
Early computed tomography after extracorporeal cardiopulmonary resuscitation on in-hospital survival: a retrospective cohort study
Highlight box
Key findings
• Early computed tomography (CT) scans after extracorporeal cardiopulmonary resuscitation (ECPR) are not associated with improved in-hospital survival. The transportation of these patients carries many risks.
What is known and what is new?
• The transfer of patients after ECPR to a CT room is very risky.
• The performance of an early CT scan after ECPR was not associated with improved in-hospital survival.
What is the implication, and what should change now?
• A targeted CT scan strategy after ECPR is preferable to the routine performance of full-body CT scans.
Introduction
Several groups of researchers have investigated the role of early computed tomography (CT) scans after cardiopulmonary resuscitation (CPR) (1-3). However, the role of early CT scans after extracorporeal cardiopulmonary resuscitation (ECPR) has not been thoroughly investigated. Early full-body scans led to the identification of many abnormalities, of which many were correlated with in-hospital survival, such as bleeding, malposition of extracorporeal membrane oxygenation (ECMO) tube (4). However, transferring ECPR patients to a CT room is a high-risk procedure which may increase the possibility of elevated mortality (5-8). Thus, the decision to perform a CT scan should be made based on a careful consideration of the associated risks and benefits. In our centers if the cause of the cardiac arrest is unclear, early CT scans will be considered, if patients hemodynamic is unstable, early CT scans may not be considered. We performed this study to evaluate the benefits of early CT scanning on in-hospital survival and the risks of transporting patients who have undergone ECPR. We hypothesized that early CT scans after ECPR would indirectly improve in-hospital survival. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-43/rc).
Methods
Study cohort
This was a retrospective, 2 center, observational study of patients who had undergone ECPR at the Jinhua Municipal Central Hospital and Hangzhou First People’s Hospital between September 2014 and January 2022. A computerized search of the electronic medical records systems of the hospitals was conducted to identify eligible patients, and each case was then manually reviewed. All the patients who had undergone venoarterial ECMO (VA-ECMO) were screened, and those who had undergone ECPR were included in the analysis. One hundred and thirty-two patients who had undergone ECPR were included in this study. Baseline factors included gender, age, ECPR location, cause of cardiac arrest, initial shockable rhythm, CPR duration, ECMO duration and Sequential Organ Failure Assessment (SOFA) score were collected. The main outcome was in-hospital survival. These patients were then matched in terms of age, initial shockable rhythm, SOFA score, CPR duration, ECMO duration, percutaneous intervention, and cardiac arrest location. The informed consent was waived because of the retrospective nature of the study. This study was approved by the Ethics Review Board of Jinhua Municipal Central Hospital (No. 2020-291). Hangzhou First People’s Hospital was informed and agreed with this study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
ECPR algorithm
Under the institutions’ protocols for managing in-hospital cardiac arrest, the implementation of ECPR is required for patients who have undergone conventional CPR for >15 minutes without the return of spontaneous circulation. Relative contraindications to ECPR include unwitnessed cardiac arrest, non-shockable initial rhythm, advanced age, a long CPR duration (>60 min), and trauma. Final decisions were informed by the family and our ECMO team, which included 5 experienced physicians and 4 nurses. Cannulation was performed immediately at the bedside under ultrasound guidance. Patients transported to the emergency department after having an out-of-hospital cardiac arrest were always cannulated in the emergency room or catheter lab. The same relative contraindications as those for in-hospital cardiac arrest patients were applied.
ECMO cannulation and maintenance
Cannulation during ECPR was performed at the site of cardiac arrest by 2 experienced intensivists and 2 nurses under ultrasound guidance. Either a SORIN SCPC (London, UK) or MAQUET (Rastatt, Germany) system was used. The venous cannulas were 21–26 Fr [MAQUET or Edwards (Santa Ana, USA)] in diameter, while the arterial (returning) cannulas were 15–18 Fr [MAQUET, Edwards, or Medtronic (Minneapolis, USA)] in diameter. Intravenous unfractionated heparin was generally administered for anticoagulation with a target activated clotting time of 160–200 s. The intensivists decided on the management of vasopressors, fluids, ECMO flow, and withdrawal time, and decannulation was mainly performed based on each patient’s cardiac function.
