Predictive scores in chronic total occlusions percutaneous recanalization: only fashionable or really useful?
Introduction
Chronic total occlusions (CTOs) remain one of the last challenges in percutaneous coronary intervention (PCI). During the last decade, following the Japanese pioneers, the interest of interventionalists’ community in CTO PCI has dramatically increased leading to an important development in equipment and techniques (1,2), and a growing expertise among dedicated operators, both resulting in increased success rates (3).
CTO PCI attempts are considered to be more costly and cumbersome procedures in comparison with continuous lesions angioplasty; and might be associated with higher incidence of peri-procedural complications (4). Different reports have underlined the importance of patients’ selection in CTO PCI (5,6). Indeed, the decision-making process of whom to undergo CTO percutaneous attempt, should pass through a rational analysis, taking into account clinical and anatomical factors and operator’s experience (6). In addition, it is well recognized that patients affected by CTOs and successfully revascularized showed better clinical long-term outcome and improved quality of life as compared with those who underwent failed CTO PCI attempt (7,8).
For all these reasons, establishing scores able to strongly predict the success of CTO recanalization and to select appropriate candidates for a percutaneous attempt among CTO patients, and could represent a key issue to achieve optimal immediate and long-term outcome.
Predictive scores in CTO PCI
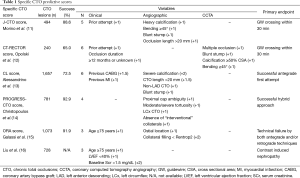
The Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) score is an angiographic tool that can quantify the degree of atherosclerosis in the entire coronary arterial tree, including the culprit lesions and is useful to select appropriate candidates for coronary artery bypass graft (CABG) surgery or PCI with drug-eluting stents in patients with left main and/or three-vessel disease (9). Nagashima et al. reported lower procedural success of CTO PCI in patients with a high SYNTAX (>22) score than those with a low SYNTAX score (74.7% vs. 91.8%, respectively; P<0.0001) (10). Moreover, a SYNTAX score >22 was also an independent predictor of 30-day major adverse cardiac events (odds ratio =4.80, 95% CI: 1.03–22.42) (10). Nonetheless, the use of SYNTAX score is more appropriate for diseased patent coronary arteries than CTOs, particularly when PCI is indicated. Indeed, the weight given to the presence of a CTO in the calculation of the SYNTAX score is such that very few patients with multi-vessel disease and a CTO will qualify for PCI, because a complex left anterior descending (LAD) CTO will almost be sufficient by itself to reach the surgical threshold of 23 (or 33 if the left main is involved). Therefore, specific scores to the setting of CTO lesions have been developed (Table 1).
Full table
The Japanese Multicenter CTO Registry (J-CTO) score was originally developed by Morino et al. (11) to predict the likelihood of successful guidewire (GW) crossing within 30 min. Independent angiographic predictors of failure (each given 1 point) that made up the J-CTO score included prior failed attempt, angiographic evidence of heavy calcification, bending ≥45° within the occluded segment, blunt proximal stump, and occlusion length >20 mm (11). Accordingly, CTO lesions were then graded as easy, intermediate, difficult, and very difficult (J-CTO scores of 0, 1, 2, and ≥3 respectively). Since then, the J-CTO score has been found to predict the overall likelihood of CTO PCI success (10,17); however, other reports demonstrated low calibration and discrimination of J-CTO score in predicting technical success of CTO percutaneous attempts (15,18). Similarly to Christopoulos et al. (17), we have shown that the higher the J-CTO score, the greater the use of antegrade dissection reentry techniques and retrograde approaches. This latter finding suggests that for difficult and very difficult lesions as assessed by J-CTO, early change of crossing strategy is recommended to avoid unnecessary delays predisposing to failure and complications. Recently, Galassi et al. (19) demonstrated that J-CTO score ≥3 was not only associated with procedural failure but also an independent predictor of worse cardiovascular long-term outcome (hazard ratio: 2.08; 95% CI: 1.32–3.27; P=0.002) in CTO patients attempted retrogradely.
