Survival impact of locoregional metachronous malignancy in survival of lung cancer patients who received curative treatment
Introduction
Malignancy is the leading cause of death worldwide. If distant metastases are confirmed initially, palliative treatment for disease control is the goal of treatment instead of curing the disease itself. When tumor tissue is localized within a limited region without vital structure invasion, en bloc tumor tissue removal is the core concept of anti-cancer therapy. Under these clinical scenarios, anatomic resection with regional lymph node (LN) dissection is the mainstay of therapy. Adjuvant therapy may be needed if locoregional LN invasion is confirmed by a pathologist. Regular surveillance with imaging tools is recommended because of the possibility of disease relapse. Metachronous malignancy of different origin may be identified incidentally during regular surveillance in cancer patients. The literature review shows that cancer survivors have increased risk of developing a second primary malignancy (1-8). The AIRTUM Working Group performed an epidemiologic study in Italy which showed that risk of metachronous primary malignancy in cancer patients was 10% higher than the general population in the average 14-year follow up (9). In Japan, Tabuchi et al. showed that metachronous secondary primary malignancy developed in 3.8% of cancer patients during a median follow-up of 2.5 years (10). Furthermore, cancer patients who develop secondary primary malignancy may have worse overall survival from the point of view of primary malignancy (4-7).
However, lung cancer population seems different. Brock et al. showed that lung cancer patients with a history of malignancy did not have a higher incidence of subsequent malignancy (11). Some studies have found that lung cancer patients with prior malignancy have better survival rates than those without a history of malignancy (11-13). In addition, Aziz et al. identified lung cancer patients who were diagnosed as secondary lung malignancy and received aggressive surgical intervention if the complete tumor survey revealed a resectable disease (12). Cancer survivors who were diagnosed with lung cancer as the first primary malignancy may present with earlier staging of the secondary lung cancer, as compared to those who were diagnosed with other malignancy first (14). There were no studies have documented lung cancer patients with metachronous malignancy and its survival impact in this population. In clinical practice, metachronous malignancy is also seen in the lung cancer population and can be identified before or after the diagnosis of lung cancer. If metachronous malignancy is loco-regional without vital structure invasion or distant metastases then surgical curative resection may be of benefit to cancer survivors. Hence, the aim of this study was to try to clarify the survival impact of locoregional metachronous malignancy in the lung cancer population with resectable disease from a pathology point of view.
Methods
Patients
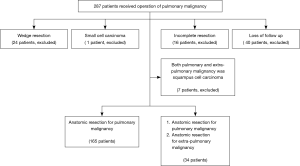
From January 2005 to December 2009, 287 lung cancer patients received operations in Chang Gung Memorial Hospital, of which only 199 patients who received anatomic resection of lung cancer were included into this study. Exclusion criteria included: (I) wedge resection due to poor pulmonary reserve (24 patients); (II) small cell lung cancer patients (1 patient); (III) patients with incomplete resection (stage IIIB or IV) (16 patients); and (IV) loss of follow up (40 patients). Additionally, seven patients were excluded because both pulmonary and extra-pulmonary malignancy was squamous cell carcinoma and because the relationship between these lesions could not identified by immuno-histo-chemical stain (Figure 1). One hundred and ninety-nine patients were enrolled and all curative therapy of lung cancer and underwent complete follow up longer than 5 years. Medical record data of these patients were retrospectively reviewed and clinico-pathologic factors were collected for further survival analysis. Informed content to patients was waived because of this study was a retrospectively study. All doctors who participated this study were gave informed consent in order to accordance study guideline. The cancer staging of patients followed the American Joint Cancer Conference (AJCC) 7th TNM staging definition. The institutional review was approved by the ethics committee of Chang Gung Memorial Hospital and Institutional Review Board number was 103-5631B.
