
Development and validation of a pulmonary complications prediction model based on the Yang’s index
Highlight box
Key findings
• We constructed a prognostic model for pulmonary contusion severity.
• Yang’s index is an easy-to-use method for the evaluation of pulmonary contusion.
What is known and what is new?
• So far, a prognostic model for early and accurate prediction of traumatic pulmonary has not been developed.
• Our model has a good performance in identifying patients with pulmonary complications and can guide clinicians to make effective intervention.
What is the implication, and what should change now?
• Pulmonary contusion is not the only determining factor of pulmonary complications.
Introduction
Traumatic injuries occur at a high incidence and are among the leading causes of death in modern societies (1,2). Blunt pulmonary contusion is a commonly seen sequela following blunt chest trauma (3-5), with an incidence of over 50% among blunt chest trauma cases (6). Studies have shown that pulmonary contusion is a risk factor for the development of acute respiratory distress syndrome (ARDS), and is moreover reported to be a major cause of death (7,8). A contusion volume greater than 20% of the total lung volume is hereby reported to indicate an increased risk of pulmonary complications (9). The existing relevant prediction models rely excessively on dynamic indicators such as arterial blood gas (ABG) indicators, making it difficult to achieve real early prediction. The new method in this study is based on computed tomography (CT) images, which can be used to obtain the Yang’s index for evaluating the degree of lung contusion through simple calculations. Other objective indicators that can be collected at admission such as the severity of rib fracture, and severe comorbid fracture(s) (of the spine, pelvis, and/or femur), can also be used in predicting the pulmonary complications. This model can identify high-risk patients at an early stage. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-378/rc).
Methods
Study design
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics committee of Shanghai Sixth People’s Hospital (No. 2020-KY-034). Individual consent for this retrospective analysis was waived. The other 7 hospitals are informed and agreed with this study. This study is a retrospective analysis of anonymized patient data. The authors of this study are responsible for the accuracy and integrity of all data and analyses.
Study population
A retrospective analysis was performed on the clinical data of blunt chest trauma patients with pulmonary contusion admitted to the thoracic surgery departments of eight hospitals (Shanghai Jiao Tong University School of Medicine Affiliated Sixth People’s Hospital, Tianjin Hospital of Tianjin University, General Hospital of Southern Theater Command of PLA, Fuzhou Second Hospital, Shijiazhuang Third Hospital, the Third Xiangya Hospital of Central South University, Hong Hui Hospital of Xi’an Jiao Tong University, and Shanghai Ninth People’s Hospital of Shanghai Jiao Tong University School of Medicine) in China from January 2014 to June 2020. The inclusion criteria for this study were as follows: adult male or female patients aged 18–80 years with blunt thoracic trauma combined with pulmonary contusion who had chest CT within 72 hours of injury. The exclusion criteria were as follows: Glasgow Coma Scale <9; traumatic brain injury requiring neurosurgical intervention; abdominal trauma requiring emergency surgery; vertebral fractures combined with spinal cord injury; lung infection before injury; previous history of chronic lung diseases, such as pulmonary tuberculosis, bronchiectasis, emphysema, chronic bronchitis or chronic obstructive pulmonary disease (COPD); unilateral atelectasis; pleural effusion/haemothorax >30%.
In this study, a total of 9 dead patients were collected during the same period, among which 7 died within 48 hours after admission and 2 died after 48 hours. Through analysis, the causes of death were not related to pulmonary contusion, but mainly to cerebral hemorrhage or other organ hemorrhage and renal failure. To avoid statistical errors, these deaths were not included in this study.
In Stage One, cases from two tertiary referral centers for trauma treating over 1,000 patients with chest trauma annually—Shanghai Jiao Tong University School of Medicine Affiliated Sixth People’s Hospital and Tianjin Hospital of Tianjin University—were chosen as the training set for the model. In Stage Two, the test set consisted of patients with chest trauma from General Hospital of Southern Theater Command of PLA, Fuzhou Second Hospital, Shijiazhuang Third Hospital, the Third Xiangya Hospital of Central South University, Hong Hui Hospital of Xi’an Jiao Tong University, and Shanghai Ninth People’s Hospital of Shanghai Jiao Tong University School of Medicine.
