Management of middle lobe veins during single-portal video-assisted thoracoscopic surgery lobectomy via the fifth intercostal approach (case series): why the subcarinal triangular right base angle is helpful
Highlight box
Key findings
• Our initial results suggest that utilization of the SCT-RBA approach to manage middle lobe vein in uniportal surgery is feasible, convenient, and safe. It can also facilitate the dissection of subcarinal lymph nodes.
What is known and what is new?
• The fifth intercostal space is frequently used in single-portal VATS. However, it is difficult to manage middle lobe vein and dissect subcarinal lymph nodes via this approach.
• We describe a new approach to manage middle lobe vein via fifth intercostal space and evaluate the short time effects, which suggest that our new approach is feasible, convenient and safe.
What is the implication, and what should change now?
• Our results supply a new optional method to manage middle lobe vein and dissect subcarinal lymph nodes. Further study should be performed to verify our initial results and evaluate the long-term efficiency with enlarged sample size and learning curve of this approach.
Introduction
Management of the middle lobe vein with a linear cutter/stapler via the fifth intercostal space during a single-portal video-assisted thoracoscopic surgery (VATS) is difficult due to the limited distance between the hilum and incision site, as well as obstruction by the bronchus and pericardium posterior. The success of the ligature-pulling method relies heavily on the surgeon’s experience. Some surgeons may use vascular clips for ligation, but there is a risk of the clips being dislodged, which will affect the subsequent surgical steps. Others choose the fourth or sixth intercostal space to facilitate the handling of the middle lobe veins, which incurs further difficulties through changing the intercostal approach. For example, it complicates the management of horizontal fissure which is not well differentiated via the fourth intercostal approach. The sixth intercostal approach increases the difficulty of upper mediastinal lymph node dissection. Here, we describe a new technique for managing the middle lobe veins during a uniportal VATS lobectomy via the fifth intercostal approach. To perform this technique, we define a new approach called subcarinal triangular right base angle (SCT-RBA), which facilitates the management of the middle lobe veins and the dissection of subcarinal lymph nodes without altering the intercostal approach. We present the following article in accordance with the AME Case Series reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-716/rc).
Case presentation
From January 2021 to January 2022, we retrospectively collected the case series of 7 consecutive patients who underwent single-portal middle lobe resection with systemic mediastinal lymph node dissection or sampling via our new technique in Department of Thoracic Surgery, Ruijin Hospital North Campus. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of Ruijin Hospital (No. 2022-247). Publication of this case series and accompanying images was waived from patient consent according to the Ruijin Hospital ethics committee.
All patients received enhanced chest computed tomography (CT) scans to evaluate clinical stage. Brain magnetic resonance (MR), abdominal CT, superficial lymph node ultrasound, and radionuclide bone scans were applied if the lesion of the patient was solid-dominant on the CT scan. A frozen-section analysis was performed to confirm the malignant disease, following which mediastinal lymph node dissection was allowed.
Participant characteristics are shown in Table 1. Four patients had ground-glass opacity (GGO)-dominant disease and three patients were solid-dominant. One of four GGOS patients was atypical adenomatous hyperplasia (AAH) confirmed by paraffin slice and the other patients were all stage I disease. One patient had immunoglobulin A (IgA) nephropathy and another patient experienced asthma, high blood pressure, coronary atherosclerotic heart disease, and had undergone coronary artery bypass grafting surgery 2 months ago.
Table 1
| Patient | Age (years) | Gender | Comorbidity | Nodule | cTNM | pTNM |
|---|---|---|---|---|---|---|
| 1 | 39 | M | N/A | GGO | T1aN0M0 | T1a(mi)N0M0 |
| 2 | 39 | M | N/A | GGO | T1bN0M0 | AAH |
| 3 | 65 | F | IgA nephropathy | GGO | T1aN0M0 | T1amiN0M0 |
| 4 | 66 | F | N/A | GGO | T1aN0M0 | T1amiN0M0 |
| 5 | 41 | F | N/A | Solid | T1bN0M0 | T1bN0M0 |
| 6 | 65 | M | N/A | Solid+GGO | T1cN0M0 | T2aN1M0 |
| T1bN0M0 | T1bN0M0 | |||||
| 7 | 70 | M | Post-CABG Asthma HBP | Solid | T1bN0M0 | T1N2M0 |
TNM, tumor, node, metastasis; N/A, not applicable; GGO, ground-glass opacity; AAH, atypical adenomatous hyperplasia; IgA, immunoglobulin A; CABG, coronary artery bypass grafting; HBP, high blood pressure.
