A, including 2 patients with 27%≤ LVEF <30%, 7 patients with 30%≤ LVEF <35%, and 19 patients with 35%≤ LVEF ≤40%. There were 39 patients in group B and 33 patients in group C. The preoperative baseline data including gender, age, height, BMI, diabetes mellitus, hypertension, cerebrovascular disease, hyperthyroidism, smoking history, preoperative arrhythmia, combined pericardial effusion, NYHA classification, and pro-BNP were compared and were not significantly different between groups (P>0.05). The proportions of patients with B-type natriuretic peptide precursor (pro-BNP) and NYHA class IV in group A were respectively higher than those in groups B and C, reflecting that the lower the LVEF, the more severe the disease and the worse the cardiac function (Table 1).
Table 1
| Clinical data | Group A (n=28) (LVEF ≤40%) |
Group B (n=39) (40%< LVEF ≤45%) |
Group C (n=33) (45%< LVEF ≤50%) |
H/F/χ² | P value |
|---|---|---|---|---|---|
| Gender (%) | |||||
| Female | 5 (17.86) | 15 (38.46) | 11 (33.33) | 3.36 | 0.186 |
| Male | 23 (82.14) | 24 (61.54) | 22 (66.67) | ||
| Age (year) | 51.25±8.54 | 52.95±11.34 | 53.12±11.42 | 0.283 | 0.754 |
| Height (cm) | 166.82±7.47 | 162.18±8.86 | 163.41±7.42 | 2.804 | 0.066 |
| BMI (kg/m2) | 22.338 (19.4, 25.0) | 21.484 (20.5, 23.5) | 22.471 (20.0, 25.8) | 0.399 | 0.819 |
| Diabetes (%) | 2 (7.14) | 4 (10.26) | 3 (9.09) | 0.193 | 0.908 |
| Hypertension (%) | 6 (21.43) | 7 (17.95) | 9 (27.27) | 0.913 | 0.633 |
| Cerebrovascular diseases (%) | 0 (0.00) | 1 (2.56) | 1 (3.03) | 0.813 | 0.666 |
| Hyperthyroidism (%) | 0 (0.00) | 1 (2.56) | 1 (3.03) | 0.813 | 0.666 |
| Smoking history (%) | 15 (53.57) | 11 (28.21) | 13 (39.39) | 4.411 | 0.11 |
| Preoperative arrhythmia (%) | 10 (35.71) | 17 (43.59) | 13 (39.39) | 0.429 | 0.807 |
| Pericardial effusion (%) | 6 (21.43) | 18 (46.15) | 13 (39.39) | 4.396 | 0.111 |
| NYHA (%) | |||||
| II | 12 (42.86) | 14 (35.90) | 9 (27.27) | 4.518 | 0.34 |
| III | 8 (28.57) | 18 (46.15) | 18 (54.55) | ||
| IV | 8 (28.57) | 7 (17.95) | 6 (18.18) | ||
| Pro-BNP (pg/mL) | 5,928.0 (2,336.0, 8,179.8) | 2,942.5 (1,429.0, 5,445.8) | 2,783.5(1,616.8, 4,360.0) | 5.116 | 0.077 |
LVEF, left ventricular ejection fraction; BMI, body mass index; BNP, brain natriuretic peptide; NYHA, New York Heart Association.
Comparison of intraoperative and postoperative data of the three groups
The time of extracorporeal circulation, time of aortic block, intraoperative blood transfusion (red blood cells and plasma), and type of surgery were compared among the three groups, and there were no statistically significant differences among the three groups (P>0.05). There were no statistically significant differences in the comparison of oxygenation index, ALB, TBiL, CRP, and PCT in the three groups of patients within 24 hours after surgery. Patients in group A had a higher maximal VIS on the first postoperative day, longer postoperative ventilator use, and longer time in the intensive care unit than patients in groups B and C. The rate of IABP was higher than in groups B and C respectively, but this was not statistically significant (P>0.05). The pro-BNP level on the first postoperative day was higher in group A than those in groups B and C, respectively. The comparison between each of the two groups was performed (P=0.024), indicating a statistically significant poorer postoperative cardiac function in group A patients in the early postoperative period. Group C had a higher mortality rate than groups A and B, but this was not statistically significant (P>0.05; Table 2).