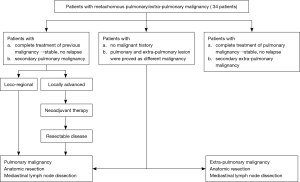
Management strategy (Figure 2)
For patients with previous malignancy and who received complete curative intent therapy, i.e., anatomic resection and further recommended adjuvant therapy, undetermined pulmonary lesions were identified in the regular follow up. Complete tumor workup was needed to evaluate the disease severity. Patients received chest computed tomography (CT), from the lower neck to the abdomen, in order to evaluate the pulmonary lesion and mediastinal LN status. In addition, bone scan or positron emission tomography (PET) was scheduled to rule out the possibility of distant metastases, except to the brain. Brain CT or magnetic resonance image (MRI) was utilized for evaluation of the brain in order to exclude brain metastases. Spirometry was also scheduled for each patient’s pulmonary reserve survey. For those without definite diagnosis after biopsy, surgical biopsy was done prior to anatomic resection. Resectability was evaluated after thorough image survey. For patients with resectable disease, anatomic resection and mediastinal LN dissection was done. For patients with locally advanced status of pulmonary malignancy, preoperative neoadjuvant therapy was given and resectability re-evaluation was carried out upon completion. Anatomic resection and mediastinal LN dissection were done if resectable disease was confirmed after neoadjuvant therapy.
For patients who were identified pulmonary and extra-pulmonary lesions at the same time, complete tumor workup is needed. Tissue proof of the both target sites were needed to obtain in order to confirm that there was no relationship between the pulmonary and extra-pulmonary lesions. Disease status was also evaluated completely with imaging tools. Distant metastases were excluded by PET and brain MRI and the patient’s pulmonary reserves were evaluated with spirometry. Surgical resection for both lesions was recommended only if pulmonary and extra-pulmonary malignancy were loco-regional invasion without distant metastases. Pulmonary malignancy was managed first with anatomic resection and mediastinal LN dissection. Another operation for synchronous malignancy was done after the patient recovered from pulmonary resection.
For patients with primary lung cancer after curative treatment but with identified metachronous extra-pulmonary lesion in the serial follow up program, complete tumor workup is warranted. Tissue proof of these lesions was needed and disease status was evaluated completely. Distant metastases were excluded by PET and brain MRI. Two important clinical presentations had to be meticulously evaluated, one being previous pulmonary malignancy status and the other being extra-pulmonary malignancy invasion status. Patients with locoregional invasion of extra-pulmonary malignancy and no evidence of relapse of pulmonary malignancy would receive anatomic resection of extra-pulmonary malignancy.
Operation and post-operation management
Anatomic resection, including lobectomy, bilobectomy, or pneumonectomy was done according to tumor invasion status. Mediastinal LN dissection was done after anatomic resection. All resected specimens, including tumors and mediastinal LNs were examined by pathologists. Post-operative planning was done according to final pathological stage and National Comprehensive Cancer Network (NCCN) guideline recommendations. Patients returned to the outpatient department every 3-month and CT was utilized as an imaging tool.
Statistics
All collected factors were analyzed by univariate analysis. Categorical variables were compared by chi-square or Fisher’s exact tests. Disease free survival was defined as the period between date of operation and relapse date or last follow up date without evidence of relapse. Overall survival was defined as the period between operation date and death date. Survival status was further analyzed and presented with a Kaplan-Meier curve. A P value less than 0.05 was considered statistically significant. All the analyses were performed using SAS, version 9 (SAS Institute, NC, USA).
Results
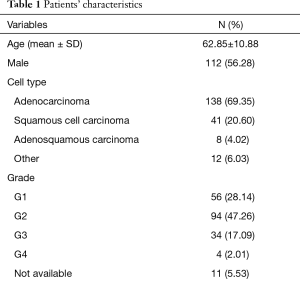
In this study, 199 patients who received curative therapy of lung cancer were enrolled. The mean age was 62.85 years and the patients were predominantly male (56%). In addition, 138 (69.35%) patients were identified as having adenocarcinoma and the mean tumor size was 3.4 cm. Visceral pleura and angiolymphatic invasion was identified in 101 patients (50.75%) and 78 patients (39.20%), respectively. There were 39 patients with locally advanced lung cancer who underwent pre-operative neoadjuvant therapy prior to surgical intervention and the majority (32/37, 82.1%) received clinical down-staging of anatomic resection and anatomic resection with mediastinal LN dissection was performed thereafter. A total of 138 patients (69.35%) received anatomic resection via thoracotomy. Other clinical characteristics of these patients are summarized in Table 1.