The short-term surgical outcomes included operation time, blood loss, lymph nodes harvest, duration of drainage, postoperative hospitalization, complications, and mortality. We describe the approach utilized in our surgery as subcarinal triangular right base angle (SCT-RBA).
Concept of the SCT-RBA
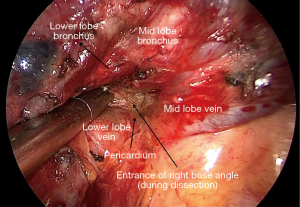
The SCT-RBA consists of two anatomical structures: the extent of the subcarinal triangle (SCT) and the location of the right basal angle (RBA). The SCT is a triangular area consisting of the right and left bronchi as well as the right and left inferior lobe veins. The RBA is the intersection of the right lower lobe bronchus and the right lower lobe vein, and the subcarinal area is just posterior to this base angle.
Borders of the SCT-RBA as viewed from the middle lobe pulmonary hilum
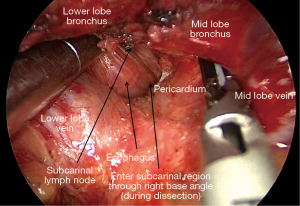
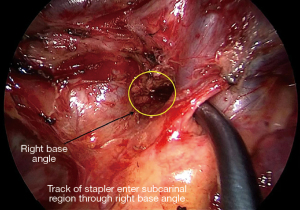
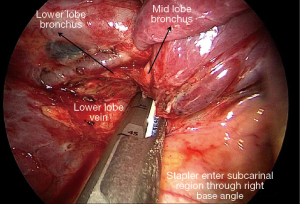
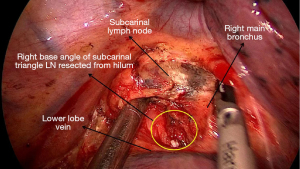
As single-portal right middle lobe resection is performed in the direction from the anterior pulmonary hilum towards the posterior mediastinum, the borders of the RBA can be clearly observed during the operation. The upper wall consists of the middle and lower lobe bronchi, the right wall consists of the middle lobe vein, the left wall consists of the lower lobe vein, and the lower wall consists of the pericardium (Figure 1). After the lymphoadipose tissues in this area are thoroughly removed, the subcarinal area can be accessed, with the anatomic landmarks being the subcarinal lymph nodes and the esophagus posterior to them (Figure 2). A stapler can be inserted into the subcarinal region through the RBA to manage the middle lobe veins (Figure 3).
Surgical technique and short-time effects
General anesthesia with a double lumen endotracheal tube was performed. Participants are positioned in the left lateral decubitus position. The selected surgical approach was a 3.5 cm uniportal incision established between the midaxillary line and the posterior axillary line in the right fifth intercostal space.
The surgery is divided into 3 steps, which can be reordered depending on the specific clinical settings (Video 1).
- The mediastinal pleura of the middle lobe pulmonary hilum is dissected to expose the middle lobe vein to a certain length. The middle and upper lobe veins are dissected to expose the right pulmonary artery and the right middle lobe bronchus, where the lymphoadipose tissues are resected.
- The oblique fissure between the middle and lower lobes is opened by using the “tunnel” technique. This step may be skipped if the oblique fissure is well developed.
- After the oblique fissure is opened, the middle and lower lobe bronchi are dissected to further expose the borders of the RBA approach. Dissection along the surface of the pericardium will allow access to the subcarinal area. The subcarinal lymphoadipose tissues should be thoroughly separated beginning from the pericardium until the esophagus is exposed, which indicates that the subcarinal area has been adequately mobilized (Figure 2).
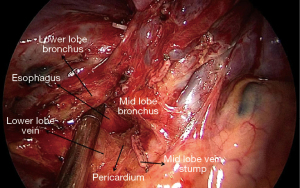
After the above steps having been performed, the cutter or stapler can be inserted above the middle lobe vein and enter the subcarinal area via the SCT-RBA approach to transect the middle lobe veins (Figures 4,5).
The clinical characteristics of patients are presented in Table 1 and the surgical outcomes are shown in Table 2. There were no conversion cases.
Table 2
| Patient | Operation time (min) | Blood loss (mL) | Lymph nodes harvest | Postoperative hospitalization (days) | Complications |
|---|---|---|---|---|---|
| 1 | 130 | 100 | 5 | 4 | N/A |
| 2 | 90 | 150 | 3 | 4 | N/A |
| 3 | 116 | 105 | 3 | 3 | N/A |
| 4 | 105 | 135 | 2 | 3 | N/A |
| 5 | 100 | 50 | 10 | 3 | N/A |
| 6 | 180 | 300 | 16 | 4 | N/A |
| 7 | 150 | 100 | 17 | 17 | Asthma |
| Air leakage | |||||
| Mean | 124.42 | 134.28 | 8 | 5.42 | N/A |
| Median | 116 | 105 | 5 | 4 | N/A |
N/A, not applicable.