Measurement and variables
The following variables were analyzed extracted from the electronic patient records and analyzed: age, sex, body mass index (BMI), smoking history, diabetes, mechanism of injury (MOI; e.g., fall from a great height, car accident, etc.), severe comorbid fracture(s) (of the spine, pelvis, and/or femur), Injury Severity Score (ISS), severity of pulmonary contusion (the Yang’s index), pulmonary atelectasis, rib fractures (number and whether they are unilateral/bilateral), surgical history of rib fractures and the primary outcome: pulmonary complications.
The pulmonary complications included pulmonary infection and respiratory failure. Images alone hardly differentiate between consolidation due to inflammation (i.e., pneumonia) and/or blunt trauma. In real life, there is a mix of the two phenomena. The pulmonary infection could be diagnosed if the patient was discovered to have: (I) fever ≥38 ℃; (II) cough, expectoration or aggravation in the original respiratory symptoms; (III) moist rales in the lung and (IV) the count of white blood cell ≥10×109/L or <4×109/L by routine blood test or pathogenic bacteria found in sputum culture. In addition to blood gas analysis as a diagnostic criterion for respiratory failure [partial pressure of oxygen (PaO2)/fraction of inspired oxygen (FiO2) ≤300 mmHg or PaO2 <60 mmHg], patients lacking blood gas analysis parameters were diagnosed with respiratory failure if tracheal intubation or tracheostomy was performed and mechanical ventilation was required for more than 24 hours after surgical operation.
Pulmonary contusion index
The pulmonary contusion volume was measured by three-dimensional reconstruction, according to methods developed by Dr. Yang. Theoretically, contusion volume can be calculated by measuring the long diameter of the contusion tissue in 3 dimensions (axial, coronal and sagittal), and the total lung volume can be determined in the same manner. Unilateral pulmonary contusion index = pulmonary contusion volume (a×b×c)/total lung volume (A×B×C) ×100%, with the Yang’s index defined as the sum of the unilateral pulmonary contusion indexes of both lungs, where A is the distance measured on the coronal plane between the top of the thorax at the carina and the top of the dome of the diaphragm on the same side. B is the vertical distance between the bottom of the posterior chest wall and the anterior chest wall at the level of the carina on the cross-section; and C is the horizontal distance between the lateral wall of the trachea and the opposite chest wall at the level of the carina on the cross-section. These measurements are as shown in Figure 1A,1B.
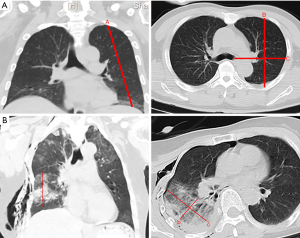
On the cross-sectional CT image, the pulmonary contusion volume can be calculated by multiplying the maximum diameters a, b, and c on the corresponding contusion tissue, where a is the maximum diameter of the contusion tissue perpendicular to the ground on the coronal plane, and the product of b and c represents the maximum cross-sectional area of the contusion tissue on the CT image, with b denoting the maximum vertical dimension of the contusion area on the plane and c expressing the maximum horizontal dimension of the contusion area on the plane.
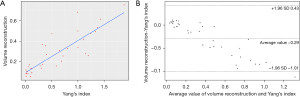
In case of a pulmonary contusion in multiple discontinuous areas, the sum of the pulmonary contusion index of each area should be calculated after the calculation of separate pulmonary contusion indexes respectively. The image of each patient was calculated and averaged by two radiologists with >5 years’ working experience in Imaging Department. For data with a great difference, the third senior doctor in Imaging Department should be consulted for joint discussion and further determination. The Yang’s index was proven to have a linear correlation with volume reconstruction.
Statistical analysis
R version 4.0.5 (The R Foundation for Statistical Computing, Vienna, Austria) was used for statistical analysis Continuous variables were expressed as medians and interquartile ranges. Categorical variables we represented as frequencies and percentages. Categorical variables were examined by the chi-squared test or Fisher’s exact test; comparisons between 2 continuous variables were performed with the Mann-Whitney U test, A two-tailed P value of <0.05 was considered statistically significant.
A linear correlation analysis and Bland-Altman approach were used to investigate the correlation and agreement between the Yang’s index and volume reconstruction. A prognostic model was constructed using logistic regression algorithms to predict adverse and severe adverse outcomes. Logistic regression algorithms were used to screen for risk factors related to adverse and severe adverse outcomes in patients with pulmonary contusion, and the risk factors included in this study were evidence-based on previous publications. A nomogram in predicting the probability of outcomes in patients with pulmonary contusion was obtained by the training set according to Occam’s Law of Razor, namely, the best model should be one that can achieve the aim of study with fewer variables.