Table 2
| Operation information | Group A (n=28) (LVEF ≤40%) |
Group B (n=39) (40%< LVEF ≤45%) |
Group C (n=33) (45%< LVEF ≤50%) |
H/F/χ² | P value |
|---|---|---|---|---|---|
| Cardiopulmonary bypass time (h) | 130.5 (112.3, 158.3) | 135.0 (92.0, 166.0) | 130.0 (95.5, 161.0) | 0.063 | 0.969 |
| Aortic occlusion time (h) | 98.36±35.84 | 98.51±33.43 | 97.85±49.36 | 0.003 | 0.997 |
| Red blood cells were transfused intraoperatively (U) | 0.75 (0.0, 2.0) | 0.0 (0.0, 2.0) | 0.0 (0.0, 2.5) | 0.163 | 0.992 |
| Intraoperative plasma transfusion (mL) | 400.0 (265.0, 467.5) | 370.0 (190.0, 420.0) | 400.0 (95.0, 465.0) | 0.88 | 0.644 |
| Operation type | |||||
| MVR (%) | 5 (17.86) | 13 (33.33) | 15 (45.45) | 8.144 | 0.086 |
| AVR (%) | 16 (57.14) | 15 (38.46) | 15 (45.45) | ||
| DVR (%) | 7 (25.00) | 11 (28.21) | 3 (9.09) | ||
| Oxygenation index | 327.64±107.14 | 308.25±132.69 | 312.22±181.50 | 0.155 | 0.857 |
| ALB (g/L) | 37.43±6.70 | 37.53±6.25 | 37.53±6.25 | 0.101 | 0.904 |
| TBiL (μmol/L) | 27.4 (20.4, 34.0) | 25.1 (17.0, 34.8) | 24.1 (16.6, 32.2) | 1.422 | 0.491 |
| CRP (mg/L) | 48.59 (10.0, 70.3) | 28.39 (11.6, 64.2) | 32.1 (14.1, 99.2) | 1.212 | 0.545 |
| PCT (ng/mL) | 19.28 (6.1, 31.4) | 13.18 (3.9, 24.2) | 18.05 (7.0, 66.1) | 3.315 | 0.191 |
| Pro-BNP (pg/mL) | 2,957.0 (1,592.0, 3472.0) | 1,088.0 (524.4, 2,849.0) | 1,580.0 (873.2, 2,983.0) | 7.5 | 0.024* |
| Postoperative day VIS max | 11.0 (10.0, 16.0) | 10.0 (8.0, 13.0) | 10.0 (8.0, 15.0) | 5.734 | 0.057 |
| Duration of ventilator use after surgery (h) | 30.0 (16.3, 74.3) | 25.0 (14.0, 47.0) | 24.0 (12.0, 49.5) | 1.051 | 0.591 |
| Length of stay in the care unit (h) | 86.75 (40.6, 155.0) | 62.0 (40.0, 85.1) | 47.21 (27.8, 73.8) | 5.492 | 0.064 |
| IABP (%) | 5 (17.86) | 2 (5.13) | 1 (3.03) | 5.241 | 0.073 |
| The number of deaths (%) | 1 (3.57) | 1 (2.56) | 3 (9.09) | 1.77 | 0.413 |
*, P<0.05. VIS = dopamine (μg/kg∙min) + dobutamine (μg/kg∙min) +10* millinone (μg/kg∙min) +100* epinephrine (μg/kg∙min) +100* norepinephrine (μg/kg∙min) +10,000* pituitrin (U/kg∙min). LVEF, left ventricular ejection fraction; MVR, mitral valve replacement; AVR, aortic valve replacement; DVR, double valve replacement; ALB, albumin; TBiL, total bilirubin; CRP, C-reactive protein; PCT, procalcitonin; BNP, brain natriuretic peptide; VIS, vasoactive-inotropic score; IABP, intra-aortic balloon pump.
Comparison of preoperative and early postoperative (within 48 hours) cardiac echocardiographic measurements in the three groups
When comparing the preoperative and early postoperative (within 48 hours after surgery) cardiac echocardiographic measurements of the three groups, patients in group A did not have significant CO changes (P=0.51). Patients in groups B and C showed a significant decrease in CO after surgery (P<0.001). LVEF increased, LVESD and LVEDD decreased, and ventricular remodeling significantly improved in all three groups compared with the preoperative period (P<0.001; Table 3).