The mean/median operation time was 124.42/116 minutes. Mean/median blood loss was 134.28/105 mL. Mean/median duration of drainage was 2.57/2 days. Mean and median postoperative hospitalization was 5.42/4 days. One patient had their chest tube removed on the fifth postoperative day (POD 5) and was discharged from the hospital on POD 17 due to the asthma and air leakage.
Four patients had GGO disease and we performed mediastinum lymph node sampling via frozen-sample testing. Three patients had solid-dominant disease and we performed mediastinum lymph node dissection and 10, 16, and 17 lymph nodes were obtained from these patients respectively. One of the three had two solid lesions in the right middle lobe. One patient had AAH disease while 3 patients had micro-invasive adenocarcinoma and 3 patients who had solid-dominant nodules on CT scan while undergoing mediastinal lymph node dissection were diagnosed with invasive adenocarcinoma.
Discussion
The single-portal approach has been widely used in anatomic lung resection surgery since it was first reported by Rocco (1) in 2004. The effect of anatomic lung surgery via the uniportal approach has been reported as comparable to that of conventional VATS. Guido-Guerrero et al. (2) reviewed the techniques of uniportal surgery, including lobectomy and segmentectomy, demonstrating that with the increase of surgeon experience, the operation time became comparable to that of the conventional VATS. A meta-analysis (3) updated in 2021 indicated a similar operative time, blood loss, and conversion rate between the uniportal surgery and multiportal VATS groups. Moreover, pain score was relatively lower in the uniportal VATS group. In addition, an ongoing prospective, randomized controlled study performed by Mendogni et al. (4) may provide more information about the surgical outcomes of different surgical approaches. Some studies have evaluated the learning curve of uniportal lobectomy or segmentectomy (5-8). The learning curve was divided into three phases and to achieve proficiency, a surgeon may be required to experience around 140 cases of lobectomy and 60–90 cases of segmentectomy.
We describe a new approach to manage middle lobe vein via a single port without changing the intercostal approach in 7 consecutive patients and illustrate the surgical outcomes of these patients to show the safety of our current approach. In our current study, the mean and median operation time were 124.42 and 116 minutes, respectively, which were consistent with that in some other studies shown in Table 3 (11,12,14-16). The similar operation time indicates that our new approach to managing the middle lobe vein does not complicate the surgical procedure. The safety of our approach is also acceptable, as the blood loss and postoperative outcomes (duration of drainage and hospitalization) were also comparable across other studies (9,11-16).
Table 3
| Studies | Cases enrolled | Operation time (min, mean) |
Duration of drainage (days, mean) |
Postoperative hospitalization (days, mean) |
Lymph nodes harvest (mean) |
|---|---|---|---|---|---|
| Paul et al. 2013 (9) | 10,173 | N/A | N/A | 5 | N/A |
| Kneuertz et al. 2019 (10) | 296 | N/A | N/A | N/A | 11.8 |
| Jin et al. 2022 (11) | 163 | 120 | 3 | 5 | 10 |
| Reddy et al. 2018 (12) | 838 | 222.6 | N/A | 6.6 | N/A |
| Hennon et al. 2020 (13) | 17,545 | N/A | N/A | 5 | 11.3 |
| Paul et al. 2010 (14) | 1,281 | 179.53 | 3.65 | 5.31 | N/A |
| Lee et al. 2015 (15) | 158 | 123 | N/A | 3 | 11 |
| Li et al. 2019 (16) | 85 | 100.1 | 4 | 5 | 10 |
N/A, not applicable. HBP, high blood pressure.
The evaluation of lymph nodes status is important for solid-dominant lesions. Three patients in our study underwent mediastinum lymph nodes dissection and the count of lymph nodes harvest were 10, 16, and 17 respectively, which were not inferior to the counts reported in previous studies (10,11,13,15,16), showing that the oncological efficacy can be ensured through our surgical approach.
