
Mastery of chest wall reconstruction with a titanium sternum-rib fixation system: a case series
Highlight box
Key findings
• We found a simple, convenient and highly applicable method for chest wall reconstruction.
What is known and what is new?
• Titanium alloys have already been used in chest wall reconstruction.
• We summarized the reconstruction of various types of chest wall defects using titanium alloy materials.
What is the implication, and what should change now?
• The titanium sternum-rib fixation system can fulfill almost all the needs of reconstruction for large defects after various chest wall lesion resections. It is affordable and the satisfactory clinical outcomes support its wider application.
Introduction
Chest wall tumors are common thoracic surgery diseases, including primary chest wall tumors, metastatic tumors, and primary tumors directly invading the chest wall (1,2). Surgical resection remains the mainstay of treatment for chest wall tumors. Excessive chest wall defects will compromise the stability of the chest wall and result in chest wall deformity, paradoxical respiration, lung herniation, and restriction of pulmonary function. These conditions may undermine the treatment outcome. Thus, reconstruction is always a treatment challenge. In 1906, Tansini reported the first case of chest wall reconstruction with a latissimus dorsi muscle flap with a pedicle covering a defect in the anterior chest wall (3). With the advancement of materials technology, implants have increasingly been used in chest wall reconstruction. Their materials include titanium mesh, bone grafts, 3D printing materials, and various patches. Each implant has its own features, and one type may only fit a specific chest wall defect. Some need to be designed and prepared beforehand, and some are very expensive (4-8). Out of all the reports of chest wall reconstruction, there is no satisfactory, readily available, affordable material and method intended for various defects. In recent years, titanium alloys have been widely used in chest wall reconstruction due to the high strength, light weight, contourability, and good tissue compatibility (9,10). But most of the studies using titanium sternum-rib fixation system for reconstruction are case reports. None of the studies described in detail the reconstruction of various chest wall defects. Since 2016, in the Department of Thoracic Surgery, Shanghai Sixth People’s Hospital, we have applied a titanium sternum-rib fixation system combined with polyester mesh to reconstruct chest wall defects, and all chest wall defects have been successfully reconstructed and followed up.
Case presentation
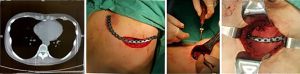
This is a retrospective study to investigate the application of titanium sternum-rib internal fixation system in reconstruction of various types of chest wall defects. The criteria for reconstruction are based on the size of the defect and practical clinical considerations, which are generally larger than 5 cm × 5 cm. Patients were followed up in the outpatient department between 1 and 3 months after surgery to observe postoperative recovery, including chest wall discomfort, chronic chest pain, chest wall deformity, stability (with or without displacement and loosening), and quality of life (time to return to daily life) to evaluate the efficacy and safety of surgery. Telephone follow-up was performed 3 months after surgery. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Shanghai Sixth People’s Hospital ethics committee [No. 2019-138-(1)]. Written informed consent was obtained from the patients for publication of this case series and accompanying images. A copy of the written consent is available for review by the editorial office of this journal. 93 patients with chest wall tumors treated at our center from January 2016 to January 2020. Among them, 57 patients underwent reconstruction using the titanium sternum-rib internal fixation system. Surgical resection was performed in all patients after complete examinations had been performed and surgical contraindications were excluded. During the operation, soft tissue margin samples were routinely taken for rapid frozen sectioning to ensure R0 resection. Whether chest wall reconstruction was needed was determined by defect size. A titanium sternum-rib fixation system was used in all bony reconstructions (Figure 1). Thoracic organs and implants were isolated by polyester meshes. Patients were followed up for at least 3 months after surgery to monitor chest wall appearance recovery, complications, stability (with or without displacement and loosening), quality of life, local recurrence, and survival.
Key considerations of surgical technique
Simple rib resection
Anterior chest wall
Tumor resection of the anterior chest wall adjacent to the costal cartilage tends to leave a large defect and has a higher impact on respiratory function because of the local anatomical features. In addition, this area is close to the organs and large vessels of the anterior mediastinal region. Therefore, we have a low threshold in anterior chest wall reconstruction to restore the stability of the chest wall and reduce respiratory complications. As required by the extent of surgical resection, the margin may be close to the junction of the rib and cartilage, and some cartilage may need to be removed. At this time, chest wall reconstruction techniques should be carefully considered. Due to the unstable anatomical characteristics of the rib-cartilage junction, when the margin is less than 2 cm from the rib-cartilage junction, reconstruction with a titanium plate fixed to the rib cortex by screws alone cannot guarantee stability. In addition, there are few studies specifically addressing fixation on costal cartilage. Thus, the data are not sufficient to clearly determine how stable internal fixation is on the costal cartilage and whether it will cause other complications. Therefore, based on our surgical experience of tumor resection and reconstruction adjacent to the costal cartilage of the anterior chest wall, it seems that the reconstruction material can be simply fixed to the rib cortex when the rib stump is longer than 2 cm. When the residual length is less than 2 cm, we have fixed one end of the reconstruction material to the sternum to ensure stability (Figure 2).