Logistic regression-based predictions of outcomes were demonstrated by an alignment diagram, and the performance of the prediction model was evaluated in terms of sensitivity, specificity, accuracy, and area under the curve (AUC), receiver operating characteristic (ROC) analyses were performed to determine the best cut-off values to detect the outcome.
Results
Thirty-eight cases were used to evaluate the agreement of the Yang’s index and volume reconstruction. As shown by Figure 2A, the correlation was 0.857 (95% CI: 0.740–0.924). The Bland-Altman plot is shown in Figure 2B.
According to the inclusion and exclusion criteria, 515 patients were included in the subsequent predictive study, including 188 (36.5%) cases of pulmonary complications and 92 (17.86%) cases of respiratory failure. The training set comprised 363 patients, and the test set comprised 152 patients.
Table 1 summarizes the results of the univariate analysis of pulmonary complications and respiratory failure. ROC curves and alignment diagrams were plotted using the independent risk factors and indicators of potential clinical significance associated with pulmonary complications and respiratory failure. The prediction performance of the models is shown in Table 2, Figure 3A,3B, and Figure 4A,4B. Using the training set, models for pulmonary complications and respiratory failure were developed, and AUCs of 0.852 and 0.788 were achieved in the validation set. In the model performance for predicting pulmonary complications, the positive predictive value of the model is 0.938.
Table 1
| Factor | Training set | Testing set | |||||
|---|---|---|---|---|---|---|---|
| No | Yes | P value | No | Yes | P value | ||
| Pulmonary complications | N=255 | N=108 | N=72 | N=80 | |||
| Age, median (IQR) | 57.00 (50.00, 65.00) | 55.00 (49.00, 64.00) | 0.483 | 52.00 (48.00, 58.00) | 52.00 (44.75, 61.00) | 0.865 | |
| Sex, male, n (%) | 184 (72.16) | 80 (74.07) | 0.806 | 49 (68.06) | 68 (85.00) | 0.022 | |
| Smoking history, n (%) | 77 (30.20) | 31 (28.70) | 0.874 | 15 (20.83) | 10 (12.50) | 0.244 | |
| Diabetes, n (%) | 25 (9.80) | 25 (23.15) | 0.001 | 8 (11.11) | 6 (7.50) | 0.626 | |
| MOI, n (%) | 0.065 | 6.000 | <0.001 | ||||
| Fall from a great height | 20 (7.84) | 18 (16.67) | 15 (20.83) | 19 (23.75) | |||
| Car accident | 136 (53.33) | 52 (48.15) | 26 (36.11) | 45 (56.25) | |||
| Injury caused by falling object | 14 (5.49) | 8 (7.41) | 5 (6.94) | 12 (15.00) | |||
| Other | 85 (33.33) | 30 (27.78) | 26 (36.11) | 4 (5.00) | |||
| Comorbid fracture of the spine/pelvis/femur, n (%) | 49 (19.22) | 38 (35.19) | 0.002 | 11 (15.28) | 36 (45.00) | <0.001 | |
| Pulmonary atelectasis, n (%) | 162 (63.53) | 88 (81.48) | 0.001 | 23 (31.94) | 33 (41.25) | ||
| ISS, median (IQR) | 13.00 (9.00, 18.00) | 13.00 (9.00, 20.25) | 0.112 | 9.00 (4.00, 14.00) | 23.50 (18.00, 30.00) | <0.001 | |
| Rib fracture site, n (%) | 0.002 | <0.001 | |||||
| Unilateral | 194 (76.08) | 64 (59.26) | 55 (76.39) | 38 (47.50) | |||