Table 3
| Group | Cardiac ultrasound | Paired (mean ± standard deviation) | Difference value (pre-operation and within 48 hours after surgery) | P value | |
|---|---|---|---|---|---|
| Pre-operation | Within 48 hours after surgery | ||||
| Group A (n=28) (LVEF ≤40%) | CO (L/min) | 8.64±2.78 | 8.26±3.20 | 0.38 | 0.51 |
| EF (%) | 35.68±3.21 | 47.14±9.47 | −11.46 | <0.001 | |
| LVESD (mm) | 58.57±10.05 | 47.25±10.78 | 11.32 | <0.001 | |
| LVEDD (mm) | 71.43±11.34 | 62.14±10.97 | 9.29 | <0.001 | |
| Group B (n=39) (40%< LVEF ≤45%) | CO (L/min) | 8.43±3.23 | 7.00±2.33 | 1.43 | <0.001 |
| EF (%) | 43.23±1.39 | 51.38±9.44 | −8.15 | <0.001 | |
| LVESD (mm) | 50.92±9.21 | 40.77±10.78 | 10.15 | <0.001 | |
| LVEDD (mm) | 65.67±11.63 | 55.36±12.36 | 10.31 | <0.001 | |
| Group C (n=33) (45%< LVEF ≤50%) | CO (L/min) | 8.93±3.59 | 7.10±2.28 | 1.83 | <0.001 |
| EF (%) | 47.91±1.40 | 54.56±7.74 | −6.65 | <0.001 | |
| LVESD (mm) | 47.61±7.84 | 40.34±7.26 | 7.27 | <0.001 | |
| LVEDD (mm) | 64.27±9.99 | 55.03±9.18 | 9.17 | <0.001 | |
| All of the patients | CO (L/min) | 8.69±3.20 | 7.39±2.61 | 1.3 | <0.001 |
| EF (%) | 42.62±5.20 | 51.21±9.26 | −8.6 | <0.001 | |
| LVESD (mm) | 51.97±9.96 | 42.46±10.09 | 9.51 | <0.001 | |
| LVEDD (mm) | 66.81±11.31 | 57.17±11.29 | 9.64 | <0.001 | |
LVEF, left ventricular ejection fraction; CO, cardiac output; EF, ejection fraction; LVESD, left ventricle end-systolic dimension; LVEDD, left ventricle end diastolic dimension.
Comparison of preoperative and 3-month postoperative cardiac ultrasound measurements in the three groups
In the comparison of cardiac echocardiographic measurements before and 3 months after surgery in the three groups, CO was reduced and valve structure was significantly changed in all groups compared with before surgery (P<0.001), LVEF increased, LVESD and LVEDD decreased, and ventricular remodeling improved in all three groups compared with the preoperative period (P<0.001; Table 4).
Table 4
| Group | Cardiac ultrasound | Paired (mean ± standard deviation) | Difference value (pre-operation and 3 months after surgery) |
P value | |
|---|---|---|---|---|---|
| Pre-operation | 3 months after surgery | ||||
| Group A (n=28) (LVEF ≤40%) | CO (L/min) | 8.64±2.78 | 6.71±1.87 | 1.93 | <0.001 |
| EF (%) | 35.68±3.21 | 54.04±13.58 | −18.36 | <0.001 | |
| LVESD (mm) | 58.57±10.05 | 40.46±9.26 | 18.11 | <0.001 | |
| LVEDD (mm) | 71.43±11.34 | 56.32±7.15 | 15.11 | <0.001 | |
| Group B (n=39) (40%< LVEF ≤45%) | CO (L/min) | 8.43±3.23 | 6.63±2.09 | 1.8 | <0.001 |
| EF (%) | 43.23±1.39 | 53.82±12.55 | −10.59 | <0.001 | |
| LVESD (mm) | 50.92±9.21 | 39.95±13.37 | 10.97 | <0.001 | |
| LVEDD (mm) | 65.67±11.63 | 55.31±14.04 | 10.36 | <0.001 | |
| Group C (n=33) (45%< LVEF ≤50%) | CO (L/min) | 8.93±3.59 | 6.47±1.61 | 2.47 | <0.001 |
| EF (%) | 47.91±1.40 | 58.88±10.86 | −10.97 | <0.001 | |
| LVESD (mm) | 47.61±7.84 | 37.67±8.03 | 9.94 | <0.001 | |
| LVEDD (mm) | 64.27±9.99 | 55.18±7.13 | 9.09 | <0.001 | |
| All of the patients | CO (L/min) | 8.66±3.20 | 6.60±1.85 | 2.06 | <0.001 |
| EF (%) | 42.66±5.20 | 55.55±12.36 | −12.89 | <0.001 | |
| LVESD (mm) | 51.97±9.91 | 39.34±10.63 | 12.63 | <0.001 | |
| LVEDD (mm) | 66.82±11.25 | 55.55±10.26 | 11.27 | <0.001 | |
LVEF, left ventricular ejection fraction; CO, cardiac output; EF, ejection fraction; LVESD, left ventricle end-systolic dimension; LVEDD, left ventricle end diastolic dimension.