Full table
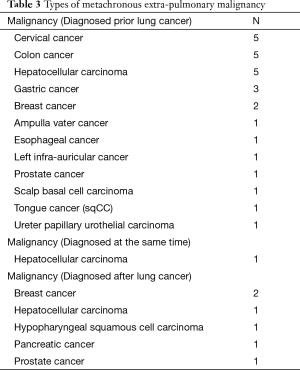
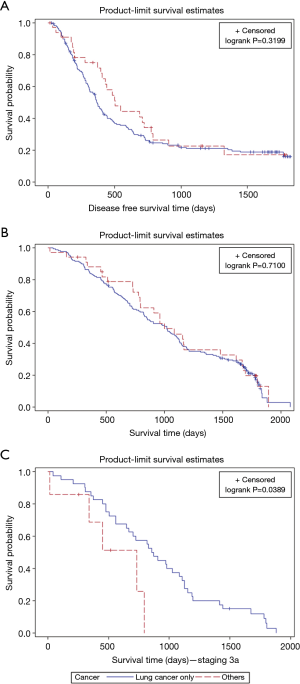
Of the total patients, 165 (82.9%) were diagnosed with lung cancer only (lung cancer group), while the remaining 34 patients (17.1%) were diagnosed with metachronous malignancy (metachronous malignancy group). There was no significant difference in clinical characteristics between the two groups (Table 2). Adenocarcinoma was predominant in both groups. Patients in the lung cancer group patients were of greater age (P=0.06) and had larger mean tumor size (P=0.06), although this did not reach statistical significance. Various metachronous malignancies were identified in the lung cancer patients and are summarized in Table 3. One patient was identified with two different malignancies at the same time. The disease free survival (P=0.3199) and overall survival (P=0.71) in these two groups showed no statistically significant difference (Figure 3A,B). We further analyzed survival impact according to pathologic stage of lung cancer in order to clarify the survival impact of metachronous malignancy in the lung cancer population. Metachronous malignancy only showed survival impact in lung patients with pathologic stage IIIA (Figure 3C; P=0.0389).

Full table
Full table
Discussion
It is not unusual for lung cancer patients to present with metachronous malignancy and may be encountered in clinical practice. There is no definite guideline to follow in these clinical scenarios. Hence, we focused on the survival impact of locoregional metachronous malignancy on survival of lung cancer patients who received curative treatment. From literature review, the definition of metachronous malignancy is not uniform and varies among different studies (9,10). For these patients, complete tumor workup is necessary in order to evaluate the lesion invasion status and relationship with prior malignancy. However, imaging tools have their own limitations because of the imaging conditions. For example, in lung cancer patients, agreement between the clinical and pathologic stages before and after PET was 21.7% and 67.2%, respectively (15-17). In order to eliminate the evaluation bias of imaging tools, we recruited patients from the pathologic view and all included patients had a definite pathology stage of pulmonary and extra-pulmonary malignancy. Radial resection with regional LN dissection was the mainstay for cancer treatment if the tumor was resectable. In this study, both pulmonary and extra-pulmonary malignancy was treated by radial resection with regional LN dissection and subsequent treatment recommendation (18). In order to eliminate the bias, 16 patients who received wedge resection and one small cell lung cancer patient were excluded. In addition, 40 patients were excluded due to loss of follow up. Furthermore, the definition of metachronous malignancy is not universally identical. The literature review shows that the American College of Surgeons defined multiple independent primaries as ‘two or more tumors arising at different sites or at the same site when histologic characteristics differ” (19). In our study, we defined metachronous malignancy as being of different histologic type in pulmonary and extra-pulmonary malignancy in the pathologic exam and this was similar to the definition of American College of Surgeons. Therefore, patients with squamous cell carcinoma of different origin (seven patients) were excluded from analysis because these was no reliable immuno-histo-chemical marker to differentiate where the metachronous malignancy come from (20). One patient presented as lung cancer first, but further tumor workup showed a hot spot lesion in the liver area. CT guide biopsy was arranged for the liver lesion and hepatocellular carcinoma was confirmed. He received left lower lobe lobectomy of the lung lesion first, and segmentectomy of the liver lesion later. Because the image study could not identify the actual sequence of tumor occurrence and he was categorized as having metachronous malignancy and included in our study.
