Failure of noninvasive ventilation in adult patients with acute asthma exacerbation
We read with interest the article entitled “Use of noninvasive ventilation in adult patients with acute asthma exacerbation” by Ganesh et al. (1). The authors have concluded that non-invasive ventilation (NIV) can be used initially in patients with acute asthma exacerbation, as it was associated with shorter duration of hospital stay and can prevent the morbidity of mechanical intubation. In this regard I would like to make the following observations.
In their study, Ganesh et al. (1) found that NIV failed only in 19% of all included patients (n=98). Patients who failed NIV were found to have longer duration of hospital stay (6.8 vs. 3.9 days, P=0.016) and longer intensive care unit stay (4 vs. 0.9 days, P=0.002). Use of inhalers and other medications was not found to significantly affect the rate of failure of NIV. However, the analysis of the included population leads to the following remarks.
First, the included population seems more likely a COPD than asthmatic population. In fact all clinical and biological characteristics: age of the included patients (48 vs. 50 years; P=0.58), history of smoking (78.5 vs. 78.9 pack-year), use of inhaled corticosteroids (50.6% vs. 42.1%), history of intubation and invasive mechanical ventilation (46.8 vs. 42.1) and bicarbonate serum level (27.3 vs. 28.3 mmol/L) were more suggestive of COPD rather than asthma. In this specific condition (COPD patients) noninvasive positive-pressure ventilation (here after, noninvasive ventilation) reduces the need for endotracheal intubation and mortality among patients with acute exacerbations of chronic obstructive pulmonary disease (2). The physiological effects of noninvasive ventilation consist on decreasing the load of work for breathing as well as improving gas exchange (2). Second, in successful NIV group, the FiO2 used was 20.42%; standard deviation (SD); lower and upper value; and median value were not mentioned. I would ask Ganesh et al. (1) why they used low FiO2 in order to treat a group of patient with respiratory failure requiring NIV (considered as asthma exacerbation). In fact, the included population was characterized by a severe impairment of gas exchange with a severe hypercapnia (54.4 mmHg) meaning that these patients had severe asthma attack (3). In fact, an asthma attack is usually characterized by compensatory hyperventilation inducing hypocapnia with respiratory alkalosis. Marked hypercapnia is synonym of severe asthma attack with respiratory failure requiring mechanical ventilation (3). Third, we would ask Ganesh et al. (1) what was the objective of NIV in their study? Is it mandatory ventilation? Supportive ventilation? prophylactic ventilation? or inhalator ventilation?
NIV has proven benefits in preventing invasive mechanical ventilation in acute exacerbation of COPD, acute pulmonary edema, as well as preventing reintubation of extubated COPD patients (2,4). However, its use during asthma attack is also controversial.
Asthma and COPD are the most prominent obstructive lung diseases and affect millions of people with an increasing incidence (5). However, there is some difference between COPD and asthma. In COPD disease, both the distal airways and lung parenchyma are affected by the disease and airflow limitation is progressive (5). However, in asthma only the airways are affected and, the remodeling process involves the whole bronchial tree, from large to small conductive airways (5).
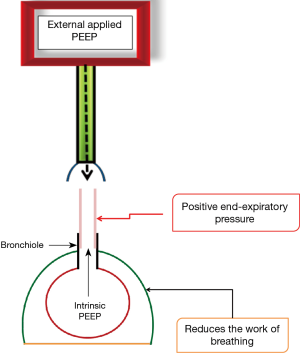
As a result, applying external positive end expiratory pressure (PEEP) to offset intrinsic PEEP might be of value in patients with COPD exacerbation. In fact, PEEP may improve ventilation/perfusion mismatch and gas exchange abnormalities, recruit collapsed alveoli, and reduce the work of breathing. Moreover, Respiratory and/or limb muscle dysfunction, which are frequently observed in chronic obstructive pulmonary disease (COPD) patients, contribute to their disease prognosis irrespective of the lung function (6,7). As consequence, pressure support on ICU ventilators or its equivalent inspiratory positive airway pressure (IPAP) on an external noninvasive positive pressure ventilation (NPPV) circuit has an additional advantage of reducing the respiratory load of work and lowering muscle fatigue (Figure 1).
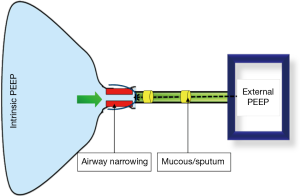
In asthma, the remodeling process involves the whole bronchial tree, from large to small conductive airways. In severe asthma, airway wall thickness was increased by between 50% and 230% (6). These changes result from airway inflammation with epithelial cell alterations, subepithelial fibrosis, submucosal gland hyperplasia, increased airway smooth muscle mass, and increased airway vascularization (8). These changes contribute to thickening airway walls and, consequently, airway narrowing, bronchial hyper-responsiveness, airway edema and mucous hypersecretion (8). Additionally, in acute exacerbations of asthma, bronchial smooth muscle contraction (bronchoconstriction) occurs quickly and increases airway obstruction. As consequence, during an asthma attack the patient may have difficulty coping with NIV, for several reasons.
First, severely dyspneic patients may not be cooperative, might resist to coordinate their breathing with the NIV machine and might therefore find NIV uncomfortable. Mucus production is a feature of severe acute asthma, and NIV can intensify sputum retention; and bronchial hyper-reactivity may be increased by the high inspiratory flow and airway dryness associated with NIV (Figure 2).
