
Pectus repair after prior sternotomy: clinical practice review and practice recommendations based on a 2,200-patient database
Introduction
Background
Since the introduction of the minimally invasive repair of pectus excavatum (MIRPE) by Dr. Donald Nuss to the American Pediatric Surgical Association in 1998, the MIRPE procedure is widely accepted as a method of pectus excavatum (PE) chest wall deformity repair (1,2). For many surgeons, this approach is preferable to the alternative method of repair involving resection of costal cartilage and sternal fracture, described by Ravitch in 1949 (3-5). The incidence of PE in patients with congenital heart disease is uncommon, however there are occasions where repair is considered in patients with prior history of median sternotomy. At this authors’ institution where the MIRPE procedure was first developed in 1987 by Dr. Nuss, the procedure has since been performed on over 2,200 patients, nine of which were performed in patients with history of prior sternotomy.
Rationale and knowledge gap
The most feared complication of MIRPE is iatrogenic cardiac injury; a 14-center review reported the incidence to be as high as 7% after analyzing 75 patients with history of sternotomy who underwent MIRPE (6). There exists little literature on best practices to prepare for MIRPE after prior sternotomy.
Objective
The goal of this review is to discuss MIRPE after prior median sternotomy and recommend techniques to optimize surgical outcomes.
Review of MIRPE procedure after previous sternotomy
MIRPE following median sternotomy may be complicated by the development of post-surgical adhesions, which can complicate the procedure by resulting in fusion of the posterior sternum, pericardium, and/or myocardium. There is a high risk of iatrogenic injury during MIRPE due to these adhesions when performing the dissection in the retrosternal space. While Dr. Nuss first described MIRPE by advancing a Kelly clamp across the retrosternal space by feel alone, he later introduced thoracoscopy as a method to prevent cardiac injury during this step (2). Thoracoscopy has now become standard practice during MIRPE (7,8). Using thoracoscopy, the surgeon maintains direct visualization of the tip of the dissecting instrument at all times, keeps a clear view of the pericardial sac away from the sternum, and sees the contralateral exit site during passage of the introducer. This is described as the “critical view” for performing MIRPE safely (9,10). In cases of prior sternotomy, it is important to note that thoracoscopy alone is not adequate to maintain the “critical view”.
In addition to thoracoscopy, the use of sternal elevation improves visualization of the mediastinal dissection during MIRPE by improving the critical view (11). There are multiple methods by which sternal elevation can be performed, including off-label use of a vacuum bell applied externally to the sternum (12-14), various methods of crane elevation first described by Park (15), and by use of a subxiphoid incision for manual elevation of the sternum (16,17). In patients without prior sternotomy, selective sternal elevation has been demonstrated to be safe (10). However, in cases of prior sternotomy, routine sternal elevation was frequently used but alone was inadequate to prevent iatrogenic cardiac injury.
The largest retrospective study analyzing MIRPE in prior sternotomy patients is a multi-institutional review involving 75 patients from 14 centers, known as the Chest Wall International Group, spanning from November 2000 to August 2015. The review included patients who had PE deformity with a history of sternotomy for cardiac surgery and an attempted PE repair with substernal Nuss bar placement. Sternal elevation was used in 9 of 14 centers and a total of 34 patients. Of the 9 centers that used sternal elevation, only 6 of them used sternal elevation in every case of prior sternotomy, with the remaining using selective sternal elevation. In this review, iatrogenic cardiac injury was reported during the procedure in 5 patients. In all cases, the surgeon used either thoracoscopy or pectoscope to visualize the retrosternal dissection. Two of the 5 cases of cardiac injury used sternal elevation as part of the procedure. With this analysis, the authors advocate for routine use of sternal elevation in cases of prior sternotomy though there is not enough data to support a decrease in risk of cardiac injury with sternal elevation alone given the low case numbers (6).