Comparison of preoperative and postoperative (within 48 hours and 3 months after surgery) cardiac echocardiographic measurements in each group
When comparing preoperative and postoperative (within 48 hours and 3 months postoperatively) cardiac echocardiographic measurements in each group, the preoperative CO in the three groups was not significantly different (P=0.81). The comparisons of LVEF, LVESD, and LVEDD among the three groups of patients showed statistically significant differences (P<0.05). In the early postoperative review of cardiac echocardiographic measurements, the comparison of CO among the three groups of patients showed no statistically significant difference (P=0.11). The comparisons of LVEF, LVESD, and LVEDD among the three groups of patients showed statistically significant differences (P<0.05). At 3 months postoperatively, cardiac echocardiographic measurements were repeated again, and a comparison of CO among the three groups of patients showed no statistically significant difference (P=0.87). The comparisons of LVEF, LVESD, and LVEDD among the three groups of patients were found to be P>0.05. There was no statistically significant difference between the three groups (Table 5).
Table 5
| Cardiac ultrasound | Group A (n=28) (LVEF ≤40%) |
Group B (n=39) (40%< LVEF ≤45%) |
Group C (n=33) (45%< LVEF ≤50%) |
F value | P value |
|---|---|---|---|---|---|
| Pre-operation | |||||
| CO (L/min) | 8.64±2.78 | 8.43±3.23 | 8.93±3.59 | 0.21 | 0.81 |
| EF (%) | 35.68±3.21 | 43.23±1.39 | 47.91±1.40 | 268.04 | <0.001** |
| LVESD (mm) | 58.57±10.05 | 50.92±9.21 | 47.61±7.84 | 11.58 | <0.001** |
| LVEDD (mm) | 71.43±11.34 | 65.67±11.63 | 64.27±9.99 | 3.54 | 0.03* |
| Early postoperative period (within 48 hours) | |||||
| CO (L/min) | 8.26±3.20 | 7.00±2.33 | 7.10±2.28 | 2.23 | 0.11 |
| EF (%) | 47.14±9.47 | 51.38±9.44 | 54.56±7.74 | 5.16 | 0.01* |
| LVESD (mm) | 47.25±10.78 | 40.77±10.78 | 40.34±7.26 | 4.69 | 0.01* |
| LVEDD (mm) | 62.14±10.97 | 55.36±12.36 | 55.03±9.18 | 3.98 | 0.02* |
| Three months after surgery | |||||
| CO (L/min) | 6.71±1.87 | 6.63±2.09 | 6.47±1.61 | 0.14 | 0.87 |
| EF (%) | 54.04±13.58 | 53.82±12.55 | 58.88±10.86 | 1.8 | 0.17 |
| LVESD (mm) | 40.46±9.26 | 39.95±13.37 | 37.67±8.03 | 0.62 | 0.54 |
| LVEDD (mm) | 56.32±7.15 | 55.31±14.04 | 55.18±7.13 | 0.11 | 0.9 |
*, P<0.05; **, P<0.01. LVEF, left ventricular ejection fraction; CO, cardiac output; EF, ejection fraction; LVESD, left ventricle end-systolic dimension; LVEDD, left ventricle end diastolic dimension.
