
Esophagram should be performed to diagnose esophageal perforation before inter-hospital transfer
Highlight box
Key Findings
• Of transferred patients, 36.9% were ultimately found to not have an esophageal perforation.
• Prior to transfer, esophagram was obtained in only 21.5% of patients.
• Of non-perforated transfers, 79.1% had a negative esophagram on arrival to receiving institution.
What is known and what is new?
• Esophagram has traditionally been viewed as the radiologic gold standard in the diagnosis of esophageal perforation, however is performed only 21.5% of the time prior to inter-hospital transfer.
• A significant number of unnecessary transfers may be able to be prevented by obtaining esophgram prior to transfer.
What is the implication, and what should change now?
• Whenever possible, esophagram should be performed prior to transfer.
• When traditional esophagram cannot be performed, providers should consider obtaining CT esophagram.
• In a clinically unstable or decompensating patient, transfer should not be delayed to obtain advanced imaging.
Introduction
Esophageal perforation is a rare surgical emergency with high morbidity and mortality. The pooled mortality risk is estimated to be 11.9%, and delays in diagnosis over 24 hours have been shown to double the mortality rate (1). Diagnosis of esophageal perforation can be challenging, and there are various approaches to evaluation (2). The management of esophageal perforation depends on several factors including timing from onset, etiology, and site of perforation. Treatment often involves advanced endoscopic procedures and/or thoracic surgery, often necessitating transfer to hospitals with larger resource pools. Importantly, treatment at high-volume institutions is associated with significant reductions in both 30- and 90-day mortality after perforation (3).
There is urgency to transfer patients with suspected esophageal perforation to a higher level of care since time to diagnosis and treatment significantly impact mortality (4,5). However, requirement of transfer has been previously demonstrated in various surgical populations to negatively impact patient outcomes. Specifically, transferred patients have been shown to utilize more resources, have poorer outcomes (6) and higher mortality (7), have an increased risk of intensive care unit (ICU) mortality (8), and require a longer length of hospital stay (9). The transfer of patients specifically with suspected esophageal perforation has not been well studied.
The purpose of this study was to evaluate patients transferred to our tertiary care institution for suspected esophageal perforation. We sought to describe this patient population and characterize the diagnosis and management of esophageal perforation in transfer patients. The results of this study will help to inform changes that may impact the efficiency and necessity of transfer in esophageal perforation patients. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1798/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was reviewed and deemed exempt by the Colorado Multiple Institutional Review Board (COMIRB; IRB Organization No. IORG0000433) and individual consent for this retrospective analysis was waived.
A retrospective review of patients transferred to our regional tertiary care institution from 2015–2021 was performed. We included patients ≥18 years of age who were accepted for transfer through our institution’s phone transfer service [calls between outside hospital (OSH) physicians and physicians at our institution are received and organized by a third party] by a thoracic surgeon at our institution. Patients with a suspected transfer diagnosis of esophageal perforation by chart review and DocLine record review were included.
Patient electronic health medical records were reviewed. The etiology of the perforation was reported; spontaneous esophageal perforations were defined as Boerhaave’s syndrome or perforation without any clearly identifiable underlying cause. Details of transferring institutions, including hospital bed number and presence of a cardiothoracic surgeon on staff, were discerned by critical website review. Transfer time was calculated from time of transfer acceptance to arrival at our institution. Transfer time of day was determined by the time of arrival. Values for elevated lactate (>1.6 mmol/L) and leukocytosis (>11.1×109/L) were determined by our institution’s standard lab values.
Statistical analysis
Bivariate comparisons were performed using the Wilcoxon-Mann-Whitney test for continuous variables and chi-squared or Fisher’s exact tests for categorical variables. Multivariable logistic regression was performed to identify factors associated with diagnosis. Covariate selection followed a two-step procedure. First, demographic and other pre-transfer variables that were associated with diagnosis with P<0.20 in bivariate analyses were selected as candidate variables from Tables 1-4. Candidate variables included American Society of Anesthesiology Physical Status Classification (ASA class), cigarette use, functional health status, prior cardiac surgery, pleural effusion on CT scan at the referring hospital, esophagram at our institution, transferring hospital size, transport route, transfer time, transfer patient status, leukocytosis, and elevated lactate. Several variables were re-categorized, combining small categories into similar categories, to improve model convergence. Stepwise selection with entry and exit criteria of P=0.05 was then performed to obtain the final model.