In their review of performance of MIRPE procedure in 35 post-sternotomy patients from 2011 to 2019, Liu and colleagues in Shijiazhuang, China not only advocate for the use of sternal elevation during the procedure but also supported other modifications to the MIRPE including the addition of direct sub-xiphoid retrosternal dissection; this allows for insertion of thoracoscope in addition to direct dissection of adhesions by blunt dissection and cautery, which they performed in 29 of their 35 post-sternotomy patients (18). The practice of utilizing a sub-xiphoid incision to directly dissect the retrosternal space for the purposes of lysing dense retrosternal adhesions is well-described in the literature for cardiac surgery in cases of re-do sternotomy (19,20). Liu and colleagues reported uneventful recovery from the MIRPE procedure with this modification aside from one incident of emergent re-sternotomy for cardiac injury during the dissection of a dense adhesion between the right atrium and the sternum, and report the patient recovered well from their repair with assistance from a cardio-thoracic surgeon (18). The practice of using direct sub-xiphoid retrosternal dissection for MIRPE is further supported by Chen and colleagues at Beijing Children’s Hospital, who reviewed 49 cases of MIRPE in patients with prior history of repair of congenital heart disease. The authors described a management algorithm of their patients based on an estimation of the severity of adhesions with thoracoscopy, computerized tomography (CT) scan, and/or echocardiogram. For patients with severe adhesions, a midline sub-sternal incision was added to the standard MIRPE with finger-assisted dissection of adhesions in the retrosternal space with use of thoracoscopic monitoring. The authors reported success with this technique, though it was not without risk with an associated iatrogenic cardiac injury incidence of 6.1% (21). With low numbers of MIRPE procedure in post-sternotomy patients internationally, further research is needed but prudent modifications are noteworthy to improve the safety profile of these rare cases.
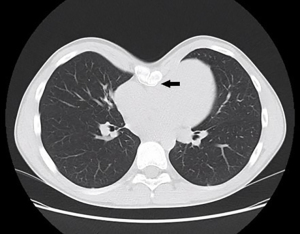
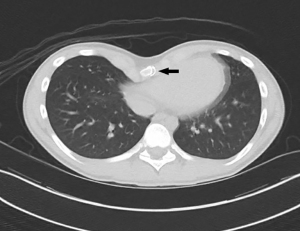
Single institution experience with MIRPE procedure after previous sternotomy
To review the cases of MIRPE in patients with prior median sternotomy at this institution, an IRB-approved (No. 01-05-EX-0175-HOSP) retrospective review was performed from 1/1/1997 to 9/1/2022 to query these patients (Table 1). A total of 9 patients were found to have undergone MIRPE after previous median sternotomy. The age of patients ranged from 9 to 24 years of age. Most of the patients underwent previous sternotomy for repair of various cardiac conditions, while 2 of the 9 patients underwent sternotomy for non-cardiac reasons, including one who had previously undergone a Ravitch procedure. Iatrogenic cardiac injury occurred in 2 patients. Evaluation of the preoperative CT scans in these cases demonstrates the location of sternal wires on cross-sectional imaging (Figures 1,2). All cases were performed with thoracoscopic assistance. Sternal elevation was used in 7 of the 9 patients to improve visualization of the retrosternal dissection. The methods that were used included vacuum bell, sub-xiphoid manual elevation, and crane retractor techniques. A cardio-thoracic surgeon was available on-site for all the cases but were present in the operating room (OR) for 6 of the patients and assisted for 5 of them, including the two cases of iatrogenic cardiac injury. Three of the cases were performed with groins surgically prepped in preparation for the emergent need for cardiopulmonary bypass but was never required. One of the patients with iatrogenic cardiac injury required an emergent sternotomy and had an estimated blood loss (EBL) of 2 L with need for transfusion of blood products. The repair involved placement of four interrupted 3-0 prolene non-pledgeted vertical mattress sutures in a tear in the right ventricle, and the total time of repair was less than 1 hour. The patient did not initially undergo sternal elevation for their procedure as the surgeon only performs it selectively, though optimal thoracoscopic visualization was reported during the retrosternal dissection, which highlights the point made earlier. The patient experienced full recovery though MIRPE was not completed. The practice of performing a direct sub-xiphoid retrosternal dissection to allow for safer dissection as described by Liu was used in 6 of the 9 patients, but still resulted in one cardiac injury. During this case, the injury occurred while the cardiothoracic surgeon lysed the retrosternal adhesions. The injury was small and repaired in a controlled fashion without the need for emergent sternotomy and with minimal blood loss. The patient’s PE repair was completed with two bars without further complication.
