An 83 year old gentleman presented to the emergency department of a local hospital with a history of hemoptysis – two weeks duration – fatigue, loss of weight, shortness of breath and high grade fever. The patient, although taking warfarin for atrial fibrillation, discontinued this once hemopotysis was noted, with no effect. Further medical history of note included a history of hypertension on treatment, mild mitral regurgitation and previous right hemicolectomy for caecal carcinoma. Sputum sent for microscopy, culture and sensitivity by the general practitioner, four days prior to admission to a local Hospital, grew Klebsiella pneumoniae and Moraxella catarrhalis. In the light of the patient’s condition, the general practitioner trialed the patient on a course of Amoxicillin/Clavulanic acid and roxithromycin, based on the sensitivity report but with minimal effect.
On presentation, mild dyspnoea with movement was noted, peripheries were warm and well perfused with an elevated blood pressure and an irregularly irregular pulse rate below 100 beats per minute was observed. Breath sounds were diminished in the right lower zone with coarse inspiratory crepitations and increased tactile fremitus in the right posterior zones. The patient’s INR (international normalized ratio) on admission was 1.9.
Chest x-ray done on admission revealed consolidation of the right middle and lower lobes with an air fluid level in the right mid zone, and blunting of the right hemidiaphragm (
Fig 1). Findings were suspicious of empyema and it was decided to obtain computerized tomography (CT) of the thorax.
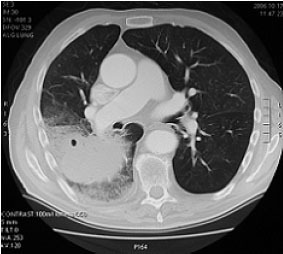
CT confirmed consolidation in the lateral and posterior basal segments of the right lower lobe and right middle lobe. A rounded opacity projected over the right mid-zone, lentiform in shape and compatible with being pleural in origin. An air fluid level at its medial aspect was typical of gas in the pleural space (
Fig 2). These findings were suggestive of pneumonia complicated by empyema. The patient was started on intravenous Cefuroxime and transfer to the Department Cardiothoracic Surgery, Wellington was organized for further management.
Rigid bronchoscopy together with right posterolateral thoracotomy were undertaken at Wellington Public hospital. Rigid bronchoscopy revealed an ulcer in the right main bronchus near the carina, most likely the cause of the hemoptysis. Bronchoscopic lavage was performed on this lesion and a specimen sent for cytology (no malignant cells noted).
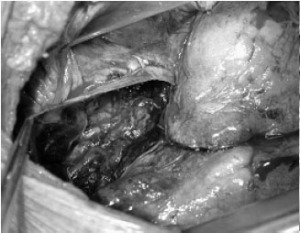
Right thoracotomy revealed a large hematoma in the fissure between the middle and lower lobes, contained beneath the visceral pleura of the lower lobe (
Fig 3). Extension of ecchymosis was noted all over the surface of the lower lobe. However, no further collections were seen anywhere else on the lower lobe. A smaller collection was also noted on the inferior surface of the right middle lobe.
Both collections were evacuated completely and no further ongoing bleeding recorded (
Fig 4,
Fig 5). The visceral pleura of the lower lobe were left open whereas air leaks on the middle lobe were sutured. Basal and apical drains were inserted and the chest was closed in layers. The patient was extubated and transferred to the recovery room.
The haematoma was cultured. However, there was no growth after 72 hours of incubation.
Post-operative recovery was unremarkable. The intercostal drains were removed on third post-operative day and the patient was discharged the day after. At the time of discharge, he was afebrile, his white cell count had returned to normal limits and the surgical wounds were healing well with no signs of infection/ inflammation. Considering the fact that the patient was old and the episode of haemoptysis and intra-thoracic haematoma, the warfarin therapy was discontinued and he was started on regular aspirin. Follow up was arranged with the referring physicians.
He was followed up six months after discharge at the local hospital. A chest X-ray done then showed complete resolution of his condition, according to the report.