Table 1
| Patient characteristics | All patients transferred for suspected esophageal perforation (n=65) | Patients with esophageal perforation (n=41) | Patients without esophageal perforation (n=24) | P value |
|---|---|---|---|---|
| Patient age (years) | 56.0 (44.0–69.0) | 59.0 (48.0–69.0) | 54.0 (36.0–66.0) | 0.27 |
| Gender (female) | 36.9% [24] | 36.6% [15] | 37.5% [9] | 0.94 |
| BMI (kg/m2) | 0.98 | |||
| <18.5 | 4.6% [3] | 4.9% [2] | 4.2% [1] | |
| 18.5–24 | 43.1% [28] | 41.5% [17] | 45.8% [11] | |
| 25–29 | 23.1% [15] | 24.4% [10] | 20.8% [5] | |
| >30 | 27.7% [18] | 26.8% [11] | 29.2% [7] | |
| Unknown | 1.5% [1] | 2.4% [1] | – | |
| Charlson Comorbidity index | 2 [1–4] | 2 [1–4] | 1 [1–2.5] | 0.37 |
| ASA class | 0.01 | |||
| I | 6.2% [4] | 2.4% [1] | 12.5% [3] | |
| II | 27.7% [18] | 17.1% [7] | 45.8% [11] | |
| III | 33.8% [22] | 41.5% [17] | 20.8% [5] | |
| IV | 32.3% [21] | 39.0% [16] | 20.8% [5] | |
| Congestive heart failure | 4.6% [3] | 2.4% [1] | 8.3% [2] | 0.55 |
| Pulmonary hypertension | 1.5% [1] | 2.4% [1] | 0.0% [0] | >0.99 |
| CVA or TIA | 3.1% [2] | 4.9% [2] | 0.0% [0] | 0.53 |
| Dementia | 1.5% [1] | 2.4% [1] | 0.0% [0] | >0.99 |
| Cigarette use within 1 year of surgery | 15.4% [10] | 9.8% [4] | 25.0% [6] | 0.15 |
| Alcohol abuse | 0.48 | |||
| None | 80.0% [52] | 75.6% [31] | 87.5% [21] | |
| Current | 16.9% [11] | 19.5% [8] | 12.5% [3] | |
| Prior | 3.1% [2] | 4.9% [2] | 0.0% [0] | |
| Connective tissue disease | 1.5% [1] | 2.4% [1] | 0.0% [0] | >0.99 |
| Peptic ulcer disease | 15.4% [10] | 14.6% [6] | 16.7% [4] | >0.99 |
| Diabetes | 0.76 | |||
| None/diet controlled | 92.3% [60] | 92.7% [38] | 91.7% [22] | |
| Uncomplicated | 6.2% [4] | 4.9% [2] | 8.3% [2] | |
| End-organ damage | 1.5% [1] | 2.4% [1] | 0.0% [0] | |
| Hemiplegia | 1.5% [1] | 2.4% [1] | 0.0% [0] | >0.99 |
| Moderate to severe CKD | 1.5% [1] | 0.0% [0] | 4.2% [1] | 0.37 |
| Solid tumor | 0.70 | |||
| None | 95.4% [62] | 92.7% [38] | 100.0% [24] | |
| Localized | 1.5% [1] | 2.4% [1] | 0.0% [0] | |
| Metastatic | 3.1% [2] | 4.9% [2] | 0.0% [0] | |
| Venous thromboembolism | 1.5% [1] | 2.4% [1] | 0.0% [0] | >0.99 |
| Functional status | 0.03 | |||
| Independent | 76.9% [50] | 70.7% [29] | 87.5% [21] | |
| Partially dependent | 13.8% [9] | 22.0% [9] | 0.0% [0] | |
| Totally dependent | 9.2% [6] | 7.3% [3] | 12.5% [3] | |
| Prior thoracic surgery | 10.8% [7] | 9.8% [4] | 12.5% [3] | 0.70 |
| Prior cardiac surgery | 7.7% [5] | 12.2% [5] | 0.0% [0] | 0.15 |
| Prior abdominal surgery | 38.5% [25] | 34.1% [14] | 45.8% [11] | 0.35 |
Data are presented as median (interquartile range) or % [n]. ASA class, American Society of Anesthesiology Physical Status Classification; BMI, body mass index; CKD, chronic kidney disease; CVA, cerebrovascular accident; IQR, interquartile range; TIA, transient ischemic attack.