In terms of pre-procedural evaluation, multiple studies have demonstrated a high diagnostic accuracy of coronary computed tomography angiography (CCTA) for the assessment of CTOs (12,20,21). Li et al. showed that a J-CTOCT score determined by coronary CCTA closely correlates to the angiographic J-CTO score (20). Opolski and coworkers developed the Computed Tomography Registry of Chronic Total Occlusion Revascularization (CT-RECTOR) score including the following clinical (previous attempt, occlusion duration ≥12 months or unknown) and CCTA (multiple occlusions, blunt stump, calcification ≥50% of CTO cross-sectional area, and bending ≥45°) variables (12). By assigning 1 point for each variable and summing all points accrued, the established CT-RECTOR score was able to strongly predict the probability of GW crossing within 30 min (12). Other CCTA parameters have been demonstrated to predict procedural success. Chen et al. showed that the attenuation of the proximal segment of CTO lesions, along occlusion length and total coronary calcium score as assessed by CCTA have predictive value for PCI outcomes (21).
In patients who underwent first antegrade attempt, Alessandrino et al. (13) established the CL-score, including both clinical and angiographic score variables [previous CABG (+1.5), previous myocardial infarction (MI) (+1), severe lesion calcification (+2), CTO length >20 mm (+1.5), non-LAD CTO (+1), and blunt stump (+1)]. Score values of 0 to 1, >1 and <3, ≥3 and <5, and ≥5 identified subgroups at high, intermediate, low, and very low probability, respectively, of CTO-PCI success rates. Hence, CL score could be suitable to be applied at centers where the retrograde or hybrid approach has not yet been implemented.
In the Prospective Global Registry for the Study of Chronic Total Occlusion Intervention (PROGRESS CTO), the investigators reported the efficiency and the safety of hybrid approach in CTO recanalization (22). A prediction model (PROGRESS CTO score) for estimating technical success using such an approach was developed and consisted of four angiographic variables [proximal cap ambiguity (1 point), moderate/severe tortuosity (1 point), circumflex artery CTO (1 point), and absence of “interventional” collaterals (1 point)] (14).
Very recently, we have established the ORA score [O: ostial location (1point); R: collateral filling < Rentrop 2 (2 points); A: age ≥75 years (1 point)] (15). This simple and easy to remember prediction model, demonstrated satisfactory calibration and discrimination for predicting technical failure using both antegrade and retrograde CTO techniques, and categorized CTO procedures into four groups with increased difficulty and reduced likelihood of success.
Finally, Liu et al. (16) developed a risk scoring system [age ≥75 years (1 point), left ventricular ejection fraction (LVEF) <40% (1 point) and baseline serum creatinine (SCr) >1.5 mg/dL (2 points)] with similar accuracy to Mehran score for predicting contrast induced nephropathy after CTO PCI.
Conclusions
In conclusion, to answer to the title question, predictive scores are not only fashionable but also very useful tools to estimate the likelihood of GW crossing, the probability of procedural success and even clinical outcome after CTO PCI. Therefore, their use should be further expanded. The most difficult challenge for the operator is to clarify the multiple information given from different scores and to draw the right conclusions. Indeed, they could be even applied to select the appropriate candidates for PCI among CTO patients to ensure a better cardiovascular outcome.
Acknowledgements
None.
Footnote
Provenance: This is an invited Editorial commissioned by the Section Editor Yue Liu (Associate professor, Department of Cardiology, The First Affiliated Hospital of Harbin Medical University, Harbin, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Tomasello SD, Giudice P, Attisano T, et al. The innovation of composite core dual coil coronary guide-wire technology: A didactic coronary chronic total occlusion revascularization case report. J Saudi Heart Assoc 2014;26:222-5. [Crossref] [PubMed]
- Mashayekhi K, Behnes M, Akin I, et al. Novel retrograde approach for percutaneous treatment of chronic total occlusions of the right coronary artery using ipsilateral collateral connections: a European centre experience. EuroIntervention 2016;11:e1231-6. [Crossref] [PubMed]
