Early cardiology assessment and intervention reduces mortality following myocardial injury after non-cardiac surgery (MINS)
Introduction
In patients undergoing general thoracic surgery, perioperative myocardial infarction is associated with high early post-operative mortality (1-4). However, the diagnosis remains challenging. The Vascular events In noncardiac Surgery patIents cOhort evaluatioN (VISION) investigators recently defined myocardial injury after non-cardiac surgery (MINS) solely on troponin level regardless of ischaemic features on 12-lead electrocardiogram (ECG) or clinical presentation (1), reporting isolated troponin elevation as an independent predictor of high 30-day mortality.
In general troponin levels are rarely routinely measured for patients undergoing general thoracic (non-cardiac) surgery, so the incidence of MINS outside the VISION study cohort is not established. It has been reported that 8% of patients would suffer MINS with the majority (58%) not fulfilling the universal definition of myocardial infarction. More importantly, having identified a risk factor for early post-operative (presumably) ischaemic heart disease related death, little is known on the efficacy of cardiology intervention to mitigate this risk.
The aim of our study is to determine the impact of early cardiology consultation and intervention on 30-day mortality and long-term outcomes in patients who underwent general thoracic surgery and suffered MINS.
Methods
We conducted a retrospective review of a consecutive series of patients who underwent thoracic surgery under the care of a single surgeon (Eric Lim) at the Royal Brompton Hospital over a 5-year period. Ethical review and Research and Development (R&D) approval was not required as this was a service evaluation study. Troponin I was routinely requested on the first post-operative day for all patients who underwent surgery with levels of ≥0.04 ng/mL was classified as positive. Baseline and cardiac risk factors were collected and entered prospectively into the thoracic surgical database. Patients who had troponin levels of ≥0.04 ng/mL were referred to inpatient cardiology services. Further investigations and management of these patients were determined by the cardiologists on an individual basis depending on patients’ cardiac risk factors. Investigations include 12-lead ECG, echocardiogram and diagnostic angiogram. Management was tailored to each patient and include primary risk factor modification, pharmacological strategies and invasive coronary intervention. Serum troponin levels were obtained from the hospital’s electronic records and mortality status documented from patient records and the NHS spine and summary care record system (https://portal.national.ncrs.nhs.uk/portal/dt, NHS, UK).
Statistical analysis
Continuous data were summarised as mean and standard deviation (SD) or median with interquartile range (IQR) as appropriate to the data distribution, and categorical data presented as frequency with percentage (%). Patients were grouped according to post-operative troponin status and compared using, t-test, Mann-Whitney, chi-square or Fisher’s exact test as appropriate to the distribution and expected frequency counts between the groups. Actuarial survival was calculated using Kaplan Meier product limit method and compared with the log rank test. Cox proportional hazards regression was utilized to determine risk adjusted impact of MINS on post-operative survival. Statistical analyses were performed using R version 3.0 (R Core Development Team, Vienna, Austria).
Results
Between 2nd September 2008 and 9th February 2013, a total of 511 patients underwent thoracic surgery. Of the 511 patients that had surgery, 491 (96%) had Troponin I assayed measured routinely on day-1 after surgery. Eighty patients (16%) had a troponin above the upper reference level (≥0.04 ng/mL), fulfilling the MINS criteria. Patients with MINS were more likely to be older, smokers and hyperlipidemic (Table 1). Sixty-one patients (76%) with Troponin I ≥0.04 ng/mL received cardiology consult. Eleven (14%) of them had an associated tachyarrhythmia (Ten patients developed atrial fibrillation and one patient developed ventricular tachycardia). Only four (5%) were diagnosed with myocardial infarction in accordance to the third universal definition (5). Echocardiogram was performed in 49 (61%) patients, where 43 were reported as “no regional wall motion abnormality”, one was reported as “global hypokinesia”, and six echocardiograms detected valvular diseases including aortic stenosis and tricuspid regurgitation.
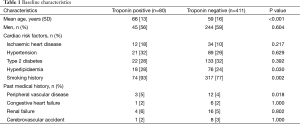
Full table
Intervention consisted of addition of pharmacological agents and risk factor modification. In total, 20 (25%) patients were commenced on anti-platelet agents (aspirin and clopidogrel) prior to discharge and 49 patients (61%) had primary risk factors modification including lifestyle changes, smoking cessation advice, blood pressure, lipid and sugar level control. In addition, patients were referred back to their primary general practitioners for maintenance of risk factors modification measures that were instituted in-hospital.