Table 2
| Diagnostic imaging | Percent of total patients in category (n=65) | Percent with esophageal perforation | P value |
|---|---|---|---|
| Esophagram at OSH | 0.46 | ||
| Not obtained | 78.5% [51] | 60.8% [31] | |
| Obtained | 21.5% [14] | 71.4% [10] | |
| Esophagram findings at OSH | 0.90 | ||
| Contained perforation | 15.4% [10] | 70.0% [7] | |
| Uncontained perforation | 6.2% [4] | 75.0% [3] | |
| Not obtained | 78.5% [51] | 60.8% [31] | |
| CT findings at OSH | 0.03 | ||
| Contained perforation | 24.6% [16] | 75.0% [12] | |
| Uncontained perforation | 20.0% [13] | 76.9% [10] | |
| Pneumomediastinum | 46.2% [30] | 56.7% [17] | |
| Not obtained | 3.1% [2] | 100.0% [2] | |
| No evidence of perforation | 6.2% [4] | 0.0% [0] | |
| Pleural effusion at OSH | <0.01 | ||
| Yes | 36.9% [24] | 83.3% [20] | |
| No | 60.0% [39] | 48.7% [19] | |
| Unknown | 3.1% [2] | 100.0% [2] | |
| Esophagram findings at UCH | <0.01 | ||
| Contained perforation | 13.8% [9] | 100.0% [9] | |
| Uncontained perforation | 10.8% [7] | 100.0% [7] | |
| No evidence of perforation | 30.8% [20] | 5.0% [1] | |
| Not obtained | 44.6% [29] | 82.8% [24] | |
| CT findings at UCH | 0.36 | ||
| Contained perforation | 6.2% [4] | 75.0% [3] | |
| Uncontained perforation | 1.5% [1] | 100.0% [1] | |
| No evidence of perforation | 6.2% [4] | 25.0% [1] | |
| Not obtained | 86.2% [56] | 64.3% [36] |
Data are presented as % [n]. CT, computed tomography; OSH, outside hospital; UCH, University of Colorado Hospital.
Table 3
| Transfer characteristics | Percent of total patients in category (n=65) | Percent with esophageal perforation | P value |
|---|---|---|---|
| Transferring hospital location | 0.39 | ||
| <50 miles | 23.1% [15] | 80.0% [12] | |
| 50–100 miles | 18.5% [12] | 66.7% [8] | |
| 101–300 miles | 32.3% [21] | 57.1% [12] | |
| >300 miles | 26.2% [17] | 52.9% [9] | |
| Transferring hospital size | 0.13 | ||
| Small (<100 beds) | 32.3% [21] | 47.6% [10] | |
| Medium (100–499 beds) | 63.1% [41] | 68.3% [28] | |
| Large (>499 beds) | 4.6% [3] | 100.0% [3] | |
| OSH cardiothoracic surgeon | 0.78 | ||
| Yes | 47.7% [31] | 61.3% [19] | |
| No | 52.3% [34] | 64.7% [22] | |
| Transfer transportation route | 0.02 | ||
| Ground | 35.4% [23] | 69.6% [16] | |
| Flight | 50.8% [33] | 69.7% [23] | |
| Unknown | 13.8% [9] | 22.2% [2] | |
| Transfer time of day | 0.51 | ||
| 6 am–6 pm | 24.6% [16] | 56.3% [9] | |
| 6 pm–6 am | 75.4% [49] | 65.3% [32] | |
| Day of transfer | 0.44 | ||
| Monday–Friday | 69.2% [45] | 60.0% [27] | |
| Saturday–Sunday | 30.8% [20] | 70.0% [14] | |
| Transfer time | 0.04 | ||
| <4 hours | 47.7% [31] | 77.4% [24] | |
| 4–12 hours | 23.1% [15] | 60.0% [9] | |
| >12 hours | 1.5% [1] | 0.0% [0] | |
| Unknown | 27.7% [18] | 44.4% [8] | |
| Transfer patient status | 0.09 | ||
| ICU | 81.5% [53] | 66.0% [35] | |
| Floor/telemetry | 13.8% [9] | 33.3% [3] | |
| Emergency department | 4.6% [3] | 100.0% [3] | |
| Intubated on arrival | 0.24 | ||
| No | 87.7% [57] | 59.6% [34] | |
| Yes | 12.3% [8] | 87.5% [7] | |
| Vasopressors on arrival | 0.40 | ||
| No | 90.8% [59] | 61.0% [36] | |
| Yes | 9.2% [6] | 83.3% [5] | |
| Leukocytosis (>11.1) on arrival | 0.15 | ||
| No | 30.8% [20] | 50.0% [10] | |
| Yes | 69.2% [45] | 68.9% [31] | |
| Elevated Lactate (>1.6) on arrival | <0.01 | ||
| No | 30.8% [20] | 40.0% [8] | |
| Yes | 36.9% [24] | 87.5% [21] | |
| Unknown | 32.3% [21] | 57.1% [12] |
Data are presented as % [n]. Details of patient transfer such as mode of transport, timing, distance. ICU, intensive care unit; OSH, outside hospital.