Discussion
This is a single-center retrospective analysis comparing outcomes and survival after heart valve surgery in patients grouped by LVEF in 2 main ways. First, the outcomes of heart valve surgery in VHD patients with LVEF ≤40% were similar to those of VHD patients with LVEF >40%, with no statistically significant differences in time to extracorporeal circulation, time to aortic block, or intraoperative transfusion. There were also no statistically significant differences in the comparison of oxygenation index, ALB, TBiL, CRP, and PCT in the three groups within the 24 hours after surgery. A higher VIS score, postoperative ventilator use time, length of stay in the care unit, IABP use rate, and mortality rate on the first postoperative day reflected the disease is serious and difficult to treat, but were not statistically significant. The pro-BNP level on the first postoperative day was significantly higher in group A than those in groups B and C, reflecting the poor postoperative cardiac function and severe condition of group A patients. Second, by comparing the preoperative and postoperative (within 48 hours and 3 months after surgery) cardiac echocardiographic examinations of the three groups, we learned that the LVEF increased, LVESD and LVEDD were both smaller than before, and ventricular remodeling was improved after surgery. Furthermore, the lower the LVEF was, the more obvious the improvement was after surgery, and at 3 months after surgery, the LVEF of patients in each group reached about 55%. Three months after surgery, patients in each group had an LVEF of approximately 55%, LVESD of 39 mm, and LVEDD of 55 mm, with no statistically significant differences between the groups, reflecting the fact that patients with VHD with lower LVEF benefit more from heart valve surgery. Therefore, even in patients with low LVEF, heart valve surgery should be performed aggressively.
VHD is caused by stenosis and/or regurgitation of the heart valves due to multiple causes. In the early and middle stages of heart valve disease, the stenosis or regurgitation causes changes in heart chamber structure, intra-atrial chamber pressure, and intra-pulmonary vascular pressure, but myocardial contractility does not show a significant decrease, and clinical symptoms generally do not appear. In the middle and late stages, due to abnormal heart valve function, the corresponding neurohumoral regulation function causes changes in volume pressure load and abnormal myocardial structure or function, in which Myocardial cells and myocardial interstitial fibrotic changes, so that myocardial compliance decreases, local diastolic function decreases, resulting in progressive myocardial damage loss of compensation, myocardial remodeling further deteriorates, the late stage of valvular disease myocardial contractility decreases, which in turn causes changes in the overall systolic and diastolic function of the heart, the clinical manifestations are mainly left heart insufficiency, mostly manifested as a decrease in LVEF. At this time, the hemodynamic impact of valvular factors can aggravate the symptoms of heart failure, manifesting as cardiac cachexia, heart failure, and even death. Drug therapy cannot fundamentally address the problem of heart valve disease, and surgery is still the definitive and effective treatment. Valve replacement surgery is the surgical treatment for VHD and is indicated primarily on the basis of clinical symptoms and hemodynamic development. LVEF, the most commonly used clinical index for evaluating LV systolic function, is also an indication for surgery (10).
It has been suggested that lower LVEF is a key factor for poor prognosis, and patients with VHD and low LVEF tend to have enlarged left ventricles, increased myocardial remodeling, and existing irreversible pathological damage to myocardial cells, which predispose them to postoperative arrhythmias and low cardiac output syndrome, with high mortality and complications (11-14). In this study, there were no statistically significant differences between the three groups in terms of extracorporeal circulation time, aortic block time, intraoperative blood transfusion (red blood cells and plasma), and type of surgery, and no statistically significant differences in the comparison of oxygenation index, ALB, TBiL, CRP, and PCT in the three groups within 24 hours after surgery. These findings reflect that anesthesia, myocardial protection, extracorporeal circulation, and surgical techniques are mature and advanced technologies, and the risk of anesthesia and surgery is relatively lower in patients with lower LVEF. However, pro-BNP, maximal VIS, postoperative ventilator use time, and length of stay in the care unit were longer in group A than in patients in groups B and C on the first postoperative day, and the IABP use rate was higher than in patients in groups B and C. These findings indicate that patients in group A were sicker than patients in groups B and C, reflecting the difficulty of postoperative recovery and longer recovery time in patients with lower LVEF. This may be mainly due to the fact that heart valve surgery is a mature procedure in China, and the diagnosis and treatment techniques for heart valve disease have continued to improve in the last decade. First, with the continuous advances in echocardiography, CT, MRI, and imaging technologies, the diagnosis of VHD has become more accurate and preoperative assessment more established. Second, with the high incidence of VHD in China and the high number of surgeries each year, the clinicians' surgical techniques have become more skilled, and the improvement of surgical skills has optimized the aortic block time and extracorporeal circulation time, and the appropriate intraoperative treatment of valves has also promoted the recovery of cardiac function in patients after surgery. For example, the posterior valve tissue and subvalvular structures are preserved as much as possible during MVR (15,16). Continuous improvements in anesthesia, intraoperative myocardial protection, extracorporeal circulation, and postoperative monitoring, especially the use of IABP, extracorporeal membrane oxygenation, and other adjunctive devices, have led to smoother surgical management of heart valve disease. These improvements in treatment techniques have led to a gradual reduction in mortality.