| Bilateral | 61 (23.92) | 44 (40.74) | 17 (23.61) | 42 (52.50) | |||
| Number of fractured rib(s), %, median (IQR) | 7.00 (5.00, 9.00) | 8.00 (6.00, 13.00) | <0.001 | 6.00 (4.00, 8.00) | 9.00 (6.00, 11.00) | 0.001 | |
| Number of broken end(s) of rib fracture(s), %, median (IQR) | 8.00 (5.00, 12.00) | 12.00 (8.00, 16.00) | <0.001 | 7.00 (5.00, 10.00) | 13.00 (8.00, 18.00) | <0.001 | |
| Ratio of broken end(s) of rib fracture(s) to fractured rib(s), median (IQR) | 1.00 (1.00, 1.40) | 1.36 (1.09, 1.57) | <0.001 | 1.00 (1.00, 1.33) | 2.00 (1.12, 2.00) | <0.001 | |
| Internal fracture fixation, n (%) | 211 (82.75) | 97 (89.81) | 0.119 | 50 (69.44) | 68 (85.00) | 0.035 | |
| Yang’s index, median (IQR) | 14.60 (9.10, 28.00) | 22.40 (16.85, 40.62) | <0.001 | 12.85 (0.00, 21.72) | 53.05 (36.07, 75.10) | <0.001 | |
| Respiratory failure | N=339 | N=24 | N=84 | N=68 | |||
| Age, median (IQR) | 57.00 (50.00, 65.00) | 56.50 (50.75, 63.00) | 0.683 | 52.00 (48.00, 59.25) | 52.00 (44.75, 59.50) | 0.591 | |
| Sex, male, n (%) | 248 (73.16) | 16 (66.67) | 0.651 | 58 (69.05) | 59 (86.76) | 0.017 | |
| Smoking history, n (%) | 102 (30.09) | 6 (25.00) | 0.767 | 16 (19.05) | 9 (13.24) | 0.459 | |
| Diabetes, n (%) | 46 (13.57) | 4 (16.67) | 0.757 | 8 (9.52) | 6 (8.82) | 1.000 | |
| MOI, n (%) | 0.012 | <0.001 | |||||
| Fall from a height | 33 (9.73) | 5 (20.83) | 18 (21.43) | 16 (23.53) | |||
| Car accident | 174 (51.33) | 14 (58.33) | 33 (39.29) | 38 (55.88) | |||
| Blunt trauma | 19 (5.60) | 3 (12.50) | 5 (5.95) | 12 (17.65) | |||
| Other | 113 (33.33) | 2 (8.33) | 28 (33.33) | 2 (2.94) | |||
| Comorbid fracture of the spine/pelvis/femur, n (%) | 76 (22.42) | 11 (45.83) | 0.019 | 14 (16.67) | 33 (48.53) | 0.002 | |
| Pulmonary atelectasis, n (%) | 229 (67.55) | 21 (87.50) | 0.070 | 29 (34.52) | 27 (39.71) | 0.624 | |
| ISS, median (IQR) | 13.00 (9.00, 18.00) | 19.50 (13.00, 30.00) | <0.001 | 10.00 (4.75, 14.25) | 25.00 (20.75, 30.50) | <0.001 | |
| Rib fracture site, n (%) | 0.002 | 0.001 | |||||
| Unilateral | 248 (73.16) | 10 (41.67) | 62 (73.81) | 31 (45.59) | |||
| Bilateral | 91 (26.84) | 14 (58.33) | 22 (26.19) | 37 (54.41) | |||
| Number of fractured rib(s), %, median (IQR) | 7.00 (5.00, 9.00) | 11.50 (7.75, 14.00) | <0.001 | 6.50 (5.00, 8.00) | 9.00 (5.00, 11.00) | 0.007 | |
| Number of broken end(s) of rib fracture(s), %, median (IQR) | 9.00 (6.00, 13.00) | 14.00 (9.75, 19.00) | <0.001 | 8.00 (5.00, 10.25) | 14.00 (8.00, 20.00) | <0.001 | |
| Ratio of broken end(s) of rib fracture(s) to fractured rib(s), median (IQR) | 1.13 (1.00, 1.45) | 1.26 (1.17, 1.46) | 0.132 | 1.00 (1.00, 1.33) | 2.00 (1.54, 2.00) | <0.001 | |
| Internal fracture fixation n (%) | 290 (85.55) | 18 (75.00) | 0.232 | 60 (71.43) | 58 (85.29) | 0.065 | |
| Yang’s index, median (IQR) | 17.00 (10.05, 30.40) | 55.00 (19.65, 87.53) | <0.001 | 15.75 (2.45, 24.65) | 56.15 (39.09, 76.96) | <0.001 | |
IQR, interquartile range; MOI, mechanism of injury; ISS, Injury Severity Score.