Table 4
| Surgical treatment | Esophageal perforation and surgery, % [n] |
|---|---|
| Incision type | 62.5% [15] |
| Thoracotomy | |
| Thoracoscopy | 16.7% [4] |
| Exploratory laparotomy | 45.8% [11] |
| Surgical treatment of perforation | 70.8% [17] |
| Repair of esophageal perforation | |
| Esophagectomy | 4.2% [1] |
| Jejunal or gastrostomy tube placement | 50.0% [12] |
| Other | 8.3% [2] |
| Confirmation of esophageal perforation intra-operatively | |
| Yes | 87.5% [21] |
| No | 12.5% [3] |
| Contamination found in abdomen | 16.7% [4] |
| Contamination found in chest | 75.0% [18] |
| Surgery timing | |
| Emergent (no delay) | 29.2% [7] |
| Urgent (within 24 hours transfer) | 50.0% [12] |
| Semi-elective | 20.8% [5] |
| Overall treatment of esophageal perforation | |
| Surgical | 58.3% [14] |
| Endoscopy followed by surgery | 20.8% [5] |
| Surgery followed by endoscopy | 20.8% [5] |
Results
A total of 65 patients who were transferred to our institution for suspected esophageal perforation were included in the dataset for analysis. Of the 65 transferred patients, 41 (63.1%) were confirmed to have esophageal perforation after arrival at our institution while 24 (36.9%) were found to have no esophageal perforation.
Patient characteristics
Table 1 compares the characteristics and comorbidities of transferred patients with confirmed esophageal perforation versus those who were not found to have a perforation at our institution. There were no significant differences in comorbidities between the groups. Patients with esophageal perforation had a higher ASA class than patients without perforation (ASA 3 41.5% versus 20.8%, ASA 4 39.0% versus 20.8%, P=0.01).
Esophageal perforation description
The most common etiology of suspected esophageal perforation was spontaneous (53.8%), followed by iatrogenic (33.8%). In those who were confirmed to have perforation after transfer, the most common causes remained spontaneous (48.8%) and iatrogenic (36.6%). Most patients (66.2%) were transferred less than 24 hours from suspected time of perforation. Esophageal perforation was most often thoracic in location (82.9%).
Diagnostic information
Table 2 shows the diagnostic imaging that was obtained before and after transfer. At the transferring OSH, a CT scan was obtained in almost all patients (96.9%). Pneumomediastinum was the least discriminatory finding on CT, seen in 46.2% of patients, of whom only 56.7% were ultimately found to have a perforation. While OSH CT evidence of contained or uncontained perforation was infrequently observed (24.6% and 20.0%, respectively), the majority of patients with those findings had a confirmed esophageal perforation upon arrival to our institution (75.0% and 76.9%, respectively). A false negative result on the OSH CT scan was not observed in any patients. However, one patient at our institution had CT scan falsely indicating no evidence of esophageal perforation, while a cervical perforation was ultimately found in the operating room.