Subsequently, 26 (33%) patients were followed up in routine outpatient cardiology clinics for evaluation of symptoms, clinical examination and Thallium myocardial perfusion scan. A smaller number of patients were initiated on statins (6, 8%) and β-blocker (4, 5%) whilst none were started with ACE inhibitor. Only one (1%) patient underwent a diagnostic angiogram and proceeded to percutaneous coronary intervention (Table 2).
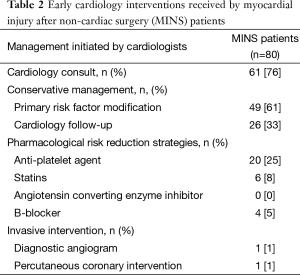
Full table
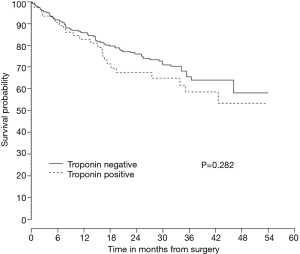
On follow-up, although the patients with MINS had lower survivorship, the difference was not statistically significant (P=0.282) (Figure 1).
Discussion
Challenge of diagnosing perioperative myocardial infarction
The incidence of perioperative cardiovascular events after general thoracic surgery ranges from 0.6% to 7.5%, due to the application of definitions that were inconsistent and highly variable including combinations of cardiovascular death, increase in CK-MB, and/or ischaemic changes on ECG (2,3,6-9). The diagnosis of perioperative or post-operative myocardial infarction based on universal definition remains challenging as many patients are receiving intravenous or oral analgesic postoperatively that may mask typical ischaemic symptoms and more than 80% of perioperative myocardial infarctions do not exhibit typical Q wave changes consistent with ischaemia on ECGs (10). In the absence of improved criteria and the current universal definition, perioperative cardiovascular events likely lead to under-diagnosis.
Significance of myocardial injury
The VISION definition facilitated a standard definition of MINS and our results indicate that MINS is common; identified in 16% of patients after elective general thoracic surgery. The uptake of routine screening using MINS criteria is met with a number of challenges, the first is that clinicians may not be generally convinced that asymptomatic troponin elevation is due specifically to myocardial injury and the second is whether a positive result would alter any change in management.
Many argue that troponin elevation can be raised in a number of non-cardiac conditions (11). The VISION study excluded patients at high risk of death due to secondary causes of troponin elevation such as sepsis and pulmonary embolism and still demonstrated MINS is significantly associated with high mortality and morbidity. In our study, we did not exclude “non-ischaemic” causes for troponin elevation, as 11 of our MINS patients experienced a tachyarrhythmia, a known association of troponin elevation. This is because we are uncertain if the tachyarrhythmia could be a secondary manifestation of myocardial injury. This argument could extent to traditional “non-ischaemic” conditions such as sepsis or pulmonary embolism that may be associated with myocardial injury small enough to be detected biochemically but not clinically.
In-hospital management of myocardial injury
In general clinicians perform investigations only if subsequent management is likely to positively influence outcome and the benefits (of the proposed intervention) outweigh its risks. The challenge in the MINS setting is that post-operative troponin elevation is associated with increased mortality (1,2,12-14), but the management is unclear. The MINS cohort is likely to represent a mixed aetiology for ischaemia that may range from myocardial hypoperfusion to acute plaque instability and rupture. We hypothesise that in our cohort, MINS served as a surrogate marker for existing coronary artery disease that manifested during surgery during periods of hypotension (during induction of anaesthesia or intraoperative factors such as hypovolaemia) resulting in imbalance of oxygen-demand supply leading to type-2 myocardial infarction (15). Clearly being able to accurately identify the aetiology would be important to help direct treatment with risk factor modification and secondary prevention alone as the appropriate strategy of the pre-existing coronary artery disease group moving to an acute coronary syndrome paradigm/acute primary percutaneous coronary intervention for patients with plaque instability and rupture.
In our study, the majority of our patients who suffered a MINS event that were referred to cardiologists had risk factor modification, with 25% and 5% medically managed on aspirin and beta-blocker respectively (16,17), and one managed with PCI.