Table 2
| Model | Cut-off | Sensitivity | Specificity | PPV | NPV | AUC |
|---|---|---|---|---|---|---|
| Model (A) | 0.397 | 0.563 | 0.958 | 0.938 | 0.663 | 0.852 |
| Model (B) | 0.2689 | 0.647 | 0.798 | 0.721 | 0.736 | 0.788 |
Model (A): model for predicting pulmonary complications; Model (B): model for predicting respiratory failure. PPV, positive predictive value; NPV, negative predictive value; AUC, area under the curve.


Discussion
Since pulmonary contusion has no highly specific, unique clinical symptoms, chest CT is considered to be the most reliable approach for diagnosing and monitoring this dynamic condition (10,11). Pulmonary contusion-induced edema and exudative effusion reach their peaks within 48–96 hours after injury (12). It is a highly complex, multifactorial phenomenon. In our study, pulmonary contusion indexes identifiable and quantifiable on CT performed within the first 3 days have been adopted as indicators to evaluate the severity of pulmonary contusion. There are two methods to evaluate pulmonary contusions based on CT images: clinicians may simply observe and interpret the CT images to evaluate the condition of the pulmonary lobes (13,14), which inevitably introduces subjectivity and substantial relative errors, or they may adopt a complex method with limited clinical application, i.e., volume reconstruction, to obtain precise measurements (4). Through stringent analysis of the chest CT findings in hundreds of patients with pulmonary contusion, a self-developed method, Yang’s index, was developed and introduced in this study. Yang’s index, which is linearly correlated with volume reconstruction, was demonstrated to have statistical significance and to help clinically evaluate pulmonary contusions; therefore, it is worthy of wide application and promotion in clinical practice.
In this study, diabetes, pulmonary atelectasis, severe comorbid fracture(s) (of the spine, pelvis and/or femur), severity of rib fracture(s), and the Yang’s index were found to be risk factors predicting pulmonary complications. The independent risk factors associated with pulmonary complications included diabetes, pulmonary atelectasis, severity of rib fracture(s) and the Yang’s index. These results suggested that patients with diabetes, severe comorbid fracture(s) (of the spine, pelvis and/or femur), or pulmonary atelectasis were at higher risk of pulmonary contusion an ideal environment for subsequent pulmonary infection. Although the ratio of pulmonary contusion volume to total lung volume is a significant cutoff value when predicting pulmonary complications (8,9,14), previous studies have reported that the prognosis of patients with chest trauma is affected by many other factors. Some researchers believe it is unnecessary to repeat chest imaging in patients with pulmonary contusion on initial imaging if they present without any clinical symptoms of respiratory compromise and that pulmonary contusion (PC) was infrequently clinically significant (15). Therefore, it is unwise to make prognosis of respiratory complications based solely on the presence or absence of pulmonary contusion on CT images alone. The Abbreviated Injury Scale (AIS) and ISS are based on overall considerations and lacks specificity on the severity of PC. Likewise, the Lung Organ Failure Score (LOFS) enables multifactorial prediction of respiratory failure in patients with chest trauma without taking pulmonary contusion into consideration (16). Moreover, we believe this method is not suitable for early prediction because of the unavailability of solid predictors upon admission. The Thoracic Trauma Severity (TTS) score can be used to evaluate the severity of chest trauma (17,18) and has been demonstrated to be a favorable method for predicting the occurrence of ARDS in patients with chest trauma (19). The TTS score focuses on the occurrence of ARDS, one of the pulmonary complications discussed in this study. According to the scoring system, PaO2/FiO2 and age are two important predictive factors; in fact, hypoxemia is not pronounced in some patients during the early onset of ARDS. In this retrospective study, continuous data on ABG and FiO2 were not available. A prediction model showing ideal performance was constructed using basic standard clinical data.
During early onset, PaO2/FiO2 is more of an indicator of the progression of lung damage than an independent prognostic factor. In the traditional prediction model of pulmonary complications, great importance has been attached to indicators of ABG. Undoubtedly, the result of ABG is one of the key indicators reflecting the progress or improvement of pulmonary diseases. Significantly, by using the prediction model established in this study, the prediction could be completed on the basis of the clinical objective data (excluding indicators of ABG) collected from patients at the time of admission, thus identifying high-risk patients who might develop pulmonary complications. In the model performance for predicting pulmonary complications, the positive predictive value of the model is 0.938, which means that the model has a good performance in identifying patients with pulmonary complications and can guide clinicians to make effective intervention.