An esophagram was obtained in only 21.5% of patients at the transferring institution. After transfer, 71% of patients with an esophagram at the OSH were found to have a perforation compared to 61% of those with no esophagram (P=0.46). Of patients with evidence of pleural effusion at the OSH, 83.3% were ultimately found to have a perforation. In patients who were found to have no perforation after transfer (n=24), this was most commonly confirmed at our institution by a negative esophagram in 79.2% of patients or a negative CT in 12.5%. Of the 24 patients who were determined to not have esophageal perforation following transfer, the final diagnoses included: pneumomediastinum (n=8, 33%), partial-thickness laceration (n=6, 25%), hiatal hernia (n=3, 13%), stricture (n=2, 8%) and esophagitis, pharyngeal abscess, hemothorax and gastro-broncho-pleural fistula related to prior Nissen (n=1, 4%, respectively).
Multiple regression
Lactate and ASA class were significant predictors of perforation. Patients with an elevated lactate on arrival to our institution were 11 times more likely to have an esophageal perforation (OR 11.3; 95% CI: 2.2, 57.2) versus those with a lactate value of 1.6 or below. Likewise, patients with an ASA class of 3–4 versus an ASA class of 1–2 were over six times more likely to have an esophageal perforation (OR 6.1; 95% CI: 1.7, 22.0).
Transfer information
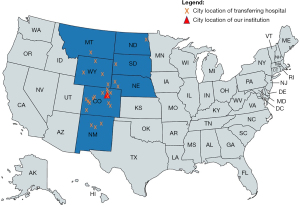
Table 3 shows the transfer information of patients accepted for suspected esophageal perforation. Reflective of our institution’s catchment size, many patients were transferred from a long distance, with 32.3% transferred from hospitals 100–300 miles away and 26.2% transferred from >300 miles away. Of patients transferred more than 100 miles (n=38), only 55.3% were found to have an esophageal perforation after transfer. Transfers were accepted from hospitals located in seven different states (Figure 1).
In patients with available transfer details, most were transferred by flight (50.8%) and arrived overnight between 6:00 pm and 6:00 am (75.4%). Transfer time was <4 hours in 47.7% of patients. Patients were most commonly classified as critical care status on transfer (81.5%). Transferring hospitals were often small (32.3% with <100 beds) or moderate (63.1% with 100–499 beds) in size, and 47.7% of hospitals had a cardiothoracic surgeon on staff.
Treatment of esophageal perforation
Table 4 outlines the treatment of patients who had surgery for esophageal perforation after arrival at our institution (n=24). In patients with an esophageal perforation who underwent an interventional procedure (n=24), 58.3% were treated with surgery alone, 20.8% had endoscopic intervention followed by surgery, and 20.8% required endoscopic intervention after surgery. Interestingly, 12.5% (n=3) were not found to have an esophageal perforation intra-operatively. One patient had gastric perforation, one had right hemothorax/hemomediastinum without perforation, and one had a pharyngeal perforation. Most patients with esophageal perforation underwent primary repair (70.8%) of the esophagus. Spillage and contamination from the perforation site into the chest was frequently noted (75.0%). A feeding jejeunostomy tube or feeding or decompressing gastrostomy tube was placed in 50.0% of patients. Operations were typically emergent (50.0%) or urgent (29.2%).
Outcomes
The median ICU length of stay was 4.0 days (IQR, 3.0–6.0) and median overall length of stay was 13.0 days (IQR, 9.0–24.0). In patients without esophageal perforation, the median ICU length of stay was 1.0 day (IQR, 0.0–2.0) and the median overall length of stay was 5.0 days (IQR, 2.0–7.0) (data not shown in table). The most common complications in patients with esophageal perforation were prolonged ventilation over 48 hours (14.7%), deep organ space infection (17.6%), and unplanned re-admission within 30 days (20.0%) (Table 5).
Table 5
| 30-day outcomes | Esophageal perforation and surgical/endoscopic intervention % (N=35) |
|---|---|
| ICU length of stay (days)1 | 4.00 (3.00–6.00) |
| Overall length of stay (days)1 | 13.00 (9.00–24.00) |
| 30-day mortality | 5.7% [2] |
| Acute respiratory distress syndrome | 2.9% [1] |
| Bronchopleural fistula | 2.9% [1] |
| Myocardial infarction | 0.0% [0] |
| Pulmonary embolism | 0.0% [0] |
| Unplanned reintubation | 11.8% [4] |
| Initial prolonged ventilation (>48 h) | 14.7% [5] |
| Pneumonia | 5.9% [2] |
| Acute renal failure | 0.0% [0] |
| Stroke | 0.0% [0] |
| Septic shock | 8.8% [3] |
| Deep incisional/organ space infection | 17.6% [6] |
| Superficial infection at surgical site | 0.0% [0] |
| Wound disruption | 2.9% [1] |
| VTE | 8.8% [3] |
| Unexpected ICU admit | 8.6% [3] |
| Unplanned readmit in 30 days | 20.0% [7] |
Data are presented as median (interquartile range) or % [n]. 1, length of stay reflects stay at our institution, and is presented as median and interquartile range. ICU, intensive care unit; VTE, venous thromboembolism.
