Concomitant off-pump coronary artery bypass grafting and total thyroidectomy for a large retrosternal goitre: a case report and review of the literature
IntroductionOther Section
Retrosternal goitre results when a proportion of at least 50% of the thyroid gland descends into the mediastinum. The documented incidence ranges from 0.02–0.5% in the general population and 2.6–21% in thyroidectomy patients, accounting for 3–12% of all mediastinal tumours (1,2). Clinical presentation may be associated with manifestations of thyroid dysfunction, as well as tracheal and oesophageal compression symptoms. Sternotomy is the indicated surgical approach if the retrosternal portion is large, thyroid tissue extends below the level of the aortic arch, invasive malignancy is likely or confirmed, or if there is existing adherence to surrounding mediastinal structures (3,4).
Thyroid disease affects cardiovascular physiology, presenting in up to 11% of patients with coronary artery or valvular heart disease (5). Whilst concomitant cardiac and thyroid procedures have been discussed in literature, no consensus exists regarding the optimal surgical management of such cases. Herein, we present a case of simultaneous off-pump coronary artery bypass grafting (OPCABG) and total thyroidectomy, followed by a review of the current literature on this subject. It is our view that in patients displaying severe cardiac ischaemia in conjunction with retrosternal goitre, concomitant CABG and thyroidectomy is the treatment of choice.
Case presentationOther Section
A 76-year-old male presented with sudden onset precordial pain. Relevant past medical history included angina pectoris (Canadian Cardiovascular Society Grade I) and dyspnoea (New York Heart Association Functional Class III). In addition, the patient suffered from stage III chronic kidney disease, type 2 diabetes mellitus, hyperlipidaemia and severe bilateral knee osteoarthritis. Previous procedures included transurethral resection of the prostate and bilateral inguinal hernia repair. With respect to social history, he was a lifelong non-smoker.
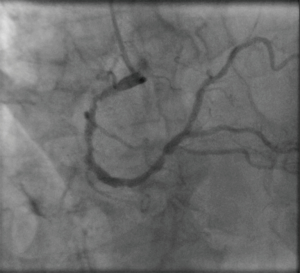
On admission, electrocardiogram showed new left bundle branch block, with troponin level within normal range. The patient underwent coronary angiography with the following findings: The left main stem (LMS) had no significant disease, but was calcified. The left anterior descending artery (LAD) was 80–90% proximally occluded, with a severe lesion in the large first diagonal branch and a less severe lesion located distally. The left circumflex artery had a severe proximal occlusive lesion just before the first obtuse marginal branch (Figure 1). The right coronary artery (RCA) was diffusely diseased with a 40–50% lesion in the mid-vessel and an 80–90% occlusion before the crux (Figure 2). A left ventricular angiography demonstrated anterior wall hypokinesis and moderately impaired left ventricular function.

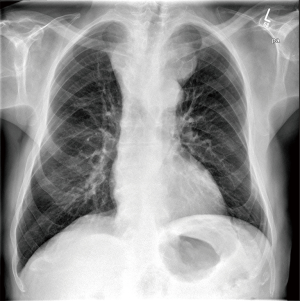
Chest radiograph had revealed superior mediastinum enlargement (Figure 3) and a subsequent CT scan of neck, chest and abdomen showed a large, calcified, multinodular goitre descending into the posterior mediastinum to the level of the carina. It displaced the great vessels, trachea and oesophagus to the right, compressing both of the latter structures (Figure 4). Pulmonary function tests revealed forced expiratory volume in 1 second (FEV1) 117%, forced vital capacity (FVC) 122% and peak expiratory flow rate (PEFR) 79%.

Due to the goitre location, a cardiac procedure with endocrine surgical input was planned. Preoperative assessment revealed left recurrent laryngeal nerve palsy and thyroid function tests showed euthyroid state. EuroSCORE values were an additive score of 9 and a logistic score of 13.71. A Parsonnet score of 19 (hard data) was determined.
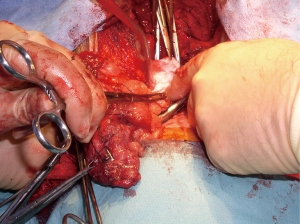
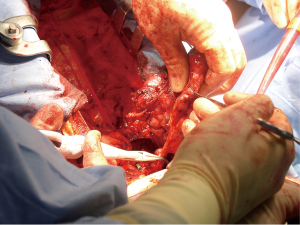
The patient underwent concomitant OPCABG ×2 with total thyroidectomy, with the endocrine component of the operation performed first. A median sternotomy incision was made, to which a subsequent 6 cm transverse incision was joined to form a ‘T’ shape. Following division and lateral retraction of strap muscles, each thyroid lobe was approached separately and excised with division of the isthmus (Figures 5,6). After ligation and division of the superior thyroid vessels, the upper pole was mobilised. The superior parathyroid glands were identified and fully preserved. No middle thyroid vein was visualised. The lower pole was mobilised in a corresponding manner. Separation of the thyroid from the trachea, oesophagus and surrounding structures was then completed. Due to a difficult anatomical dissection, damage was incurred to both recurrent laryngeal nerves.