Extensive evidence and common sense have shown that advanced age was an independent risk factor for poor prognosis in patients with severe chest trauma (20,21). However, the results of this study suggested that age was not a risk factor, which might be explained by the fact that the research participants included a number of younger adults who suffered from occupational or high-energy injuries, and that this study excluded elderly patients because of the presence of multiple underlying chronic conditions.
Our study results showed that the number of fractured rib(s) and the Yang’s index were two independent risk factors for respiratory failure. Numerous studies have indicated a correlation between the number of fractured rib(s) and poor prognosis in trauma patients (22,23). The presence of fractured ribs implies a severe high-energy MOI predisposing the patient to an underlying pulmonary contusion that is highly likely to be complicated with injuries in other locations. Patients with respiratory failure largely suffer from severe pulmonary contusions that progress rapidly and experience serious pathological effusion in their lung tissue. On this basis, multiple rib fractures cause intense pain, chest wall instability, limited expectoration, and worsening respiration, eventually resulting in respiratory failure in a short time. In this study, 59 patients required mechanical ventilation due to respiratory failure within 72 hours after chest trauma, representing 64% of all respiratory failure cases. Internal fixation of rib fractures remains controversial in the treatment of severe chest trauma complicated with pulmonary contusion (24-26). Although surgical treatment was not assessed as a risk factor for pulmonary complications, this treatment approach might help reduce the risk of respiratory failure or mitigate the long-term effects. Improved prognostic tools may help providers determine both the need for surgical intervention and identify the true clinical impact of PC in patients with concomitant severe chest wall injuries.
Limitations
This study had several limitations. As a retrospective study, important biochemical parameters were not available in every case for statistical analysis. To ensure data accuracy and integrity, these parameters were excluded from the study, which might impose limitations on the modeling results. In addition, this study had a relatively long study period but failed to include all patients meeting the inclusion criteria from the eight trauma centers; instead, patients with adverse outcomes were largely included in the study. The inclusion and exclusion criteria might also have introduced bias to the study results. Polytrauma patients are missing from the analysis, therefore the validity of the Yang’s index needs a much extensive, prospective observational study. For patients whose condition is complicated with severe hemopneumothorax, there is still no accurate strategy to evaluate the degree of pulmonary contusion owing to the significant changes in pulmonary volume, which remains to be further explored in the future.
Conclusions
In summary, a prognostic model for blunt chest trauma was successfully constructed based on the self-developed the Yang’s index in combination with the severity of chest trauma and other related clinical factors, and the prognostic model was demonstrated to have favorable prediction performance. The predictors were closely associated with clinical outcomes and could be collected upon admission to achieve early predictions and identification of high-risk patients and allow for pertinent treatment including aggressive physiotherapy, pain control and supportive therapy. The Yang’s index is an easy-to-use method for the accurate evaluation of pulmonary contusion severity and seems to be promising in a wider range of clinical application and decision making.
Acknowledgments
We thank the patients and the radiologists for their contribution to the study. The authors also appreciate the academic support from the AME Thoracic Surgery Collaborative Group.
Funding: The project was supported by the fund of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital (No. ynhg201919).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-378/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-378/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-378/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-378/coif). PG reports that he serves as a paid instructor and product development advisor for Zimmer Biomet and chest wall trauma division, the chairman for Chest Wall Injury Society and the History and Archives Committee (American College of Surgeons), also on the advisory board for Zimmer Biomet. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics committee of Shanghai Sixth People’s Hospital (No. 2020-KY-034), the other 7 hospitals are informed and agreed with this study. Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lanitis S, Kontovounisios C, Zafeiriadou P, et al. Epidemiology and management of trauma patients in a Greek multispecialty hospital in the absence of a dedicated trauma center. Eur J Trauma Emerg Surg 2013;39:369-74. [Crossref] [PubMed]