Discussion
In this study, we retrospectively evaluated patients who were transferred to our tertiary care hospital for suspected esophageal perforation. Our results indicate that 36.9% of patients were ultimately determined to have no esophageal perforation following transfer. This was most commonly demonstrated by a negative esophagram on arrival to our institution (80%). Transfer distance was typically long, over 100 miles, and often by flight. Our findings indicate that transfer is resource intensive, and that an esophagram is a critical component in identifying patients who do not have esophageal perforation.
It should be immediately noted that in a clinically apparent or unstable patient, transfer to definitive surgical management of suspected perforation should not be delayed to obtain confirmatory imaging. Prior review of studies of esophageal perforations have identified several clinical predictive factors including subcutaneous emphysema, fever, tachypnea, tachycardia and hypotension that should increase suspicion. However, in a stable patient without obvious clinical signs or symptomatology, performing an esophagram at the transferring institution, when possible, may prevent unnecessary transfers as well as save time and associated costs related to excess, unnecessary care. In the 24 patients transferred to our institution who were found to not have a perforated viscus, 79.2% were found to have a negative esophagram. As such it is conceivable that obtaining an esophagram, in a clinically appropriate patient, may have prevented a substantial number of these transfers. Our recommendation for obtaining an esophagram prior to transfer when able is supported by previous studies. Ceppa et al. (10) reviewed patients transferred to their institution with suspected esophageal perforation. The authors found that a proportion (46%, n=33/71) of patients transferred due to pneumomediastinum were subsequently found to have no esophageal perforation on esophagram. In a review of patients with esophageal perforation, Brinster et al. recommend esophagram as the study of choice for diagnosis; if the esophagram is negative but clinical suspicion remains high, serial esophagram examination or esophagram with barium contrast may be required for diagnosis (11). Further, Minnich et al. recommend esophagram to evaluate for esophageal perforation, sometimes paired with a CT scan to evaluate for mediastinal or pleural fluid collections requiring drainage (12).
While esophagram has traditionally been viewed as the radiologic gold standard in the diagnosis of esophageal perforation (13), and is the standard at our institution, recent studies have refuted the necessity of esophagram. Haam et al. found that esophagram in patients with spontaneous pneumomediastinum is unnecessary, and that chest x-ray and CT scan provide sufficient radiographic diagnosis (14). Others find that in diagnosis of esophageal perforation, a CT scan provides appropriate evaluation (4,15); the sensitivity and specificity of CT scan with oral contrast was 100.0% and 79.8%, versus 77.8% and 98.9% for esophagram (16). While CT scan has excellent sensitivity, the low specificity is problematic when considering transfer of patients. In addition, adynamic CT imaging may not provide sufficient information about location or extent of perforation to guide endoscopic or surgical intervention. Another review found that diagnostic accuracy of both CT scan and esophagram was less than 40% (2), indicating the challenge in diagnosis of this condition. Additional data points beyond imaging may aid with diagnosis, with both elevated lactate and higher ASA class serving as predictors of esophageal perforation in the present study. Lactate has previously been shown to be an important predictor of mortality after peritonitis associated with bowel perforation (17). While ASA class was found to be a predictor of perforation, this classification is partly confounded by patients with a suspected or known esophageal perforation being assigned a higher pre-operative ASA class based on severity of illness.