An intra-aortic balloon pump was inserted prior to the cardiac aspect of the operation. No cardiopulmonary bypass or cross-clamping of the aorta was implemented and the core temperature was sustained at 37 °C. Only 1 mg/kg body weight of heparin was administered intravenously, in order to minimise bleeding from the extensive raw mediastinal surfaces. Saphenous veins were not suitable for grafting. The patient underwent pedicled left internal mammary artery grafting to LAD and radial artery to distal RCA, with the proximal end of the radial artery anastomosed on the aorta. Ventricular pacing wires were placed and closure was carried out in layers, with the sternum approximated using three loop stainless steel wires.
Cardiac surgery ICU and HDU recovery period lasted 26 days. The patient was commenced on thyroid hormone replacement therapy and calcium and vitamin D supplements. Sequelae included a failed extubation on day two due to bilateral vocal cord palsy, and resultant prolonged endotracheal intubation, with a tracheostomy performed on day 8. An extended ventilator-weaning period necessitated the commencement of nasogastric feeding between days 13–25. Other postoperative complications included ventilator-associated pneumonia, initially treated with piperacillin/tazobactam and subsequently changed to meropenem following sensitivity results. Anaemia required transfusion of 2 units of packed red blood cells. As the patient also exhibited transient hypertension and frank haematuria, outpatient flexible cystoscopy was arranged as per urology review. On day 26 the patient was transferred to the care of the otolaryngology team. He remained in hospital for a further 10 days and was then discharged.
The thyroid was subject to pathological examination. The gland was of substantial size, weighing 439 g and measuring 19 cm × 16 cm × 5.5 cm. A multinodular appearance was noted with respect to both lobes (Figure 7). Histological examination showed considerable variation in follicular size and colloid content with small areas of fibrosis and dystrophic calcification. There was no evidence of malignancy.
At 1-year follow up the patient remained asymptomatic. The right vocal cord function had improved and tracheostomy had since been reversed. The patient was confirmed to be euthyroid and was discharged from both cardiac and endocrine surgical care.
DiscussionOther Section
In general, combined cardiac surgery and thyroidectomy is regarded as a safe and efficacious procedure with good clinical outcomes. A recent review of the existing literature determined 16 key papers (3 retrospective case series and 13 case reports) on this topic (6). However, of a total cohort of 32 patients, only four underwent concomitant OPCABG with total thyroidectomy for a retrosternal goitre. In the first report, Mehta et al. (7) documented the case of a 66-year-old female with unstable angina (LMS disease) and severely compromised airway secondary to a multinodular retrosternal goitre. Initially, a subtotal thyroidectomy was performed, followed by OPCABG with saphenous vein grafts to the LAD and the ramus intermedius, with the absence of intraoperative complications. Following a slow ventilator-weaning period, the patient was returned to theatre for extubation under general anaesthesia, due to development of post-intubation tracheomalacia. The patient was discharged on the 8th day postoperatively, with normal respiratory and cardiac function and euthyroid hormone levels. In the second case report, Mehra et al. (8) performed combined OPCABG and thyroidectomy on a 70-year-old woman with extensive coronary artery disease, involving the LMS, and tracheal compression as a consequence of a retrosternal goitre. They reported a successful procedure, with no resultant postoperative complications. As a consequence of this combined approach, normal cardiovascular function and upper airway patency were established, with the patient discharged on postoperative day 10. In the third case report, this same combined procedure was performed on a 57-year-old female with coronary artery disease, which included 95% in-stent restenosis of the LAD, accompanied by a large retrosternal goitre (9). The reported postoperative period was uneventful and the patient was discharged 5 days later. Finally, in one case from the retrospective series reported by Testini et al. (10), a total thyroidectomy followed by CABG was performed. All the cases from the aforementioned 16 key papers which involved a combined procedure of isolated CABG and thyroidectomy are presented in Table 1.