Lateral chest wall
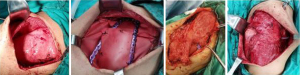
It is relatively simple to reconstruct the lateral chest wall after tumor resection, and enough bone stump can be retained at both ends of the margin for chest wall reconstruction. However, it is still tricky to select the right material for large defects and carry out the reconstruction in a straightforward and effective way. Figure 3 shows a rib tumor in which 6 ribs were removed. Chest wall reconstruction was carried out by using 3 titanium rib plates to reconstruct the bone structure combined with polyester mesh. When the resection involves the surrounding muscle and even skin, muscle flap transfer and skin flap transfer are required for soft tissue reconstruction to ensure wound healing and reduce the risk of infection.
Posterior chest wall or full-length rib resection
In cases of posterior chest wall tumors where the rib stump is already close to the transverse process after R0 resection, the remaining rib stump may not provide a good anchor point for stable fixation. When the lesion is too large or even involves the full length of the rib, anatomical reconstruction of the rib is not feasible. For this type of chest wall reconstruction, our aim is to restore the stability of the chest wall and avoid local chest wall deformity and paradoxical respiration caused by the large defect. We have fixed the reconstruction plate perpendicular to the ribs. In this study, we performed 2 operations in this way. No obvious chest wall deformity or constriction of breath was observed during the follow-up. This type of reconstruction seems feasible based on our current clinical observations and can also be used in patients with chest wall tumors below the sixth rib whose posterior margin of resection is adjacent to the costal cartilage, resulting in unstable fixation. However, whether this reconstruction technique compromises pulmonary function still needs further study.
Scapula and surrounding area
Chest wall reconstruction is indicated when the defect in the scapular area is larger than 10 cm. In our clinical observation, when the defect is located under the inferior angle of the scapula, it will cause sinking of the scapular angle and discomfort, even if the defect is small. In this study, 22 patients with chest wall defects in the scapular-covered area were divided into those with an inferior angle of the scapular area (ribs 5 to 7) and those with a noninferior angle of the scapular area. When the defect is located under the inferior angle of the scapula, we have a low threshold to reconstruct the chest wall, and the operation in this area is relatively simple and safe.
Sternal lesions
When the tumor is close to or directly invades the sternum, it is necessary to resect the partial or total sternum to ensure R0 resection. The titanium sternum-rib fixation system was used for cruciform reconstruction of the defect. The transverse reconstruction plate must be fixed on the rib stumps on both sides, and vertical reconstruction material should bridge the sternum stumps longitudinally. In this study, in 5 cases of sternal tumor resection and reconstruction, we retained part of the sternum as much as possible to provide stable fixation points for the reconstruction materials (Figure 4).

Sternoclavicular lesions
Sternoclavicular joints do not need to be reconstructed after tumor resection, although chest wall reconstruction may still be performed to ensure the stability of the chest wall in patients with large defects (Figure 5). Unreconstructed sternoclavicular joints did not affect the normal movement of the shoulder joints in our postoperative follow-up study (11).

In this study, a total of 57 patients underwent chest wall reconstruction with an average of 2.3 ribs removed. Table 1 shows the basic data of all patients. The reconstruction materials used in the 57 cases of chest wall reconstruction are listed in Table 2, including 10 cases involving sternotomy and reconstruction and 3 cases involving sternoclavicular joint resection and reconstruction. The follow-up time ranged from 3 months to 5 years, with an 86% follow-up rate (8 were lost to follow-up) (details in Table 3). Postoperative chest discomfort occurred in 6 patients during follow-up, and 2 patients had chronic pain. The average time to return to normal life was 1.4 months. One patient developed deformed depression of the chest wall, and 2 patients developed wound infections. A total of 4 patients developed recurrence and metastasis, 1 of whom was pathologically diagnosed with chondrosarcoma and died 2 years after treatment following metastasis to other sites. The remaining 3 patients with recurrence also developed metastases in other sites and are still under treatment and follow-up. No perioperative death was observed in the whole group.