Early CT scanning after ECPR
We defined early CT scanning as the performance of a CT scan following ECPR. Almost all of the patients underwent a CT scan within 1 hour of ECPR. For the in-hospital cardiac arrest patients, decisions concerning CT scans were based on the following factors: whether the cause for collapse was known, CPR duration, pre-CPR CT scan results, and suspected pulmonary embolism or haemorrhagic shock. Most of the patients only underwent brain and chest CT scans. Decisions to perform full-body CT scans on a minority of our patients were made by the physician in charge based on specific patient characteristics. For the out-of-hospital cardiac arrest patients, the main purpose of the CT scans was to identify the causes of cardiac arrest. The CT scans were interpreted by radiologists. For this study, we collected the radiologists’ reports, and our intensivists retrospectively assessed them.
Statistical analysis
SPSS (Version 22, IBM Statistics) and R (Version 3.6.3) were used for the data analysis. The data are presented as the mean ± standard deviation for the continuous variables and the number and percentage for the categorical variables. The Kolmogorov-Smirnov test was used to test for normality; a P value >0.1 indicated a normal distribution. Differences between the 2 independent groups were assessed by a 2 independent samples t-test or Mann-Whitney U-test for the continuous variables and by a Fisher’s exact test or Pearson’s χ2 test for the categorical variables. Kaplan-Meier curves were used to describe the in-hospital survival of patients who had undergone early CT scanning (the treatment group) and those who had not (the control group). Log-rank tests were used to assess the statistical significance of any differences. Multiple Cox regression analysis was used to investigate the factors associated with in-hospital survival. A P value <0.05 was considered statistically significant.
Results
Patient cohort
Of the 396 patients who were identified as having undergone VA-ECMO at our institutions during the study period, 132 had undergone ECPR (Figure 1). Among the 132 patients included in the analysis, 71 were in the treatment group and 61 were in the control group. The treatment group comprised 53.5% males and 46.5% females. The medium age of the treatment group patients was 46.3±15.7 years and that of the control group patients was 50.0±12.3 years. 67.6% of the 71 patients had been transferred from the emergency department and 39.4% cause of cardiac arrest was myocardial infarction. The median CPR duration was 30.3±8.9 min in the treatment group, which was longer than that in the control group (27.5±10.9 min; P=0.106). The median ECMO duration was 126.7±43.4 h in the treatment group and 124.7±45.4 h in the control group. Patients’ characteristics are shown in Table 1.
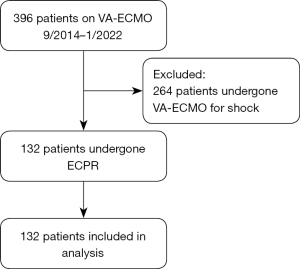
Table 1
| Variables | Treatment (n=71) | Control (n=61) | P value |
|---|---|---|---|
| Gender | 0.947 | ||
| Male | 38 (53.5) | 33 (54.1) | |
| Female | 33 (46.5) | 28 (45.9) | |
| Age (years) | 46.3±15.7 | 50.0±12.3 | 0.124 |
| ECPR location | 1.000 | ||
| Emergency room | 48 (67.6) | 28 (45.9) | |
| Catheter lab | 10 (14.1) | 13 (21.3) | |
| Intensive care unit | 6 (8.5) | 15 (24.6) | |
| Other departments | 7 (9.9) | 5 (8.2) | |
| Out of hospital | 31 (43.7) | 25 (41.0) | 0.860 |
| Cause of cardiac arrest | 1.000 | ||
| Myocardial infarction | 28 (39.4) | 30 (49.2) | |
| Myocarditis | 12 (16.9) | 11 (18.0) | |
| Pulmonary embolism | 20 (28.2) | 14 (23.0) | |
| Unknown etiology | 11 (15.5) | 6 (9.8) | |
| Initial shockable rhythm | 46 (64.8) | 47 (77.0) | 0.132 |
| CPR duration (min) | 30.3±8.9 | 27.5±10.9 | 0.106 |
| ECMO duration (h) | 126.7±43.4 | 124.7±45.4 | 0.792 |
| SOFA score | 13.9±2.7 | 13.2±2.7 | 0.088 |
| Outcome | 0.013 | ||
| Survival | 16 (22.5) | 26 (42.6) | |
| Death | 55 (77.5) | 35 (57.4) |
Data are presented as n (%) or mean ± standard deviation. ECPR, extracorporeal cardiopulmonary resuscitation; CPR, cardiopulmonary resuscitation; ECMO, extracorporeal membrane oxygenation; SOFA, sequential organ failure assessment score.