There have been several studies of cardiac surgery in patients with low preoperative EF. In a study that included 485 patients with severe aortic valve closure insufficiency undergoing AVR, they were divided into three groups according to LVEF: the low LVEF group (LVEF ≤35%), moderate LVEF group (36%< LVEF <50%) and retention of LVEF group (LVEF >50%). Statistical analysis found that the operative mortality rate was 1.9%, with similar mortality rates between the groups (0% in the low LVEF group, 2.1% in the moderate LVEF group, and the LVEF group was 2.0%). The low EF group showed a large degree of postoperative reverse remodeling, with LV diameter at diastole decreasing from 6.7 to 5.1 cm in diastole and from 5.2 to 3.6 cm during contraction, and EF also improved significantly (mean 30% to 49.5%). The results showed that patients in the low LVEF group had similar postoperative outcomes and survival to those in the moderate LVEF group or the preserved LVEF group, and patients in the low LVEF group who underwent AVR developed postoperative LV reverse remodeling. This result suggests that reduced LVEF may not be a contraindication to surgery (17). Another study divided patients with severe aortic valve closure insufficiency with LVEF ≤35% into surgical and pharmacological groups. The mean follow-up time of the study cohort was 6.58 years and the mean survival of patients in the surgical group was 6.31 years, with a 1-year survival rate of 88%. The average survival time of patients in the medication group was 0.5 years, and a 1-year survival rate was 65%. The absolute mortality rate at the end of follow-up was 27.8% in the surgical group compared to 91.8% in the drug-treated group. These results indicate a large benefit of surgery in patients with low LVEF (18). This is a similar finding to other studies of MVR as well as minimally invasive valve replacement surgery (19-21). Overall, patients with VHD and low LVEF have severe perioperative disease and a difficult postoperative recovery, but surgical valve treatment over pharmacological treatment is beneficial for survival (22-26). This is identical to the data of the present study.
Previous studies have shown that heart valve surgery leads to myocardial reverse remodeling of the cardiac structure and improves the functional status of patients (17,27-29), and similar results were obtained in the present study. In the present study, preoperative and postoperative (within 48 hours and 3 months after surgery) cardiac echocardiographic measurements showed a decrease in CO in all groups compared with the preoperative period, it was considered that there was false high row due to anatomical changes before operation, and the valve anatomy was recovered after operation, when CO is true cardiac output and can accurately reflect cardiac function. However, there was no statistically significant difference in the comparison between the preoperative and postoperative groups (within 48 hours and 3 months after surgery), as the degree of recovery of valve anatomy after surgery was similar in all groups. The LVEF increased, LVESD and LVEDD decreased, and ventricular remodeling improved in all three groups compared with the preoperative period, and the lower the LVEF, the more pronounced the postoperative improvement. At 3 months postoperatively, LVEF increased to 55%, LVESD decreased to 39 mm, and LVEDD decreased to 55 mm in all groups, with no statistically significant differences between the groups, reflecting the fact that patients with VHD and lower LVEF had more significant improvement in myocardial remodeling and benefit from cardiac insufficiency after heart valve surgery.