- Galassi AR, Brilakis ES, Boukhris M, et al. Appropriateness of percutaneous revascularization of coronary chronic total occlusions: an overview. Eur Heart J 2015. [Epub ahead of print]. [PubMed]
- Galassi AR, Tomasello SD, Reifart N, et al. In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. EuroIntervention 2011;7:472-9. [Crossref] [PubMed]
- Boukhris M, Tomasello SD, Galassi AR. Should we give into temptation and attempt all chronic total occlusions? Interv Cardiol 2014;6:399-401. [Crossref]
- Galassi AR, Boukhris M, Azzarelli S, et al. Percutaneous Coronary Interventions for Chronic Total Occlusions: More Benefit for the Patient or for the Interventionist's Ego? Can J Cardiol 2015;31:974-9. [Crossref] [PubMed]
- Hoebers LP, Claessen BE, Elias J, et al. Meta-analysis on the impact of percutaneous coronary intervention of chronic total occlusions on left ventricular function and clinical outcome. Int J Cardiol 2015;187:90-6. [Crossref] [PubMed]
- Boukhris M, Elhadj ZI, Galassi AR. Chronic total improvement in ventricular function and survival. J Thorac Dis 2015;7:E222-5. [PubMed]
- Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009;360:961-72. [Crossref] [PubMed]
- Nagashima Y, Iijima R, Nakamura M, et al. Utility of the SYNTAX score in predicting outcomes after coronary intervention for chronic total occlusion. Herz 2015;40:1090-6. [Crossref] [PubMed]
- Morino Y, Abe M, Morimoto T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv 2011;4:213-21. [Crossref] [PubMed]
- Opolski MP, Achenbach S, Schuhbäck A, et al. Coronary computed tomographic prediction rule for time-efficient guidewire crossing through chronic total occlusion: insights from the CT-RECTOR multicenter registry (Computed Tomography Registry of Chronic Total Occlusion Revascularization). JACC Cardiovasc Interv 2015;8:257-67. [Crossref] [PubMed]
- Alessandrino G, Chevalier B, Lefèvre T, et al. A Clinical and Angiographic Scoring System to Predict the Probability of Successful First-Attempt Percutaneous Coronary Intervention in Patients With Total Chronic Coronary Occlusion. JACC Cardiovasc Interv 2015;8:1540-8. [Crossref] [PubMed]
- Christopoulos G, Kandzari DE, Yeh RW, et al. Development and Validation of a Novel Scoring System for Predicting Technical Success of Chronic Total Occlusion Percutaneous Coronary Interventions: The PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) Score. JACC Cardiovasc Interv 2016;9:1-9. [Crossref] [PubMed]
- Galassi AR, Boukhris M, Azzarelli S, et al. Percutaneous Coronary Revascularization for Chronic Total Occlusions. A Novel Predictive Score of Technical Failure Using Advanced Technologies. J Am Coll Cardiol Intv 2016. doi: [Crossref]
- Liu Y, Liu YH, Chen JY, et al. A simple pre-procedural risk score for contrast-induced nephropathy among patients with chronic total occlusion undergoing percutaneous coronary intervention. Int J Cardiol 2015;180:69-71. [Crossref] [PubMed]
- Christopoulos G, Wyman RM, Alaswad K, et al. Clinical Utility of the Japan-Chronic Total Occlusion Score in Coronary Chronic Total Occlusion Interventions: Results from a Multicenter Registry. Circ Cardiovasc Interv 2015;8:e002171. [Crossref] [PubMed]
- Nombela-Franco L, Urena M, Jerez-Valero M, et al. Validation of the J-chronic total occlusion score for chronic total occlusion percutaneous coronary intervention in an independent contemporary cohort. Circ Cardiovasc Interv 2013;6:635-43. [Crossref] [PubMed]
- Galassi AR, Sianos G, Werner GS, et al. Retrograde Recanalization of Chronic Total Occlusions in Europe: Procedural, In-Hospital, and Long-Term Outcomes From the Multicenter ERCTO Registry. J Am Coll Cardiol 2015;65:2388-400. [Crossref] [PubMed]
- Li Y, Xu N, Zhang J, et al. Procedural success of CTO recanalization: Comparison of the J-CTO score determined by coronary CT angiography to invasive angiography. J Cardiovasc Comput Tomogr 2015;9:578-84. [Crossref] [PubMed]
- Chen Y, Lu B, Hou ZH, et al. Predicting successful percutaneous coronary intervention in patients with chronic total occlusion: the incremental value of a novel morphological parameter assessed by computed tomography. Int J Cardiovasc Imaging 2015;31:1263-9. [Crossref] [PubMed]
- Christopoulos G, Karmpaliotis D, Alaswad K, et al. The efficacy of "hybrid" percutaneous coronary intervention in chronic total occlusions caused by in-stent restenosis: insights from a US multicenter registry. Catheter Cardiovasc Interv 2014;84:646-51. [Crossref] [PubMed]