Table 1
| Age of MIRPE (years) | Age of prior sternotomy | Reason for sternotomy | # of bars placed | EBL (mL) | Thoracoscopy | Method of sternal elevation | Groin prepped | CT surgery present | Cardiac injury | Noted details of MIRPE procedure |
|---|---|---|---|---|---|---|---|---|---|---|
| 13 | 4 years | ASD repair | 2 | 5 | Yes | Manual elevation with retractor | No | No | No | DSRD was performed by the pediatric surgeon for retrosternal dissection |
| 9 | 3 days | Sternal cleft repair | 2 | <5 | Yes | Vacuum bell | No | No | No | |
| 17 | 4 months, 6 months | VSD repair, aortopexy | 2 | <5 | Yes | Manual elevation with retractor | No | Yes | No | DSRD was performed by CTS for retrosternal dissection |
| 17 | newborn | TGA-IAA repair | 2 | 10 | Yes | Manual elevation with retractor | No | Yes | No | DSRD was performed by CTS for retrosternal dissection |
| 15 | 3 years | VSD and ASD repair | 1 | 2,000 | Yes | None | No | Yes, after injury | Yes | Cardiac injury occurred during passage of a second bar. Median sternotomy was performed by CTS for repair of right ventricular injury. MIRPE was not completed |
| 14 | 9 months | Atrioventricular canal defect repair | 2 | 5 | Yes | None | Yes | Yes | No | CTS was present for retrosternal dissection |
| 24 | 20 years | Ravitch procedure | 1 | 100 | Yes | N/A, elevation was performed | No | No | No | Ravitch repair was opened, sternum was dissected down to include a sub-xiphoid window, DSRD was performed |
| 17 | 1 year | Pericardial patch closure of an ASD | 2 | 15 | Yes | Crane retractor | Yes | Yes | No | CTS performed DSRD |
| 19 | Newborn, 2 years |
BT shunt ligation, RVOT reconstruction with transannular patch and ASD closure | 1 | 25 | Yes | Crane retractor | Yes | Yes | Yes | CTS performed DSRD, cardiac injury occurred during this dissection and was repaired without re-sternotomy |
ASD, atrial septal defect; BT, Blalock-Taussig; CT, computerized tomography; CTS, cardio-thoracic surgery; DSRD, direct sub-xiphoid retrosternal dissection; EBL, estimated blood loss; IAA, interrupted aortic arch; MIRPE, minimally invasive repair of pectus excavatum; N/A, not available; RVOT, right ventricular outflow tract; TGA, transposition of great arteries; VSD, ventricular septal defect.
Recommendations for practice
Although MIRPE after previous sternotomy is uncommon, review of available literature and this institution’s experience allow one to draw some important conclusions about how to improve safety in these challenging cases. Recommendations for optimizing the procedure based on this information include:
- Thoracoscopy should be utilized in all cases of MIRPE after prior sternotomy to optimize visualization of retrosternal space and to improve the “critical view” as described in the literature for safe repair of PE (9,10);
- Sternal elevation is recommended on a routine basis for patients undergoing MIRPE after sternotomy to improve visualization of the retrosternal space during dissection of post-surgical adhesions;
- Direct sub-xiphoid retrosternal dissection is also strongly recommended, and may be performed by the primary surgeon or a cardio-thoracic surgeon if appropriate;
- Cardio-thoracic surgeon(s) are highly recommended to assist during the operation but must be available on-site to assist in the event of an iatrogenic cardiac injury;
- Cardiac bypass preparation should be performed including surgically prepping the patient’s groins in case of emergent need for cardiac bypass. The procedure should be performed in an OR where cardiopulmonary bypass can be performed;
- Massive blood transfusion protocol with appropriate intravenous access must be available.
Limitations
Limitations of this evaluation include the retrospective nature of the study with a small number of patients over a 20-year time period managed by different surgeons. In addition, a potential limiting factor is the patients had their initial sternotomy for different reasons which could affect the degree of scarring in the retrosternal plane. Finally, the severity of pectus deformity could also affect the incidence of cardiac injuries, but since this was the only patient population to sustain cardiac injuries at our institution this effect should be minimal.