It is important to consider potential barriers to obtaining an esophagram at certain institutions. In our experience, and similar to what others have noted (15), esophagram is not always possible to obtain at the OSH. If esophageal perforation is clinically suspected and an esophagram is unable to be obtained, the safest approach is to precipitously transfer the patient. The performance of an esophagram requires staffing with a radiology technologist and a radiologist, which can be burdensome, especially when needed outside of routine business hours. Although this poses challenges and often requires calling in extra staff, we believe the resources potentially saved from a lengthy patient transfer are crucial to consider. Unnecessary transfer is a significant cost burden to patients and has been well-studied in the trauma population. Inter-hospital transfer in the U.S. has been estimated to cost an additional $15.8 billion each year (18). One study found that trauma patients who were transferred and subsequently discharged within 24 hours (e.g., “secondary overtriage”) incurred mean additional costs of $5,917, which is a large percentage of the $8,047 average per-year per-person health expenditure (19). Importantly, the transfer distance associated with this cost was shorter than in our study at an average of 45 miles, and transfer by air was necessary in only 10% of patients.
It’s worth noting that when an esophagram is unable to be obtained, providers should consider obtaining a CT esophagram. A CT esophagram, different from a regular CT with contrast, is protocolized to provide more direct imaging evaluation of acute esophageal injuries such as traumatic hematomas, perforations and postoperative leaks, and has been shown to have a sensitivity and specificity of 77.7% and 94.3%, respectively, for esophageal perforation (20). CT esophagram may be more readily achievable in smaller, community hospitals and outside of business hours then a traditional esophagram and has the advantage of being able to diagnose extraesophageal conditions. Given that 96.9% of patients transferred to our institution had received a CT scan prior to transfer, it is conceivable that a CT esophagram could be added on to these studies. However, this is an adynamic study and subject to limitations as such. Importantly, esophageal perforation is not only a diagnosis of imaging, but based on history and clinical evaluation. In an unstable or declining patient, obtaining advanced imaging should not delay transfer for improved access to definitive treatment.
The strengths of this study include analysis of a diverse sample of patients with esophageal perforations of various etiologies and diagnostic approaches. Furthermore, our this study provides an example of the magnitude of resources involved in transferring patients given the geographic size of our catchment area. There are several limitations to this study, including the retrospective nature and the potential for missed patients who were transferred for management of esophageal perforation without consultation to thoracic surgery, such as to the trauma/acute care surgery team or an intensive care unit. It is also possible that some small, contained perforations seen initially at the OSH were no longer visible on imaging or not clinically meaningful after transfer and thus the thoracic surgeon was not consulted, although this number is likely small. In addition, obtaining complete transfer records was sometimes difficult, and thus OSH diagnostic information or transfer details were occasionally missing. We did not have diagnostic information for patients who were not transferred from OSHs (e.g., those who had a negative esophagram prior to initiation of transfer), thus we were unable to calculate a reliable positive predictive or negative predictive value for OSH imaging, including esophagram. We also did not evaluate how many OSHs have the capability of performing esophagrams at the time of transfer, or have the site-specific sensitivity/specificity/AUROC for diagnostic tests performed at the OSHs. Regarding the use of step-wise logistic regression analysis, at present forward selection is the standard way to look at the importance of predictive variables, however criticism exists regarding the problem of multiple hypothesis testing, rates of error and issues of collinearity. The decision to use forward selection was made due to its computational feasibility, however limitations of this analysis should be considered.
Conclusions
The findings of this study support obtaining an esophagram for the evaluation of suspected esophageal perforation prior to hospital transfer. We found that many patients with suspected perforation were ultimately found to have no esophageal perforation, indicating that transfer could have been avoided. While all patients should ideally undergo esophagram at the referring institution, we acknowledge this may not be possible due to limited availability of resources and need for expedient treatment of patients with esophageal perforations. This recommendation is especially relevant for tertiary care centers that accept patients from a great distance, as this incurs significant resources, time, and cost both to the patient and hospital.
Acknowledgments
This study was presented at ACS Annual Meeting 10/2022. The authors thank Michael Bronsert, PhD, MS, for his statistical methodology consultation.