A randomized control study performed by Bendixen et al. (17) demonstrated that VATS is associated with less pain and better quality of life than conventional thoracotomy for first year after surgery in stage I disease. Singer et al. (18) reviewed 15 studies and obtained similar results, although highly variable assessment of quality of life across enrolled studies. Superior short-term patient satisfaction and less pain are observed in single-port group from study conducted by Yoshifumi Sano and colleagues (19) compared with three-port VATS. Xu and colleagues (20) also prefer single-port VATS because of rapid recovery, less fatigue and pain, better short-term quality of life. However, the advantages of single-port VATS above are not observed in long-term follow-up (3-month after surgery) compared with three-port VATS in study performed by Ye et al. (21), which indicates the long-term quality of life effect is comparable between different intercostal incision on the premise of minimal invasive surgery and further prospective randomized control study should be performed to verify the result.
As the costal approach in our study is single-port (fifth costal space), the probable complications of our method are similar with conventional pulmonary surgery. Of note, with this method, it may cause accidental injury of the right inferior pulmonary vein. The prevention of accident is shown in video.
Zhang et al. (22) reported a novel technique to optimize uniportal mid-lobectomy, the incision of which was in the sixth intercostal space posterior to the scapular line. The technique facilitated the manipulation of the stapler. Nevertheless, we consider that a constant incision approach is important for surgeons to accumulate experience and master single-portal techniques.
Our study describes an optional method of single-portal middle lobectomy via the fifth intercostal approach for inexperienced surgeons and it facilitates dissection of the subcarinal lymph nodes. There were no intraoperative complications and conversion cases. One patient’s chest tube was removed on POD 5 and they were discharged from hospital on POD 17 after surgery because of air leakage and asthma, which may have been caused by comorbidity rather than the surgical approach used to manage the middle lobe vein.
The biggest advantage of our current method is facilitating the management of middle lobe vein via fifth costal space with single-port, which avoid the alteration of costal space approach to manage middle lobe vein.
Facilitating the subcarinal lymph nodes dissection is another advantage of our approach. As the subcarinal lymph nodes and periardium are separated when we dissect the RBA (right base angle), which can also resect the lymph nodes that are difficult to be exposed from posterior mediastinum locating at the entrance of RBA (under the intersection of middle and lower lobe bronchus) (Figure 6).
The risk of injuring lower lobe vein is main disadvantage of our method, the prevention of which is illustrated in the video and we regard it avoidable.
To use this approach, certain details should be noted:
- Resect lymph nodes and adipose tissue located in the right base angle to facilitate the exposure of the subcarinal region from the posterior mediastinum;
- The esophagus is a landmark that indicates the sufficient dissection of subcarinal region;
- Subcarinal lymph nodes and surrounding adipose tissue should be completely separated from the pericardium so that a stapler can enter the subcarinal region smoothly;
- If the anatomical structures (right base angle and subcarinal region) are not entirely exposed, the stapler may slip to the lower lobe and increase the risk of injury to the lower lobe structure;
As far as our knowledge, only some case reports described the technique of middle lobe vein management. We firstly evaluate the short-term effect and safety of our surgical approach. The main limitation of present study is the small sample size and absence of a control group.
Conclusions
Our initial results suggest that utilization of the SCT-RBA approach to manage middle lobe vein in uniportal surgery is feasible, convenient, and safe. It can also facilitate the dissection of subcarinal lymph nodes and avoid the change of surgical habits such as the incision approach. Further study should be performed to verify our initial results and evaluate the long-term efficiency with enlarged sample size and learning curve of this approach.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the AME Case Series reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-716/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-716/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of Ruijin Hospital (No. 2022-247). Publication of this case series and accompanying images was waived from patient consent according to the Ruijin Hospital ethics committee.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rocco G. One-port (uniportal) video-assisted thoracic surgical resections--a clear advance. J Thorac Cardiovasc Surg 2012;144:S27-31. [Crossref] [PubMed]