- The Lancet. Trauma: a neglected US public health emergency. Lancet 2016;388:2058. [Crossref]
- Eghbalzadeh K, Sabashnikov A, Zeriouh M, et al. Blunt chest trauma: a clinical chameleon. Heart 2018;104:719-24. [Crossref] [PubMed]
- Becher RD, Colonna AL, Enniss TM, et al. An innovative approach to predict the development of adult respiratory distress syndrome in patients with blunt trauma. J Trauma Acute Care Surg 2012;73:1229-35. [Crossref] [PubMed]
- Rendeki S, Molnár TF. Pulmonary contusion. J Thorac Dis 2019;11:S141-51. [Crossref] [PubMed]
- Dehghan N, de Mestral C, McKee MD, et al. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg 2014;76:462-8. [Crossref] [PubMed]
- Cohn SM. Pulmonary contusion: review of the clinical entity. J Trauma 1997;42:973-9. [Crossref] [PubMed]
- Beshay M, Mertzlufft F, Kottkamp HW, et al. Analysis of risk factors in thoracic trauma patients with a comparison of a modern trauma centre: a mono-centre study. World J Emerg Surg 2020;15:45. [Crossref] [PubMed]
- Miller PR, Croce MA, Bee TK, et al. ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients. J Trauma 2001;51:223-8; discussion 229-30. [Crossref] [PubMed]
- Tyburski JG, Collinge JD, Wilson RF, et al. Pulmonary contusions: quantifying the lesions on chest X-ray films and the factors affecting prognosis. J Trauma 1999;46:833-8. [Crossref] [PubMed]
- Gou J, Jiang Z, Wang P, et al. Diagnostic value of multi-slice spiral CT scan in lung compression ratio of patients with pulmonary contusion complicated by pneumothorax or hydropneumothorax. Am J Transl Res 2021;13:3004-9. [PubMed]
- Cohn SM, Dubose JJ. Pulmonary contusion: an update on recent advances in clinical management. World J Surg 2010;34:1959-70. [Crossref] [PubMed]
- Wagner RB, Jamieson PM. Pulmonary contusion. Evaluation and classification by computed tomography. Surg Clin North Am 1989;69:31-40. [Crossref] [PubMed]
- de Moya MA, Manolakaki D, Chang Y, et al. Blunt pulmonary contusion: admission computed tomography scan predicts mechanical ventilation. J Trauma 2011;71:1543-7. [Crossref] [PubMed]
- Požgain Z, Kristek D, Lovrić I, et al. Pulmonary contusions after blunt chest trauma: clinical significance and evaluation of patient management. Eur J Trauma Emerg Surg 2018;44:773-7. [Crossref] [PubMed]
- Wutzler S, Wafaisade A, Maegele M, et al. Lung Organ Failure Score (LOFS): probability of severe pulmonary organ failure after multiple injuries including chest trauma. Injury 2012;43:1507-12. [Crossref] [PubMed]
- Mommsen P, Zeckey C, Andruszkow H, et al. Comparison of different thoracic trauma scoring systems in regards to prediction of post-traumatic complications and outcome in blunt chest trauma. J Surg Res 2012;176:239-47. [Crossref] [PubMed]
- Pape HC, Remmers D, Rice J, et al. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma 2000;49:496-504. [Crossref] [PubMed]
- Daurat A, Millet I, Roustan JP, et al. Thoracic Trauma Severity score on admission allows to determine the risk of delayed ARDS in trauma patients with pulmonary contusion. Injury 2016;47:147-53. [Crossref] [PubMed]
- Zehr M, Klar N, Malthaner RA. Risk Score for Predicting Mortality in Flail Chest. Ann Thorac Surg 2015;100:223-8. [Crossref] [PubMed]
- Benjamin E, Recinos G, Aiolfi A, et al. Flail Chest: Less Deadly than Originally Thought. World J Surg 2018;42:3927-31. [Crossref] [PubMed]
- Shulzhenko NO, Zens TJ, Beems MV, et al. Number of rib fractures thresholds independently predict worse outcomes in older patients with blunt trauma. Surgery 2017;161:1083-9. [Crossref] [PubMed]
- Battle CE, Hutchings H, Evans PA. Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury 2012;43:8-17. [Crossref] [PubMed]
- Voggenreiter G, Neudeck F, Aufmkolk M, et al. Operative chest wall stabilization in flail chest--outcomes of patients with or without pulmonary contusion. J Am Coll Surg 1998;187:130-8. [Crossref] [PubMed]
- Jiang Y, Wang X, Teng L, et al. Comparison of the Effectiveness of Surgical Versus Nonsurgical Treatment for Multiple Rib Fractures Accompanied with Pulmonary Contusion. Ann Thorac Cardiovasc Surg 2019;25:185-91. [Crossref] [PubMed]
- Otaka S, Aso S, Matsui H, et al. Early Versus Late Rib Fixation in Patients With Traumatic Rib Fractures: A Nationwide Study. Ann Thorac Surg 2020;110:988-92. [Crossref] [PubMed]