Funding: This study was funded by an internal grant from the Surgical Outcomes and Applied Research Program, Department of Surgery, University of Colorado School of Medicine.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1798/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1798/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1798/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1798/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was reviewed and deemed exempt by the Colorado Multiple Institutional Review Board (COMIRB; IRB Organization No. IORG0000433) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Biancari F, D'Andrea V, Paone R, et al. Current treatment and outcome of esophageal perforations in adults: systematic review and meta-analysis of 75 studies. World J Surg 2013;37:1051-9. [Crossref] [PubMed]
- Sdralis EIK, Petousis S, Rashid F, et al. Epidemiology, diagnosis, and management of esophageal perforations: systematic review. Dis Esophagus 2017;30:1-6. [Crossref] [PubMed]
- Markar SR, Mackenzie H, Wiggins T, et al. Management and Outcomes of Esophageal Perforation: A National Study of 2,564 Patients in England. Am J Gastroenterol 2015;110:1559-66. [Crossref] [PubMed]
- Zimmermann M, Hoffmann M, Jungbluth T, et al. Predictors of Morbidity and Mortality in Esophageal Perforation: Retrospective Study of 80 Patients. Scand J Surg 2017;106:126-32. [Crossref] [PubMed]
- Puerta Vicente A, Priego Jiménez P, Cornejo López MÁ, et al. Management of Esophageal Perforation: 28-Year Experience in a Major Referral Center. Am Surg 2018;84:684-9. [Crossref] [PubMed]
- Crippen CJ, Hughes SJ, Chen S, et al. The impact of interhospital transfers on surgical quality metrics for academic medical centers. Am Surg 2014;80:690-5. [Crossref] [PubMed]
- Castillo-Angeles M, Uribe-Leitz T, Jarman M, et al. Transferred Emergency General Surgery Patients Are at Increased Risk of Death: A NSQIP Propensity Score Matched Analysis. J Am Coll Surg 2019;228:871-7. [Crossref] [PubMed]
- Arthur KR, Kelz RR, Mills AM, et al. Interhospital transfer: an independent risk factor for mortality in the surgical intensive care unit. Am Surg 2013;79:909-13. [Crossref] [PubMed]
- Lucas DJ, Ejaz A, Haut ER, et al. Interhospital transfer and adverse outcomes after general surgery: implications for pay for performance. J Am Coll Surg 2014;218:393-400. [Crossref] [PubMed]
- Ceppa DP, Rosati CM, Chabtini L, et al. Development of a Multidisciplinary Program to Expedite Care of Esophageal Emergencies. Ann Thorac Surg 2017;104:1054-61. [Crossref] [PubMed]
- Brinster CJ, Singhal S, Lee L, et al. Evolving options in the management of esophageal perforation. Ann Thorac Surg 2004;77:1475-83. [Crossref] [PubMed]
- Minnich DJ, Yu P, Bryant AS, et al. Management of thoracic esophageal perforations. Eur J Cardiothorac Surg 2011;40:931-7. [PubMed]
- Backer CL, LoCicero J 3rd, Hartz RS, et al. Computed tomography in patients with esophageal perforation. Chest 1990;98:1078-80. [Crossref] [PubMed]
- Haam SJ, Lee JG, Kim DJ, et al. Oesophagography and oesophagoscopy are not necessary in patients with spontaneous pneumomediastinum. Emerg Med J 2010;27:29-31. [Crossref] [PubMed]
- Morgan CT, Maloney JD, Decamp MM, et al. A narrative review of primary spontaneous pneumomediastinum: a poorly understood and resource-intensive problem. J Thorac Dis 2021;13:3721-30. [Crossref] [PubMed]
- Wei CJ, Levenson RB, Lee KS. Diagnostic Utility of CT and Fluoroscopic Esophagography for Suspected Esophageal Perforation in the Emergency Department. AJR Am J Roentgenol 2020;215:631-8. [Crossref] [PubMed]
- Jobin SP, Maitra S, Baidya DK, et al. Role of serial lactate measurement to predict 28-day mortality in patients undergoing emergency laparotomy for perforation peritonitis: prospective observational study. J Intensive Care 2019;7:58. [Crossref] [PubMed]
- Reimer AP, Schiltz N, Koroukian SM, et al. National incidence of medical transfer: patient characteristics and regional variation. J Health Hum Serv Adm 2016;38:509-28. [PubMed]
- Osen HB, Bass RR, Abdullah F, et al. Rapid discharge after transfer: risk factors, incidence, and implications for trauma systems. J Trauma 2010;69:602-6. [Crossref] [PubMed]
- Suarez-Poveda T, Morales-Uribe CH, Sanabria A, et al. Diagnostic performance of CT esophagography in patients with suspected esophageal rupture. Emerg Radiol 2014;21:505-10. [Crossref] [PubMed]