- Guido-Guerrero W, Bolaños-Cubillo A, González-Rivas D. Single-port video-assisted thoracic surgery (VATS)-advanced procedures & update. J Thorac Dis 2018;10:S1652-61. [Crossref] [PubMed]
- Magouliotis DE, Fergadi MP, Spiliopoulos K, et al. Uniportal Versus Multiportal Video-Assisted Thoracoscopic Lobectomy for Lung Cancer: An Updated Meta-analysis. Lung 2021;199:43-53. [Crossref] [PubMed]
- Mendogni P, Mazzucco A, Palleschi A, et al. Uniportal and three-portal video-assisted thoracic surgery pulmonary lobectomy for early-stage lung cancer (UNIT trial): study protocol of a single-center randomized trial. Trials 2021;22:163. [Crossref] [PubMed]
- Chen L, Pan Y, Zhang Q, et al. Learning Curve for Uniportal Thoracoscopic Anatomical Pulmonary Segmentectomy. Surg Innov 2020;27:378-83. [Crossref] [PubMed]
- Li S, Wu J, Wan Z, et al. The learning curve for uniportal video-assisted thoracoscopic anatomical segmentectomy. J Surg Oncol 2021;124:441-52. [Crossref] [PubMed]
- Vieira A, Bourdages-Pageau E, Kennedy K, et al. The learning curve on uniportal video-assisted thoracic surgery: An analysis of proficiency. J Thorac Cardiovasc Surg 2020;159:2487-95.e2. [Crossref] [PubMed]
- Drevet G, Ugalde Figueroa P. Uniportal video-assisted thoracoscopic surgery: safety, efficacy and learning curve during the first 250 cases in Quebec, Canada. Ann Cardiothorac Surg 2016;5:100-6. [Crossref] [PubMed]
- Paul S, Sedrakyan A, Chiu YL, et al. Outcomes after lobectomy using thoracoscopy vs thoracotomy: a comparative effectiveness analysis utilizing the Nationwide Inpatient Sample database. Eur J Cardiothorac Surg 2013;43:813-7. [Crossref] [PubMed]
- Kneuertz PJ, Cheufou DH, D'Souza DM, et al. Propensity-score adjusted comparison of pathologic nodal upstaging by robotic, video-assisted thoracoscopic, and open lobectomy for non-small cell lung cancer. J Thorac Cardiovasc Surg 2019;158:1457-66.e2. [Crossref] [PubMed]
- Jin R, Zheng Y, Yuan Y, et al. Robotic-assisted Versus Video-assisted Thoracoscopic Lobectomy: Short-term Results of a Randomized Clinical Trial (RVlob Trial). Ann Surg 2022;275:295-302. [Crossref] [PubMed]
- Reddy RM, Gorrepati ML, Oh DS, et al. Robotic-Assisted Versus Thoracoscopic Lobectomy Outcomes From High-Volume Thoracic Surgeons. Ann Thorac Surg 2018;106:902-8. [Crossref] [PubMed]
- Hennon MW, DeGraaff LH, Groman A, et al. The association of nodal upstaging with surgical approach and its impact on long-term survival after resection of non-small-cell lung cancer. Eur J Cardiothorac Surg 2020;57:888-95. [Crossref] [PubMed]
- Paul S, Altorki NK, Sheng S, et al. Thoracoscopic lobectomy is associated with lower morbidity than open lobectomy: a propensity-matched analysis from the STS database. J Thorac Cardiovasc Surg 2010;139:366-78. [Crossref] [PubMed]
- Lee BE, Shapiro M, Rutledge JR, et al. Nodal Upstaging in Robotic and Video Assisted Thoracic Surgery Lobectomy for Clinical N0 Lung Cancer. Ann Thorac Surg 2015;100:229-33; discussion 233-4. [Crossref] [PubMed]
- Li C, Hu Y, Huang J, et al. Comparison of robotic-assisted lobectomy with video-assisted thoracic surgery for stage IIB-IIIA non-small cell lung cancer. Transl Lung Cancer Res 2019;8:820-8. [Crossref] [PubMed]
- Bendixen M, Jørgensen OD, Kronborg C, et al. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol 2016;17:836-44. [Crossref] [PubMed]
- Singer ES, Kneuertz PJ, Nishimura J, et al. Effect of operative approach on quality of life following anatomic lung cancer resection. J Thorac Dis 2020;12:6913-9. [Crossref] [PubMed]
- Sano Y, Okazaki M, Shigematsu H, et al. Quality of life after partial lung resection with uniportal versus 3-port video-assisted thoracoscopic surgery: a prospective randomized controlled study. Surg Today 2021;51:1755-63. [Crossref] [PubMed]
- Xu GW, Xie MR, Wu HR, et al. A prospective study examining the impact of uniportal video-assisted thoracic surgery on the short-term quality of life in patients with lung cancer. Thorac Cancer 2020;11:612-8. [Crossref] [PubMed]
- Ye Z, Zhang B, Chen Y, et al. Comparison of single utility port video-assisted thoracoscopic surgery (VATS) and three-port VATS for non-small cell lung cancer. Oncol Lett 2019;18:1311-7. [Crossref] [PubMed]
- Zhang Hanlu, Yang Yu-Shang, Nong Kui, et al. A Novel Technique to Optimize Uniportal Thoracoscopic Right Middle Lobectomy. Ann Thorac Surg 2022;113:e303-5. [Crossref] [PubMed]