CT scan findings
Of the 71 patients, 49 underwent brain and chest CT scans and 22 underwent full-body CT scans. An average of 4.3±1.9 abnormalities per patient were identified, comprising 3.8±1.3 per patient in those who survived and 4.5±2.0 in those who died. Pulmonary infiltrates, oedema, and pleural effusions were the most common findings (98.6%) followed by cerebral oedema (60.6%). Intracranial bleeding occurred in 4 patients, ischemic stroke in 2, and brain herniation in 5. The differences in frequency of these 3 conditions did not differ significantly between those who survived and those who died.
As to the treatment of intracranial bleeding and ischemic stroke, the neurosurgeon was of the view that emergency surgery was unlikely to significantly improve patient prognosis and that this would be a high-risk procedure. Thus, with the agreement of their families, we merely adjusted the rate of administration of heparin and the activated clotting time target for these patients. Only 1 of these patients survived without any cerebral sequela. In the 71 patients, 8 types of thoracic problem were found, among which pulmonary embolism was the most common disorder requiring immediate intervention. Additionally, in 22 patients, 7 types of abdominal problems were found, none of which required immediate treatment. Complications occurred during transportation in 13 patients in the treatment group. These findings are set out in Table 2.
Table 2
| Variables | Incidence of finding | Survival with finding | Death with finding | P value |
|---|---|---|---|---|
| CT scan performed | 71 | 16 | 55 | |
| All findings | 4.3±1.9 | 3.8±1.3 | 4.5±2.0 | 0.408 |
| Brain | 1.4±1.0 | 1.3±0.9 | 1.4±1.1 | 0.986 |
| Chest | 2.4±1.0 | 2.1±0.9 | 2.5±0.9 | 0.201 |
| Abdomen | 0.5±1.0 | 0.4±0.7 | 0.6±1.0 | 0.674 |
| Details of findings | ||||
| Intracranial bleeding | 4 (5.6) | 1 (6.3) | 3 (5.5) | 1.000 |
| Ischemic stroke | 2 (2.8) | 0 (0.0) | 2 (3.6) | 1.000 |
| Cerebral edema | 43 (60.6) | 7 (43.8) | 36 (65.5) | 0.118 |
| Brain herniation | 5 (7.0) | 0 (0.0) | 5 (9.1) | 0.581 |
| Ethmoid sinusitis | 15 (21.1) | 1 (6.3) | 14 (25.5) | 0.163 |
| Sphenoiditis | 16 (22.5) | 8 (50.0) | 8 (14.5) | 0.006 |
| Maxillary sinusitis | 14 (19.7) | 3 (18.8) | 11 (20.0) | 1.000 |
| Rib fracture | 27 (38.0) | 4 (25.0) | 23 (41.8) | 0.223 |
| Sternal fracture | 8 (11.3) | 1 (6.3) | 7 (12.7) | 0.673 |
| Pulmonary infiltrates, edema, effusion | 70 (98.6) | 16 (100.0) | 54 (98.2) | 1.000 |
| Pulmonary embolism | 24 (33.8) | 7 (43.8) | 17 (30.9) | 0.339 |
| Cardiac enlargement | 9 (12.7) | 2 (12.5) | 7 (12.7) | 1.000 |
| Pericardial effusion | 19 (26.8) | 4 (25.0) | 15 (27.3) | 1.000 |
| Gallstones | 9 (12.7) | 2 (12.5) | 7 (12.7) | 1.000 |
| Cholecystitis | 6 (8.5) | 0 (0.0) | 6 (10.9) | 0.326 |
| Hepatic cyst | 6 (8.5) | 2 (12.5) | 4 (7.3) | 0.611 |
| Liver cirrhosis | 9 (12.7) | 1 (6.3) | 8 (14.5) | 0.673 |
| Spleen hematomas | 7 (9.9) | 1 (6.3) | 6 (10.9) | 1.000 |
| Arteriostosis | 5 (7.0) | 0 (0.0) | 5 (9.1) | 0.581 |
| Myocardial calcification | 7 (9.9) | 0 (0.0) | 7 (12.7) | 0.337 |
| Lumbar fractures | 1 (1.4) | 1 (6.3) | 0 (0.0) | 0.225 |
| Thoracic vertebra fracture | 2 (2.8) | 0 (0.0) | 2 (3.6) | 1.000 |
| Complications during transportation | ||||
| ECMO blood flow drop | 3 (4.2) | 1 (6.3) | 2 (3.6) | 0.541 |
| ECMO catheter bent | 2 (2.8) | 1 (6.3) | 1 (1.8) | 0.402 |
| Oxygen saturation drop | 3 (4.2) | 1 (6.3) | 2 (3.6) | 0.541 |
| Blood pressure drop | 5 (7.0) | 2 (12.5) | 3 (5.5) | 0.314 |
Data are presented as n (%) or mean ± standard deviation. CT, computed tomography; ECPR, extracorporeal cardiopulmonary resuscitation; ECMO, extracorporeal membrane oxygenation.