Full table
This paper has presented a case involving the single-procedure treatment of two significant diseases of differing pathology, namely severe myocardial ischaemia and retrosternal goitre causing displacement and compression of adjacent structures. Both for our patient and in a wider context, the combined approach exhibits various advantages. Firstly, the anatomical proximity of the thyroid facilitates its excision in conjunction with CABG, making this a feasible surgical option (5). Furthermore, the cumulative risk of a combined operation seems to be less than the individual risks associated with each separate procedure and also avoids the need for resternotomy (15). A stand-alone thyroidectomy preceding CABG subjects a patient with coexisting coronary artery disease to significant risk associated with the use of general anesthesia. Conversely, an independently performed CABG prior to thyroidectomy cannot address goitre-related respiratory dysfunction and may result in a problematic and prolonged ventilator-weaning period. Moreover, CABG as an initial stand-alone procedure in cases of hyperthyroidism could lead to undesirable arrhythmias complicating the postoperative recovery period (5). In our case, an off-pump approach was preferable due to the patient’s increased age and impairment of left ventricular function. A significant advantage of OPCABG is the use of lower heparin doses relative to on-pump procedures, which reduces the risk of bleeding, especially from the highly vascularised thyroid (16).
In conclusion, it is our view that a simultaneous, dual discipline approach combining OPCABG and thyroidectomy for a retrosternal goitre can be safely and effectively performed to achieve good clinical outcomes, provided that perioperative levels of thyroid hormones are maintained at euthyroid or hypothyroid levels.
AcknowledgementsOther Section
None.
FootnoteOther Section
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
ReferencesOther Section
- Hedayati N, McHenry CR. The clinical presentation and operative management of nodular and diffuse substernal thyroid disease. Am Surg 2002;68:245-51; discussion 251-2. [PubMed]
- Raffaelli M, De Crea C, Ronti S, et al. Substernal goiters: incidence, surgical approach, and complications in a tertiary care referral center. Head Neck 2011;33:1420-5. [Crossref] [PubMed]
- Ahmed ME, Ahmed EO, Mahadi SI. Retrosternal goiter: the need for median sternotomy. World J Surg 2006;30:1945-8; discussion 1949.
- Rugiu MG, Piemonte M. Surgical approach to retrosternal goitre: do we still need sternotomy? Acta Otorhinolaryngol Ital 2009;29:331-8. [PubMed]
- Abboud B, Sleilaty G, Asmar B, et al. Interventions in heart and thyroid surgery: can they be safely combined? Eur J Cardiothorac Surg 2003;24:712-5. [Crossref] [PubMed]
- De Silva RP, Dignan RJ. Does a combined procedure for cardiac surgery and thyroidectomy offer acceptable outcomes? Interact Cardiovasc Thorac Surg 2015;21:787-91. [Crossref] [PubMed]
- Mehta Y. OPCAB and thyroidectomy in a patient with a severely compromised airway. J Cardiothorac Vasc Anesth 2005;19:79-82. [Crossref] [PubMed]
- Mehra AP, Shah KS, Jain PC, et al. Combined off-pump coronary artery bypass grafting and thyroidectomy. Ann Thorac Surg 2009;88:661-3. [Crossref] [PubMed]
- Cetin E, Ozyuksel A, Dalbasi E. Single stage substernal thyroidectomy and off-pump coronary artery bypass grafting: is it worth using cardiopulmonary bypass unless absolutely necessary? BMJ Case Rep 2014;2014.
- Testini M, Poli E, Lardo D, et al. Combined cardiac surgery and total thyroidectomy: our experience and review of the literature. Thorac Cardiovasc Surg 2010;58:450-4. [Crossref] [PubMed]
- Gürkan S, Hüseyin S, Saraç A, et al. Combined cardiac surgery and substernal thyroidectomy. Türk Göğüs Kalp Damar Cerrahisi Dergisi 2012;20:629-31.
- Koçak H, Becit N, Erkut B, et al. Combined coronary arterial bypass graft and thyroidectomy in a patient with giant goiter: how reliable is it? Thorac Cardiovasc Surg 2007;55:56-8. [Crossref] [PubMed]
- Litmathe J, Kurt M, Boeken U, et al. Combined cardiothoracic surgery and interventions of the para/thyroid gland. A rare clinical cooperation. Z Kardiol 2005;94:28-32. [Crossref] [PubMed]
- Wexler S, Yamane K, Fisher KW, et al. Single-stage operation for giant substernal goiter with severe coronary artery disease. Ann Thorac Cardiovasc Surg 2011;17:524-7. [Crossref] [PubMed]
- Wolfhard U, Krause U, Walz MK, et al. Combined interventions in heart and thyroid surgery--an example of interdisciplinary cooperation. Chirurg 1994;65:1107-10. [PubMed]
- Englberger L, Streich M, Tevaearai H, et al. Different anticoagulation strategies in off-pump coronary artery bypass operations: a European survey. Interact Cardiovasc Thorac Surg 2008;7:378-82. [Crossref] [PubMed]