In our study, there were no significant differences in the clinico-pathologic presentations between the lung cancer group and the metachronous malignancy group. Lung cancer patients presented as predominantly male (P=0.052), of older age (P=0.06), and with larger tumor size (P=0.06) but none were statistically significant. These presentations may be caused by different clinical scenarios that encountered by lung cancer and metachronous group. For the lung cancer group, most were identified incidentally by abnormal chest plain film and had characteristics similar to the clinical presentations of lung cancer, i.e., old age and predominantly male. For metachronous malignancy group, the related small mean tumor size may be on account of these patients all being under surveillance at regular intervals as part of previous malignancy follow up. Since the case numbers are relatively small, further investigation is warranted. From the data we were collected, both groups were presented similar clinico-pathologic characteristics. In addition, both lung cancer and metachronous malignant group were showed similar disease free and overall survival. This result suggests that locoregional metachronous malignancy may not impact survival in patients with resectable lung cancer. This finding may indicate that the extra-pulmonary metachronous malignancy is an individual, separated event, not related to lung cancer. Anatomic resection and regional LN dissection are recommended for secondary primary malignancy if the previous malignancy showed stable disease without relapse. The clinical significance of this finding was as follows. For patients presenting with previous extra-pulmonary malignancy, the relationship with past malignancy and the resectability of the lung lesion should be completely worked up. If previous malignancy showed stable disease and extra-pulmonary lesion was confirmed different cell origin and resectable disease anatomic resection with mediastinal LN dissection are recommended. For patients presenting with extra-pulmonary and pulmonary malignancies, anatomic resection with regional LN dissection are recommended if different tumor cell types are found, and both malignancies are shown to be resectable. For patients presenting with previous pulmonary malignancy, the relationship with previous pulmonary malignancy and the resectability of the extra-pulmonary lesion should be completely worked up. Anatomic resection with regional LN dissection is recommended if previous pulmonary malignancy showed no relapse and the extra-pulmonary lesion was resectable. For patients who had uncertain the relationship between the first and second malignancies, anatomic resection for locoregional malignancy may be considered as a treatment option. In the era of target therapy, more tissue may lead for possible further genetic survey and personalized treatment planning which beneficial to patient’s overall survival. Take lung cancer for example, patients who are confirmed to have a distant relapse related to previous lung cancer, further genetic survey is warranted and more personalized treatment plan could be made for disease control. We also further analyzed the survival impact of pathologic stage of lung cancer. Only in pathologic stage IIIA lung cancer does metachronous malignancy show worse overall survival than in lung cancer only. However, overall survival is the summation of adjuvant therapy and further investigation is warranted because of the limited number of cases.
There are still limitations to our study. First, this is a retrospective study. But we only analyzed for patients with underwent radical resection and corresponding adjuvant therapy for the pulmonary and extra-pulmonary malignancies and all patients underwent complete follow up longer than 5 years. In this study, we identified surgical intervention as recommended for patients with loco-regional invasion status of the metachronous malignancy. A second limitation was the relatively small case numbers after sub-grouping of patients into different stages. We identified no survival difference between the lung cancer group and the metachronous malignancy group from pathologic staging IA to IIB. Only in stage IIIA lung cancer patients who presented with metachronous malignancy was there worse overall survival, compared with those with lung cancer only. However, further investigation is warranted because of the small case numbers. Third, we included lung cancer patients who presented with a secondary extra-pulmonary malignancy, however, the case numbers were very limited, and current imaging tools could not identify the actual sequence of occurrence among the malignancies and we categorized as metachronous malignancy group. Further investigation may be warranted after new imaging modalities become available. A fourth limitation lay in our exclusion of patients who presented as squamous cell carcinoma both in the lung and other sites because of some lingering difficulties in distinguishing causality. We could not clarify the survival impact of metachronous squamous cell carcinoma on squamous cell lung cancer patients. Although these limitations remain, locoregional metachronous malignancy has no impact on survival of lung cancer patients who receive curative treatment.