Patient outcomes
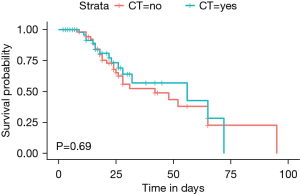
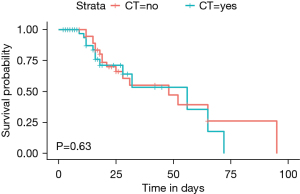
Of the 132 patients, 16 survived in the treatment group and 26 survived in the control group, and the difference was significant (P=0.013). Among the patients, 90 were matched in terms of age, initial shockable rhythm, SOFA score, CPR duration, ECMO duration, percutaneous intervention, and cardiac arrest location (45 in the treatment group and 45 in the control group). The results of the log-rank test showed that 13 patients survived in the treatment group and 17 survived in the control group, but this difference was not statistically significant (P=0.63). Multiple Cox regression analysis of in-hospital survival showed that early CT scan was not associated with improved in-hospital survival (P=0.357). The factors included in the matching mode and patients’ outcomes are shown in Table 3. Multiple Cox regression analysis are shown in Table 4. Survival curves before and after matching are shown in Figures 2,3.
Table 3
| Variables | Treatment (n=45) | Control (n=45) | P value |
|---|---|---|---|
| Gender | 1.000 | ||
| Male | 25 (55.6) | 25 (55.6) | |
| Female | 20 (44.4) | 20 (44.4) | |
| Age (years) | 48.1±15.5 | 48.1±11.9 | 0.548 |
| Initial shockable rhythm | 32 (71.1) | 34 (75.6) | 0.634 |
| SOFA | 13.7±2.6 | 13.4±2.8 | 0.550 |
| CPR duration | 28.3±7.5 | 28.9±11.6 | 0.764 |
| ECMO duration | 124.3±38.3 | 122.6±35.0 | 0.622 |
| PCI | 9 (20.0) | 9 (20.0) | 1.000 |
| Cardiac arrest location | 0.832 | ||
| In hospital | 24 (53.3) | 25 (55.6) | |
| Out of hospital | 21 (46.7) | 20 (44.4) | |
| Outcome | 0.371 | ||
| Survival | 13 (28.9) | 17 (37.8) | |
| Death | 32 (71.1) | 28 (62.2) |
Data are presented as n (%) or mean ± standard deviation. SOFA, sequential organ failure assessment score; CPR, cardiopulmonary resuscitation; ECMO, extracorporeal membrane oxygenation; PCI, percutaneous coronary intervention.
Table 4
| Variables | HR | 95% CI | P value |
|---|---|---|---|
| Early CT scan | 0.705 | 0.335–1.483 | 0.357 |
| Age | 0.991 | 0.967–1.015 | 0.445 |
| Initial shockable rhythm | 3.209 | 0.916–11.242 | 0.068 |
| SOFA score | 0.739 | 0.622–0.876 | 0.001 |
| CPR duration | 1.025 | 0.991–1.060 | 0.146 |
| ECMO duration | 0.983 | 0.974–0.993 | 0.000 |
| Percutaneous intervention | 1.146 | 0.527–2.491 | 0.731 |
| Cardiac arrest location | 2.453 | 1.090–5.522 | 0.030 |
HR, hazard ratio; CI, confidence interval; SOFA, sequential organ failure assessment score; CPR, cardiopulmonary resuscitation; ECMO, extracorporeal membrane oxygenation.
Discussion
Our findings did not support our hypothesis. Our major finding was that early CT after ECPR was not associated with improved in-hospital survival. This finding supports that of Yang et al, who found that the role of routine whole-body CT scanning after ECPR in patients who had out-of-hospital cardiac arrests was limited (9). Moreover, during transportation, our patients experienced many complications. Early CT scanning after ECPR identified many abnormalities, which could help clinicians to gain important information to guide clinical practice.