Table 1
| Variables | Sample (n=57) |
|---|---|
| Average age (years) | 44.1 |
| Sex, n (%) | |
| Male | 35 (61.4) |
| Female | 22 (38.6) |
| Pathology, n (%) | |
| Malignant tumor | 31 (54.4) |
| Benign tumor | 26 (45.6) |
| Primary tumor | 50 (87.7) |
| Metastatic tumor | 7 (12.3) |
| Average number of-rib resection | 2.3 |
| Partial sternal resection, n (%) | 10 (17.5) |
| Sternoclavicular joint resection, n (%) | 3 (5.3) |
| Scapula and surrounding area, n (%) | 11 (19.3) |
| Under the inferior angle of scapula | 7 (12.3) |
| Noninferior angle of scapula area | 4 (7.0) |
| Average number of reconstructive plates per rib | 0.6 |
| Reconstruction involves costal cartilage, n (%) | 10 (17.5) |
| Reconstruction involved the sternum, n (%) | 13 (22.8) |
| Postoperative complications, n (%) | 2 (3.5) |
| Average length of hospital stay (days) | 12.3 |
| Follow-up cases, n (%) | 49 (86.0) |
| Perioperative death, n (%) | 0 (0.0) |
Table 2
| Reconstruction type | Number |
|---|---|
| Used one piece of reconstruction material, n (%) | 35 |
| One-rib resection | 22 (62.9) |
| Two-rib resection | 5 (14.3) |
| Three-rib resection | 6 (17.1) |
| Four-rib resection | 2 (5.7) |
| Used two pieces of reconstruction material, n (%) | 13 |
| Two-rib resection | 1 (7.7) |
| Three-rib resection | 10 (76.9) |
| Four-rib resection | 0 |
| Five-rib resection | 1 (7.7) |
| Six-rib resection | 1 (7.7) |
| Used three pieces of reconstruction material, n (%) | 1 |
| Six-rib resection | 1 (100.0) |
| Sternal tumor, n (%) | 5 |
| Resection range | |
| Bilateral resection of the 2nd to 5th costal cartilage and sternum | 3 (60.0) |
| Bilateral resection of the 3rd to 6th costal cartilage and sternum | 2 (40.0) |
| Reconstruction material | |
| Titanium sternum fixation system | 4 (80.0) |
| Titanium rib fixation system | 1 (20.0) |
| Sternoclavicular joint resection | 3 |
| Total | 57 |
Table 3
| Variables | Number (%) |
|---|---|
| Chest wall deformity | 1 (1.8) |
| Paradoxical respiration | 0 (0.0) |
| Postoperative complications | 2 (3.5) |
| Recurrence and metastasis | 4 (7.0) |
| Reconstruction material shift | 0 (0.0) |
| Chest discomfort | 6 (10.5) |
| Chronic pain | 2 (3.5) |
| Average time to return to normal life (month) | 1.4 (2.5) |
| Follow-up | 49 (86.0) |
| Lost to follow-up | 8 (14.0) |
| Death | 1 (1.8) |
Discussion
Chest wall reconstruction has always been a challenge for thoracic surgeons. It involves the reconstruction of the pleura, bone structure, and soft tissue separately (12). For bone reconstruction, titanium mesh, 3D-printed materials, and bone grafts are widely used in clinical practice. The advantage of 3D-printed materials lies in the modeling of the defect reconstruction site before surgery to produce preformed materials of the right proportions. During reconstruction, the original contour of the chest wall can be restored to the greatest extent when 3D-printed materials are used. However, due to its high cost, its clinical application has certain limitations (13). Bone grafting can provide perfect histocompatibility and avoid immune rejection. This technique is suitable for reconstruction with small local defects, but not for reconstruction with large or complex defects (14). In this study, a titanium sternum-rib fixation system with polyester mesh was used for various types of chest wall reconstruction. Titanium is among the metallic materials with the best histocompatibility. The curved undersurface of the titanium plate ensures free pressure on the periosteum and protects the blood supply. The titanium sternum-rib fixation system can be cut to fit the defect. It can be contoured easily while having considerable rigidity, so that it can effectively support the defective chest wall. Locking plates with threaded locking holes boast more scientific mechanical properties. The stable locking structure enables the reconstruction material to have excellent stability and sufficient rigidity and flexibility to fully adapt to the chest wall movement caused by respiration. Titanium plates will not affect computed tomography (CT), magnetic resonance imaging (MRI), or other examinations. None of the patients in this study experienced plate deformation or displacement. Polyester patches can cover a wide area, as they are highly durable, radiolucent, and easy to handle. They can be directly sutured on the surrounding tissues as a material for pleural reconstruction, chest cavity closure, and organ protection (15).