Conclusions
In clinical practice, metachronous malignancy was also seen in lung cancer patients, and may be identified before or after the diagnosis of lung cancer. Locoregional metachronous malignancy has no impact on survival of lung cancer patients who receive curative treatment. Anatomic resection with regional LN dissection is recommended if different tumor cell types and resectable disease are confirmed.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chen SC, Teng CJ, Hu YW, et al. Secondary primary malignancy risk among patients with esophageal cancer in Taiwan: a nationwide population-based study. PLoS One 2015;10:e0116384. [Crossref] [PubMed]
- Lu CH, Lee KD, Chen PT, et al. Second primary malignancies following thyroid cancer: a population-based study in Taiwan. Eur J Endocrinol 2013;169:577-85. [Crossref] [PubMed]
- Cho YY, Lim J, Oh CM, et al. Elevated risks of subsequent primary malignancies in patients with thyroid cancer: a nationwide, population-based study in Korea. Cancer 2015;121:259-68. [Crossref] [PubMed]
- Atienza JA, Dasanu CA. Incidence of second primary malignancies in patients with treated head and neck cancer: a comprehensive review of literature. Curr Med Res Opin 2012;28:1899-909. [Crossref] [PubMed]
- Chen MC, Feng IJ, Lu CH, et al. The incidence and risk of second primary cancers in patients with nasopharyngeal carcinoma: a population-based study in Taiwan over a 25-year period (1979-2003). Ann Oncol 2008;19:1180-6. [Crossref] [PubMed]
- Chen CY, Lai CH, Lee KD, et al. Risk of second primary malignancies in women with cervical cancer: a population-based study in Taiwan over a 30-year period. Gynecol Oncol 2012;127:625-30. [Crossref] [PubMed]
- Lee KD, Chen SC, Chan CH, et al. Increased risk for second primary malignancies in women with breast cancer diagnosed at young age: a population-based study in Taiwan. Cancer Epidemiol Biomarkers Prev 2008;17:2647-55. [Crossref] [PubMed]
- Marees T, Moll AC, Imhof SM, et al. Risk of second malignancies in survivors of retinoblastoma: more than 40 years of follow-up. J Natl Cancer Inst 2008;100:1771-9. [Crossref] [PubMed]
- AIRTUM Working Group. Italian cancer figures, report 2013: Multiple tumours. Epidemiol Prev 2013;37:1-152. [PubMed]
- Tabuchi T, Ito Y, Ioka A, et al. Incidence of metachronous second primary cancers in Osaka, Japan: update of analyses using population-based cancer registry data. Cancer Sci 2012;103:1111-20. [Crossref] [PubMed]
- Brock MV, Alberg AJ, Hooker CM, et al. Risk of subsequent primary neoplasms developing in lung cancer patients with prior malignancies. J Thorac Cardiovasc Surg 2004;127:1119-25. [Crossref] [PubMed]
- Aziz TM, Saad RA, Glasser J, et al. The management of second primary lung cancers. A single centre experience in 15 years. Eur J Cardiothorac Surg 2002;21:527-33. [Crossref] [PubMed]
- Duchateau CS, Stokkel MP. Second primary tumors involving non-small cell lung cancer: prevalence and its influence on survival. Chest 2005;127:1152-8. [PubMed]
- Liu YY, Chen YM, Yen SH, et al. Multiple primary malignancies involving lung cancer-clinical characteristics and prognosis. Lung Cancer 2002;35:189-94. [Crossref] [PubMed]
- Fernandes G, Sucena M, Lombardia E, et al. Non small cell lung cancer - comparison between clinical and pathological staging. Rev Port Pneumol 2006;12:337-57. [Crossref] [PubMed]
- Vaz AP, Fernandes G, Souto Moura C, et al. Integrated PET/CT in non small cell lung cancer staging--clinical and pathological agreement. Rev Port Pneumol 2012;18:109-14. [Crossref] [PubMed]
- McCann J. PET scans approved for detecting metastatic non-small-cell lung cancer. J Natl Cancer Inst 1998;90:94-6. [Crossref] [PubMed]
- National Comprehensive Cancer Network Guideline Version1.2015. Available online: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp
- The Facility Oncology Registry Data Standards (FORDS). Chicago: Commission on Cancer, American College of Surgeons, 2002. Available online: https://www.facs.org/~/media/files/quality%20programs/cancer/coc/fords/fordsoriginal2003.ashx
- Carney JM, Kraynie AM, Roggli VL. Immunostaining in lung cancer for the clinician. Commonly used markers for differentiating primary and metastatic pulmonary tumors. Ann Am Thorac Soc 2015;12:429-35. [Crossref] [PubMed]