Transporting patients immediately after ECPR to the CT room carries a significant risk of adverse events (5-8). Thus, decisions to perform CT scans should be based on a careful consideration of the associated benefits and risks. The rationale for performing CT scans after CPR has always been to determine the causes of cardiac arrest or identify CPR-related injuries (2,10,11). However, the risks are greater after ECPR than after CPR, partly because, in the former case, the hemodynamic state is characteristically more unstable and disconnection of an ECMO catheter can be catastrophic.
At our institutions, the most common reason for CT scanning was an unknown cause of collapse, especially in patients who suffered cardiac arrest out of hospital. For patients suffered in-hospital cardiac arrest, the decision of an early CT scan would be based on the cause of cardiac arrest, CPR duration and hemodynamic situation. Another reason for CT scans at our institutions was pulmonary embolism, which is a dangerous condition that requires immediate intervention. Contrast-enhanced CT can help clarify the area of infarction, thus assisting physicians to determine the optimal subsequent treatment options. At our institutions, CPR duration was a third reason for CT scans. Patients who have undergone prolonged CPR always have a poorer prognosis and more complications (12,13). Favorable neurologic outcomes are less likely after prolonged CPR (14,15). Thus, performing a CT scan can help to determine the state of the brain and provide evidence for making treatment decisions.
Our findings support the ECPR guidelines of the Extracorporeal Life Support Organization, which recommend an individualized CT scan strategy for such patients (16). According to these guidelines, if the cause of the cardiac arrest is unclear, or if there is evidence of significant internal hemorrhage, CT scanning should be performed immediately after cannulation. A full-body CT scan is recommended to identify the cause of collapse; however, this investigation may not be necessary for patients with a clear cause of collapse (10,16). For example, if a cardiac arrest occurs in the intensive care unit (ICU), the CPR duration is short, and the patient has no history of brain disease, performing a CT scan immediately may not be the optimal course of action.
An early full-body CT scan is recommended after cardiac arrest associated with trauma (10,17,18). However, during ECPR, the situation is different. In patients who have undergone trauma, the purpose of CT scanning is to determine the location and severity of injuries. Trauma management treats the cause of cardiac arrest and can thus improve patient outcomes, while in the case of ECPR, treatment is more complex. Anticoagulation is the main impediment to advanced management, which is why many patients with intracranial bleeding do not undergo surgery.
Today, ultrasound is used more often in the ICU than it was in the past. Ultrasound can make many useful contributions, such as confirming the position of an ECMO catheter (19) and detecting CPR-related injuries by a standard or extended focused assessment with sonography in trauma examinations (20,21); thus, it is less urgent to perform a CT scan post-CPR than it used to be. Additionally, in patients with hemodynamic instability, ultrasound can provide acceptable imaging and has considerable advantages over CT (22). Given that patients always have hemodynamic instability after ECPR, an ultrasonic examination is likely to be preferable to an immediate CT scan.
This study had several limitations. First, as it was a retrospective study, the evidence is less reliable than that of a randomized controlled trial. However, conducting a randomized controlled trial in such patients could be problematic from an ethical perspective. Second, this study was relatively small. Indeed, the cohort comprised only 90 patients after propensity score matching. As the implementation of ECPR increases in our country, we will soon have more patients to investigate.
Conclusions
The in-hospital survival rate between early CT scan performed group and early CT scan not performed group was not different, even after propensity score matching analysis, however, the CT after ECPR could help clinicians to gain important information to guide clinical practice.