It is not necessary to reconstruct each rib in chest wall reconstruction. The point is to select appropriate reconstruction materials according to the tumor site and resection extent. Thus, the reconstruction operation should be justified and simplified. For simple rib lesion resection, the reconstruction technique of a titanium rib fixation system with polyester mesh can be selected. In our study, 35 lesions were reconstructed with 1 titanium rib plate to cover the defect of up to 4 ribs. Depending on the number and location of the ribs removed, defect reconstruction can be performed using only 3 titanium rib fixation systems when 6 ribs are resected. However, the titanium rib fixation system also has certain limitations. Being approximately 18 cm length, it is often not long enough to cover the defect after anterior wall resection for sternum tumors. Thus, in this case, the titanium sternum fixation system is often used in combination with the rib system. Due to its intended use, the titanium sternum plate is approximately 30 cm long and has higher strength. It is more suitable for reconstruction of large defects in the anterior chest wall. In this study, 5 patients with sternal tumor lesions underwent bilateral costal cartilage and sternum removal. A total of 4 costal cartilages and the corresponding sternum were removed, on average, on both sides. According to the size of the defect, the titanium sternal fixation system was selected for chest wall reconstruction in 4 patients, and the titanium rib fixation system was selected in 1 patient. Postoperative recovery was good in all 5 patients, without displacement, dislodgement, or other discomfort associated with reconstruction materials.
The extent of chest wall resection should be chosen individually, and reconstruction should be accomplished as simply as possible. Our experience is that we should respect the barrier function of the host tissue and retain as much of the healthy tissue as possible to simplify reconstruction. In this group of cases, for the lesions that did not penetrate the muscular layer or a certain layer of soft tissue, the adjacent muscles or tissues were preserved as much as possible, which greatly reduced the frequency of application of a transferred muscle flap or skin flap. This not only reduced the surgical trauma but also simplified the operation, and there was no short-term local recurrence during the follow-up. For bone tissue, especially the sternum, as much healthy bone structure as possible should be retained. If the sternoclavicular joint is not involved, it is recommended to keep as much of the sternum a part of the sternoclavicular joint as possible to provide a fixation point for the titanium plate. This also significantly simplifies the operation. The sternal angle is also an important structure (16). From the point of view of anatomy, there are 3 types of sternal angles: synovial joints, cartilage connections, and bony connections. These types can be distinguished on CT images. When the connection is a synovial joint or cartilage connection, this structure can serve as a natural barrier. If the tumor does not involve the articular surface, part of the sternal manubrium may be preserved to guarantee the stability of sternoclavicular joints and to facilitate titanium plate fixation.
Due to high population mobility, 8 patients were not followed up on time at 1 month after surgery. In the follow-up for the other 49 patients, 1 patient had a local depression deformity of the chest wall after surgery. The condition was explained by massive soft tissue resection and scar contracture after reconstruction of the chest wall. However, the patient had no paradoxical breathing during the follow-up period. Among the 2 patients with wound infection, 1 was due to massive soft tissue resection with high local tension, so that postoperative wound healing was difficult. The other was due to preoperative radiotherapy, which hardened the local skin and hindered postoperative wound healing. When determining the resection extent of soft tissue intraoperatively, R0 resection of the tumor should be ensured through rapid frozen sectioning. The physiological barrier of the muscular space matters. This can be used as the anatomical landmark for us to visually determine the resection extent during the operation and reduce the operation time. Second, for patients with large soft tissue defects, it is suggested that muscle flap coverage be applied by a plastic surgeon to achieve a satisfying appearance after reconstruction and reduce the postoperative wound infection rate. If the tumor invades the dermis, indicating wide skin resection, a skin flap may be used. In addition, during the follow-up, 6 patients had chest discomfort, including numbness around the incision and foreign body sensation in the surgical area, and 2 patients had chronic pain more than 3 months after surgery, which was considered to be caused by peripheral nerve injury in the surgical area and adverse reactions to implants. In the follow-up of the 2 patients with chronic pain, the patients only took intermittent oral nonopioid analgesics for pain control, without any hinderance to daily work or life caused by chronic pain.
For chest wall reconstruction surgery, a stable thoracic cage after surgery, no implant displacement, no obvious chest wall deformity, and no abnormal breathing are the basic evaluation indexes of the surgery. In this study, only 1 case of postoperative chest wall depression deformity was found among all the patients, so the success rate of reconstruction was 98%. Problems such as surgical operability and cost are secondary evaluation indexes. The titanium sternum-rib internal fixation system combined with polyester mesh has wider applicability than other reconstruction materials and can cope with various types of chest wall defects. Through the evaluation of the defect site during the operation, reconstruction of the chest wall with a defect area larger than 5 cm × 5 cm saves the use of reconstruction materials to a certain extent and further reduces the operation cost while ensuring the success of the operation.