In this study, the number of cases in group A was limited (the lowest LVEF was 27%, 2 cases were 27%≤ LVEF <30%, and 7 cases were 30%≤ LVEF <35%). The reasons for this are twofold: (I) valve interventions have been emerging in recent years and have brought great benefits to VHD patients with low LVEF (30), and our traditional nonstop valve replacement surgery also has some advantages in patients with low LVEF (31-33). Therefore, more surgical options are available for these patients; (II) the follow-up period of patients in this study was short, and the long-term results need to be further studied.
Conclusions
In conclusion, in patients with low LVEF, even though the perioperative period of valve surgery is severe and postoperative recovery is difficult, surgical treatment is beneficial for survival, and active surgical treatment should be considered. With the correction of valve anatomy, patients’ left ventricular volume was reduced and the systolic function of the heart significantly improved compared with the preoperative period.
Acknowledgments
Funding: This study was supported by the Scientific Research Project of Guangxi Health Commission (No. 20211014).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1345/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1345/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1345/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the First Affiliated Hospital of Guangxi Medical University [No. 2022-KY-E-(308)]. Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015;28:1-39.e14. [Crossref] [PubMed]
- Moreira JL, Barletta PHAAS, Baucia JA. Morbidity and Mortality in Patients Undergoing Mitral Valve Replacement at a Cardiovascular Surgery Referral Service: a Retrospective Analysis. Braz J Cardiovasc Surg 2021;36:183-91. [Crossref] [PubMed]
- Ibrahim KS, Kheirallah KA, Mayyas FA, et al. Predictors of short-term mortality after rheumatic heart valve surgery: A single-center retrospective study. Ann Med Surg (Lond) 2021;62:395-401. [Crossref] [PubMed]
- O'Brien SM, Shahian DM, Filardo G, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 2--isolated valve surgery. Ann Thorac Surg 2009;88:S23-42. [Crossref] [PubMed]
- Taniguchi T, Morimoto T, Shiomi H, et al. Prognostic Impact of Left Ventricular Ejection Fraction in Patients With Severe Aortic Stenosis. JACC Cardiovasc Interv 2018;11:145-57. [Crossref] [PubMed]
- Yammine M, Ramirez-Del Val F, Ejiofor JI, et al. Parsimonious assessment for reoperative aortic valve replacement; the deterrent effect of low left ventricular ejection fraction and renal impairment. Ann Cardiothorac Surg 2017;6:484-92. [Crossref] [PubMed]
- Macedo FI, Carvalho EM, Hassan M, et al. Beating heart valve surgery in patients with low left ventricular ejection fraction. J Card Surg 2010;25:267-71. [Crossref] [PubMed]
- Omer S, Adeseye A, Jimenez E, et al. Low left ventricular ejection fraction, complication rescue, and long-term survival after coronary artery bypass grafting. J Thorac Cardiovasc Surg 2022;163:111-19.e2. [Crossref] [PubMed]
- Galassi AR, Boukhris M, Toma A, et al. Percutaneous Coronary Intervention of Chronic Total Occlusions in Patients With Low Left Ventricular Ejection Fraction. JACC Cardiovasc Interv 2017;10:2158-70. [Crossref] [PubMed]
- Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021;143:e72-e227. [Crossref] [PubMed]
- Sathyamurthy I, Jayanthi K. Low flow low gradient aortic stenosis: clinical pathways. Indian Heart J 2014;66:672-7. [Crossref] [PubMed]
- Hatle L. How to diagnose diastolic heart failure a consensus statement. Eur Heart J 2007;28:2421-3. [Crossref] [PubMed]
- Stassen J, Ewe SH, Butcher SC, et al. Moderate aortic stenosis: importance of symptoms and left ventricular ejection fraction. Eur Heart J Cardiovasc Imaging 2022;23:790-9. [Crossref] [PubMed]
- Rizzello V. Moderate gradient severe aortic stenosis: diagnosis, prognosis and therapy. Eur Heart J Suppl 2021;23:E133-7. [Crossref] [PubMed]