Acknowledgments
Funding: This work was supported by the Key Research and Development Project of Zhejiang Province (No. 2020C03019).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-43/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-43/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-43/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-43/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The informed consent was waived because of the retrospective nature of the study. This study was approved by the Ethics Review Board of Jinhua Municipal Central Hospital (No. 2020-291)
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Branch KRH, Strote J, Gunn M, et al. Early head-to-pelvis computed tomography in out-of-hospital circulatory arrest without obvious etiology. Acad Emerg Med 2021;28:394-403. [Crossref] [PubMed]
- Dunham GM, Perez-Girbes A, Bolster F, et al. Use of whole body CT to detect patterns of CPR-related injuries after sudden cardiac arrest. Eur Radiol 2018;28:4122-7. [Crossref] [PubMed]
- Karatasakis A, Sarikaya B, Liu L, et al. Prevalence and Patterns of Resuscitation-Associated Injury Detected by Head-to-Pelvis Computed Tomography After Successful Out-of-Hospital Cardiac Arrest Resuscitation. J Am Heart Assoc 2022;11:e023949. [Crossref] [PubMed]
- Zotzmann V, Rilinger J, Lang CN, et al. Early full-body computed tomography in patients after extracorporeal cardiopulmonary resuscitation (eCPR). Resuscitation 2020;146:149-54. [Crossref] [PubMed]
- Ericsson A, Frenckner B, Broman LM. Adverse Events during Inter-Hospital Transports on Extracorporeal Membrane Oxygenation. Prehosp Emerg Care 2017;21:448-55. [Crossref] [PubMed]
- Vieira J, Frakes M, Cohen J, et al. Extracorporeal Membrane Oxygenation in Transport Part 2: Complications and Troubleshooting. Air Med J 2020;39:124-32. [Crossref] [PubMed]
- Mendes PV, de Albuquerque Gallo C, Besen BAMP, et al. Transportation of patients on extracorporeal membrane oxygenation: a tertiary medical center experience and systematic review of the literature. Ann Intensive Care 2017;7:14. [Crossref] [PubMed]
- Austin DE, Burns B, Lowe D, et al. Retrieval of critically ill adults using extracorporeal membrane oxygenation: the nine-year experience in New South Wales. Anaesth Intensive Care 2018;46:579-88. [Crossref] [PubMed]
- Yang KJ, Wang CH, Huang YC, et al. Clinical experience of whole-body computed tomography as the initial evaluation tool after extracorporeal cardiopulmonary resuscitation in patients of out-of-hospital cardiac arrest. Scand J Trauma Resusc Emerg Med 2020;28:54. [Crossref] [PubMed]
- Nolan JP, Sandroni C, Böttiger BW, et al. European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: post-resuscitation care. Intensive Care Med 2021;47:369-421. [Crossref] [PubMed]
- Elfassy MD, Randhawa VK, Allan KS, et al. Understanding Etiologies of Cardiac Arrest: Seeking Definitional Clarity. Can J Cardiol 2022;38:1715-8. [Crossref] [PubMed]
- Arima T, Nagata O, Sakaida K, et al. Relationship between duration of prehospital resuscitation and favorable prognosis in ventricular fibrillation. Am J Emerg Med 2015;33:677-81. [Crossref] [PubMed]
- Jang SJ, Cha YK, Kim JS, et al. Computed tomographic findings of chest injuries following cardiopulmonary resuscitation: More complications for prolonged chest compressions? Medicine (Baltimore) 2020;99:e21685. [Crossref] [PubMed]
- Esdaille CJ, Coppler PJ, Faro JW, et al. Duration and clinical features of cardiac arrest predict early severe cerebral edema. Resuscitation 2020;153:111-8. [Crossref] [PubMed]
- Welbourn C, Efstathiou N. How does the length of cardiopulmonary resuscitation affect brain damage in patients surviving cardiac arrest? A systematic review. Scand J Trauma Resusc Emerg Med 2018;26:77. [Crossref] [PubMed]
- Richardson ASC, Tonna JE, Nanjayya V, et al. Extracorporeal Cardiopulmonary Resuscitation in Adults. Interim Guideline Consensus Statement From the Extracorporeal Life Support Organization. ASAIO J 2021;67:221-8. [Crossref] [PubMed]
- Lott C, Truhlář A, Alfonzo A, et al. European Resuscitation Council Guidelines 2021: Cardiac arrest in special circumstances. Resuscitation 2021;161:152-219. [Crossref] [PubMed]
- Krahn AD, Tfelt-Hansen J, Tadros R, et al. Latent Causes of Sudden Cardiac Arrest. JACC Clin Electrophysiol 2022;8:806-21. [Crossref] [PubMed]
- O’Neil ER, Coleman RD, Vogel AM, et al. Safely repositioning dual-lumen ECMO cannulas with a transfemoral lasso snare. Perfusion 2021;36:777-80. [Crossref] [PubMed]
- Montoya J, Stawicki SP, Evans DC, et al. From FAST to E-FAST: an overview of the evolution of ultrasound-based traumatic injury assessment. Eur J Trauma Emerg Surg 2016;42:119-26. [Crossref] [PubMed]
- Liu N, Roth KR, Nesbit DA, et al. Hemoperitoneum identified by focused assessment with sonography for trauma following cardiopulmonary resuscitation. Radiol Case Rep 2021;16:3987-9. [Crossref] [PubMed]
- Fornell Pérez R. Focused assessment with sonography for trauma (FAST) versus multidetector computed tomography in hemodynamically unstable emergency patients. Radiologia 2017;59:531-4. [PubMed]