Longer term outcome
On follow-up, our data shows a small difference in late survival probability between patients suffering from MINS and those that did not, although this was not statistically significant, possibly alluding to a benefit of early cardiology intervention.
Limitations
Given that maintenance of primary risk factor modification was conducted in primary care, we have assumed that compliance was achieved in all patients.
Further work
Our results underscore the importance of screening for MINS after non-cardiac surgery and highlight the importance of early cardiology assessment and intervention. Further work needs to be undertaken to elucidate the underlying pathogenesis for MINS to help inform on the correct treatment strategy. Larger scale studies are required to ascertain the impact (if any) of MINS on survival and any influence of subsequent longer terms management.
Conclusions
Our results confirm MINS is common after general thoracic surgery. We observed that early cardiology intervention reduced the expected hazard ratio of early death from 3.87 to an odds ratio of 1.69 with no significant difference in 30-day mortality for patients who developed MINS compared to those without evidence of post-operative troponin elevation, underscoring the importance of early cardiology assessment and intervention.
Acknowledgements
None.
Footnote
Conflicts of Interest: This paper was read at the Scientific Session (poster and e-Abstract categories) of the American Heart Association in Chicago on 18 November 2014.
References
- Botto F, Alonso-Coello P, Chan MT, et al. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology 2014;120:564-78. [Crossref] [PubMed]
- Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1997;100:1043-9. [Crossref] [PubMed]
- Boersma E, Kertai MD, Schouten O, et al. Perioperative cardiovascular mortality in noncardiac surgery: validation of the Lee cardiac risk index. Am J Med 2005;118:1134-41. [Crossref] [PubMed]
- Devereaux PJ, Xavier D, Pogue J, et al. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort study. Ann Intern Med 2011;154:523-8. [Crossref] [PubMed]
- Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol 2012;60:1581-98. [Crossref] [PubMed]
- Ashton CM, Petersen NJ, Wray NP, et al. The incidence of perioperative myocardial infarction in men undergoing noncardiac surgery. Ann Intern Med 1993;118:504-10. [Crossref] [PubMed]
- Kumar R, McKinney WP, Raj G, et al. Adverse cardiac events after surgery: assessing risk in a veteran population. J Gen Intern Med 2001;16:507-18. [Crossref] [PubMed]
- Shah KB, Kleinman BS, Rao TL, et al. Angina and other risk factors in patients with cardiac diseases undergoing noncardiac operations. Anesth Analg 1990;70:240-7. [Crossref] [PubMed]
- von Knorring J, Lepäntalo M, Lindgren L, et al. Cardiac arrhythmias and myocardial ischemia after thoracotomy for lung cancer. Ann Thorac Surg 1992;53:642-7. [Crossref] [PubMed]
- Priebe HJ. Perioperative myocardial infarction--aetiology and prevention. Br J Anaesth 2005;95:3-19. [Crossref] [PubMed]
- Khan IA, Tun A, Wattanasauwan N, et al. Elevation of serum cardiac troponin I in noncardiac and cardiac diseases other than acute coronary syndromes. Am J Emerg Med 1999;17:225-9. [Crossref] [PubMed]
- Badner NH, Knill RL, Brown JE, et al. Myocardial infarction after noncardiac surgery. Anesthesiology 1998;88:572-8. [Crossref] [PubMed]
- Martinez EA, Nass CM, Jermyn RM, et al. Intermittent cardiac troponin-I screening is an effective means of surveillance for a perioperative myocardial infarction. J Cardiothorac Vasc Anesth 2005;19:577-82. [Crossref] [PubMed]
- van Waes JA, Nathoe HM, de Graaff JC, et al. Myocardial injury after noncardiac surgery and its association with short-term mortality. Circulation 2013;127:2264-71. [Crossref] [PubMed]
- Landesberg G, Beattie WS, Mosseri M, et al. Perioperative myocardial infarction. Circulation 2009;119:2936-44. [Crossref] [PubMed]
- Randomised trial of intravenous atenolol among 16 027 cases of suspected acute myocardial infarction: ISIS-1. First International Study of Infarct Survival Collaborative Group. Lancet 1986;2:57-66. [PubMed]
- Baigent C, Collins R, Appleby P, et al. ISIS-2: 10 year survival among patients with suspected acute myocardial infarction in randomised comparison of intravenous streptokinase, oral aspirin, both, or neither. The ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. BMJ 1998;316:1337-43. [Crossref] [PubMed]