- Besik J, Pirk J, Netuka I, et al. Aortic and Mitral Valve Replacement Due to Extensive Inflammatory Immunoglobulin G4-Related Pseudotumor. Ann Thorac Surg 2015;100:1439-41. [Crossref] [PubMed]
- Guo Y, He S, Wang T, et al. Comparison of modified total leaflet preservation, posterior leaflet preservation, and no leaflet preservation techniques in mitral valve replacement - a retrospective study. J Cardiothorac Surg 2019;14:102. [Crossref] [PubMed]
- Kaneko T, Ejiofor JI, Neely RC, et al. Aortic Regurgitation With Markedly Reduced Left Ventricular Function Is Not a Contraindication for Aortic Valve Replacement. Ann Thorac Surg 2016;102:41-7. [Crossref] [PubMed]
- Fiedler AG, Bhambhani V, Laikhter E, et al. Aortic valve replacement associated with survival in severe regurgitation and low ejection fraction. Heart 2018;104:835-40. [Crossref] [PubMed]
- Santana O, Xydas S, Williams RF, et al. Aortic valve replacement in patients with a left ventricular ejection fraction ≤35% performed via a minimally invasive right thoracotomy. J Thorac Dis 2017;9:S607-13. [Crossref] [PubMed]
- Mangoni AA, Koelling TM, Meyer GS, et al. Outcome following mitral valve replacement in patients with mitral stenosis and moderately reduced left ventricular ejection fraction. Eur J Cardiothorac Surg 2002;22:90-4. [Crossref] [PubMed]
- Santana O, Reyna J, Pineda AM, et al. Outcomes of minimally invasive mitral valve surgery in patients with an ejection fraction of 35% or less. Innovations (Phila) 2013;8:1-5.
- Micali LR, Algargoosh S, Parise O, et al. Patient survival in severe low-flow, low-gradient aortic stenosis after aortic valve replacement or conservative management. J Card Surg 2021;36:1030-9. [Crossref] [PubMed]
- Gunay D, Ozen Y, Cekmecelioglu D, et al. Effect of ejection fraction on left ventricular remodeling in aortic insufficiency. Asian Cardiovasc Thorac Ann 2016;24:332-6. [Crossref] [PubMed]
- Chaliki HP, Mohty D, Avierinos JF, et al. Outcomes after aortic valve replacement in patients with severe aortic regurgitation and markedly reduced left ventricular function. Circulation 2002;106:2687-93. [Crossref] [PubMed]
- Seese L, Sultan I, Gleason T, et al. Outcomes of Conventional Cardiac Surgery in Patients With Severely Reduced Ejection Fraction in the Modern Era. Ann Thorac Surg 2020;109:1409-18. [Crossref] [PubMed]
- Kamath AR, Varadarajan P, Turk R, et al. Survival in patients with severe aortic regurgitation and severe left ventricular dysfunction is improved by aortic valve replacement: results from a cohort of 166 patients with an ejection fraction < or =35%. Circulation 2009;120:S134-8. [Crossref] [PubMed]
- Toya T, Fukushima S, Shimahara Y, et al. Reverse left ventricular remodelling after aortic valve replacement for severe aortic insufficiency. Interact Cardiovasc Thorac Surg 2021;32:846-54. [Crossref] [PubMed]
- Bakkali A, Jaabari I, Dadji CK, et al. Results of aortic valve replacement in patients with aortic stenosis associated with severe left ventricular dysfunction. Pan Afr Med J 2018;29:79. [Crossref] [PubMed]
- Aithoussa M, Moutakiallah Y, Abdou A, et al. Surgery of aortic regurgitation with reduced left ventricular function. Ann Cardiol Angeiol (Paris) 2013;62:101-7. [Crossref] [PubMed]
- Koutsoukis A, Nahory L, Deguillard C, et al. Timing of aortic valve replacement in high-gradient severe aortic stenosis: impact of left ventricular ejection fraction. Acta Cardiol 2021;76:517-24. [Crossref] [PubMed]
- Lin F, He W, Liu TW, et al. Nonstop aortic valve or combined valve replacement. Chinese Journal of Thoracic and Cardiovascular Surgery 2002;18-20.
- Gersak B. Mitral valve repair or replacement on the beating heart. Heart Surg Forum 2000;3:232-7.
- Ghosh S, Jutley RS, Wraighte P, et al. Beating-heart mitral valve surgery in patients with poor left ventricular function. J Heart Valve Dis 2004;13:622-7; discussion 627-9.