Conclusions
In conclusion, we suggest that for chest wall lesions, surgery should be performed with the goal of maximal lesion resection and maximal preservation of the healthy tissue to simplify reconstruction. The titanium sternum-rib fixation system can fulfill almost all the needs of reconstruction for large defects after various chest wall lesion resections. It is ready to use, easy to cut and contour, and easily combined with polyester mesh. It is affordable and the satisfactory clinical outcomes support its wider application.
Acknowledgments
First and foremost, I (Yang Li) would like to thank all my teachers who have helped me to develop the fundamental and essential academic competence. My sincere appreciation also goes to the colleagues from Department of Thoracic surgery, Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University, who participated in this study with great cooperation.
Funding: The study was supported by Shanghai Sixth People’s Hospital (No. ynlc201908).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1686/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Shanghai Sixth People’s Hospital ethics committee [No. 2019-138-(1)]. Written informed consent was obtained from the patients for publication of this case series and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Colella S, Brandimarte A, Marra R, et al. Chest wall reconstruction in benign and malignant tumors with non-rigid materials: An overview. Front Surg 2022;9:976463. [Crossref] [PubMed]
- Khullar OV, Fernandez FG. Prosthetic Reconstruction of the Chest Wall. Thorac Surg Clin 2017;27:201-8. [Crossref] [PubMed]
- Tansini I. Sopra il mio nuovo processo di amputazione della mammella. Gazetta Medica Italiana 1906;57:141-2.
- Tamburini N, Grossi W, Sanna S, et al. Chest wall reconstruction using a new titanium mesh: a multicenters experience. J Thorac Dis 2019;11:3459-66. [Crossref] [PubMed]
- Dell'Amore A, Comacchio G, Ferrigno P, et al. Sternal allograft transplantation for anterior chest wall reconstruction after sternectomy. Multimed Man Cardiothorac Surg 2019; [Crossref]
- Cabral D, Leitão R, Gomes Rosa F, et al. CHEST WALL RECONSTRUCTION USING CUSTOMIZED NEO-RIBS: CASE REPORT. Port J Card Thorac Vasc Surg 2021;28:53-5. [Crossref] [PubMed]
- Bellia-Munzon G, Martinez J, Toselli L, et al. From bench to bedside: 3D reconstruction and printing as a valuable tool for the chest wall surgeon. J Pediatr Surg 2020;55:2703-9. [Crossref] [PubMed]
- Goldsmith I. Chest Wall Reconstruction With 3D Printing: Anatomical and Functional Considerations. Innovations (Phila) 2022;17:191-200. [Crossref] [PubMed]
- Danker SJ, Mericli AF, Rice DC, et al. Custom 3D-printed Titanium Implant for Reconstruction of a Composite Chest and Abdominal Wall Defect. Plast Reconstr Surg Glob Open 2021;9:e3885. [Crossref] [PubMed]
- Dai Z, Maihemuti M, Sun Y, et al. Resection and reconstruction of huge tumors in the chest wall. J Cardiothorac Surg 2022;17:116. [Crossref] [PubMed]
- Li Y, Gao E, Yang Y, et al. Is arthroplasty necessary after sternoclavicular tumor resection? J Thorac Dis 2019;11:3171-4. [Crossref] [PubMed]
- McCormack P, Bains MS, Beattie EJ Jr, et al. New trends in skeletal reconstruction after resection of chest wall tumors. Ann Thorac Surg 1981;31:45-52. [Crossref] [PubMed]
- Wu Y, Chen N, Xu Z, et al. Application of 3D printing technology to thoracic wall tumor resection and thoracic wall reconstruction. J Thorac Dis 2018;10:6880-90. [Crossref] [PubMed]
- Kaláb M, Karkoška J, Kamínek M, et al. Transplantation of allogeneic bone graft in the therapy of massive post-sternotomy defects - 6 years of experience with the method. Rozhl Chir 2016;95:399-406.
- Kilic D, Gungor A, Kavukcu S, et al. Comparison of mersilene mesh-methyl metacrylate sandwich and polytetrafluoroethylene grafts for chest wall reconstruction. J Invest Surg 2006;19:353-60. [Crossref] [PubMed]
- Ball M, Falkson SR, Adigun OO. Anatomy, Angle of Louis. 2022 Jul 25. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.