Second, the use of positive pressure in asthmatic patients can be associated with increased risk of barotraumas (9). Third, application of extrinsic PEEP in severe asthma could contribute to further dynamic hyperinflation. The combination of relative hypovolemia and excessively applied extrinsic PEEP may decrease venous return and expose the patient to the risk of hemodynamic compromise. Fourth, technical issues of NIV in severe acute asthma have not been clarified (bi-level pressure ventilation or continuous positive airway pressure?).
Fifth, asthma is characterized by reversible airway obstruction. In most patients, control of disease activity is easily achieved and in a small minority of patients, asthma may be fatal and/or requiring mechanical ventilation (10). Finally, there is limited evidence to recommend use of noninvasive positive-pressure ventilation in patients with respiratory failure from severe asthma exacerbations. In fact, only five randomized controlled trial (RCT) (11-15) including only a total of 206 patients were published and were subsequently analyzed in a recent meta-analysis (16). The review of these trials highlighted the paucity of data that exist to support the use of NIV status asthmaticus patients. In fact, no benefit was found when examining the primary outcomes—mortality and intubation rates—in patients who received NPPV. Regarding endotracheal intubation as primary outcome, there were two studies (14,15) that contributed data: two intubations were needed in 45 participants on NPPV and no intubations in 41 control patients with no evidence of an effect between groups [risk ratio (RR), 4.48; 95% CI, 0.23–89.13]. There were no deaths in either of these studies. Length of hospital stay was reported in two studies. Though meta-analysis was not possible. Hospitalization was reported in one small study (15), in which there were three admissions out of 17 on NPPV and 10 admissions out of 16 in control patients (RR, 0.28, 95% CI, 0.09–0.84). However, in this last study (15), although the study was blinded to the patients, a limitation of the study was that investigators did not succeed in blinding it from the investigating team. Regarding, the treatment failure, two studies reported on treatment failure (14,15) with 45 participants in the intervention group and 41 in the control. Overall, no statistically significant benefit was identified for this outcome on meta-analysis (RR, 0.73; 95%, CI 0.21–2.53).
We concluded that, there is limited evidence to recommend use of noninvasive positive-pressure ventilation in patients with respiratory failure from severe asthma exacerbation. Hence, this treatment remains controversial despite its continued use in current clinical practice. Larger, prospective RCTs of rigorous methodological design is needed to clarify when, where and why a trial of NIV may be attempted in severe asthma attack.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ganesh A, Shenoy S, Doshi V, et al. Use of noninvasive ventilation in adult patients with acute asthma exacerbation. Am J Ther 2015;22:431-4. [Crossref] [PubMed]
- Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 2015;372:2185-96. [Crossref] [PubMed]
- Scala R. Noninvasive ventilation in severe acute asthma? Still far from the truth. Respir Care 2010;55:630-7. [PubMed]
- Dalar L, Caner H, Eryuksel E, et al. Application of non-invasive mechanical ventilation in an asthmatic pregnant woman in respiratory failure: a case report. J Thorac Dis 2013;5:97-100. [PubMed]
- Dournes G, Laurent F. Airway Remodelling in Asthma and COPD: Findings, Similarities, and Differences Using Quantitative CT. Pulm Med 2012;2012:670414.
- Gea J, Pascual S, Casadevall C, et al. Muscle dysfunction in chronic obstructive pulmonary disease: update on causes and biological findings. J Thorac Dis 2015;7:E418-38. [PubMed]
- Erbabacan E, González Pérez MI, Koksal GM, et al. Protocolized weaning from mechanical strategy in chronic obstructive pulmonary disease: respiratory therapists versus physician directed-who guides best? J Thorac Dis 2015;7:E135-6. [PubMed]
- Shifren A, Witt C, Christie C, et al. Mechanisms of remodeling in asthmatic airways. J Allergy (Cairo) 2012;2012:316049.
- Caramez MP, Borges JB, Tucci MR, et al. Paradoxical responses to positive end-expiratory pressure in patients with airway obstruction during controlled ventilation. Crit Care Med 2005;33:1519-28. [Crossref] [PubMed]
- Leatherman J. Mechanical ventilation for severe asthma. Chest 2015;147:1671-80. [Crossref] [PubMed]
- Brandao DC, Lima VM, Filho VG, et al. Reversal of bronchial obstruction with bi-level positive airway pressure and nebulization in patients with acute asthma. J Asthma 2009;46:356-61. [Crossref] [PubMed]
- de Miranda AS, Silva COS, Beppa OS, et al. Non-invasive ventilation for continuous positive airways pressure (CPAP) assisted to the bronchodilator in the treatment of bronchial asthma crisis. Fisiotherapia em Movimento 2004;17:17-27.
- Filho VG, Rodrigues MM, Brandao D, et al. Coupling of noninvasive mechanical ventilation and nebulization during asthma exacerbations: higher amount of aerosol deposition into the airways or effective mechanical bronchodilation due to positive pressure? European Respiratory Society Annual Congress, Vienna, Austria, 2009.
- Gupta D, Nath A, Agarwal R, et al. A prospective randomized controlled trial on the efficacy of noninvasive ventilation in severe acute asthma. Respir Care 2010;55:536-43. [PubMed]
- Soroksky A, Stav D, Shpirer I. A pilot prospective, randomized, placebo-controlled trial of bilevel positive airway pressure in acute asthmatic attack. Chest 2003;123:1018-25. [Crossref] [PubMed]
- Lim WJ, Mohammed Akram R, Carson KV, et al. Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma. Cochrane Database Syst Rev 2012;12:CD004360. [PubMed]