Conclusions
Since the introduction of the MIRPE procedure by Dr. Nuss in 1998, the procedure has become the standard for repair of PE. In rare cases, patients with a history of prior sternotomy may present for repair and are at the highest risk of iatrogenic injury due to retrosternal post-surgical adhesions. With appropriate preparation and safe practices including the recommendations as listed above, surgical outcomes can be optimized for this patient population.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Erik R. de Loos, Jean H. T. Daemen and Frank-Martin Haecker) for the series “Minimally Invasive Treatment of Pectus Deformities” published in Journal of Thoracic Disease. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1567/coif). The series “Minimally Invasive Treatment of Pectus Deformities” was commissioned by the editorial office without any funding or sponsorship. RJO declares the consulting fees paid to practice from Zimmer Biomet. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kelly RE Jr. Modifications and Further Development of the Original Nuss Procedure: Blessing or Curse? Eur J Pediatr Surg 2018;28:304-19. [Crossref] [PubMed]
- Nuss D, Kelly RE Jr, Croitoru DP, et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998;33:545-52. [Crossref] [PubMed]
- Nuss D, Obermeyer RJ, Kelly RE. Nuss bar procedure: past, present and future. Ann Cardiothorac Surg 2016;5:422-33. [Crossref] [PubMed]
- Mao YZ, Tang S, Li S. Comparison of the Nuss versus Ravitch procedure for pectus excavatum repair: an updated meta-analysis. J Pediatr Surg 2017;52:1545-52. [Crossref] [PubMed]
- Ravitch MM. The Operative Treatment of Pectus Excavatum. Ann Surg 1949;129:429-44. [Crossref] [PubMed]
- Jaroszewski DE, Gustin PJ, Haecker FM, et al. Pectus excavatum repair after sternotomy: the Chest Wall International Group experience with substernal Nuss bars. Eur J Cardiothorac Surg 2017;52:710-7. [Crossref] [PubMed]
- Croitoru DP, Kelly RE Jr, Goretsky MJ, et al. Experience and modification update for the minimally invasive Nuss technique for pectus excavatum repair in 303 patients. J Pediatr Surg 2002;37:437-45. [Crossref] [PubMed]
- Nuss D. Minimally invasive surgical repair of pectus excavatum. Semin Pediatr Surg 2008;17:209-17. [Crossref] [PubMed]
- Notrica DM. Modifications to the Nuss procedure for pectus excavatum repair: A 20-year review. Semin Pediatr Surg 2018;27:133-50. [Crossref] [PubMed]
- Obermeyer RJ, Goretsky MJ, Kelly RE Jr, et al. Selective use of sternal elevation before substernal dissection in more than 2000 Nuss repairs at a single institution. J Pediatr Surg 2021;56:649-54. [Crossref] [PubMed]
- Haecker FM, Krebs T, Kocher GJ, et al. Sternal elevation techniques during the minimally invasive repair of pectus excavatum. Interact Cardiovasc Thorac Surg 2019;29:497-502. [Crossref] [PubMed]
- Haecker FM, Sesia SB. Intraoperative use of the vacuum bell for elevating the sternum during the Nuss procedure. J Laparoendosc Adv Surg Tech A 2012;22:934-6. [Crossref] [PubMed]
- Schier F, Bahr M, Klobe E. The vacuum chest wall lifter: an innovative, nonsurgical addition to the management of pectus excavatum. J Pediatr Surg 2005;40:496-500. [Crossref] [PubMed]
- Haecker FM, Sesia S. Vacuum bell therapy. Ann Cardiothorac Surg 2016;5:440-9. [Crossref] [PubMed]
- Park HJ, Jeong JY, Jo WM, et al. Minimally invasive repair of pectus excavatum: a novel morphology-tailored, patient-specific approach. J Thorac Cardiovasc Surg 2010;139:379-86. [Crossref] [PubMed]
- Gould JL, Sharp RJ, Peter SD, et al. The Minimally Invasive Repair of Pectus Excavatum Using a Subxiphoid Incision. Eur J Pediatr Surg 2017;27:2-6. [Crossref] [PubMed]
- Rygl M, Vyhnanek M, Kucera A, et al. Technical innovation in minimally invasive repair of pectus excavatum. Pediatr Surg Int 2014;30:113-7. [Crossref] [PubMed]
- Liu S, Wang L, Zhang H, et al. Modified Nuss procedure with a novel steel bar in patients with pectus excavatum post-congenital heart surgery. Interact Cardiovasc Thorac Surg 2022;34:424-30. [Crossref] [PubMed]
- Kouchoukos NT, Blackstone EH, Hanley FL, et al. Kirklin/Barratt-Boyes Cardiac Surgery: Morphology, Diagnostic criteria, Natural history, Techniques, Results, and indications. 4th edition. Elsevier, 2013.
- Kaiser LR, Kron IL, Spray TL. Mastery of Cardiothoracic Surgery. 3rd edition. Lippincott Williams & Wilkins, 2014.
- Chen C, Li X, Zhang N, et al. Different Nuss procedures and risk management for pectus excavatum after surgery for congenital heart disease. J Pediatr Surg 2018;53:1964-9. [Crossref] [PubMed]


