Is the incident of once chronic obstructive pulmonary disease related admission a high risk for readmission in the future?
Highlight box
Key findings
• An incident of one admission in the previous year was not a good predictor of future readmission.
What is known and what is new?
• GOLD and China’s COPD guidelines suggest that even if an incident of one admission previously also is an index of frequent exacerbators.
• However, we found an incident of one admission in the previous year was not a good predictor of future readmission, and ≥2 admissions in 1 year or ≥3 admissions within 5 years are good “labels” for the patients with frequent exacerbation admissions.
What is the implication, and what should change now?
• The incident of one admission previously as an index of high-risk AECOPD may not be applicable in China. Because there are significant differences in the admission criteria for AECOPD in China from Western countries. The severity of AECOPD admission in different hospitals in China is so different, and the risk of future exacerbations is also different.
Introduction
According to the epidemiological survey, about 100 million patients with chronic obstructive pulmonary disease (COPD) in China is the third most common chronic disease (1). In China, COPD ranked fourth as a leading cause of death in urban areas and third in rural areas (2). Acute exacerbation is a crucial worsening event of COPD, particularly those requiring admission that seriously affects their quality of life (3), accelerates the deterioration of lung function (4), imposes a heavy disease burden (5), and even leads to death (6). In China, the admission rate for COPD has continued to rise in the past decade (2). Prevention and reduction of acute exacerbation of COPD (AECOPD) are essential objectives of COPD management (7).
COPD has the highest admission rate in respiratory diseases in China and is also one of the most common reasons for readmission (8,9). Repeated readmissions overuse medical resources and lead to a substantial economic burden (8). Data from the ECLIPSE study (10) proposed that patients with a history of ≥2 exacerbations in a previous year represented the frequent exacerbation phenotype of COPD. Similar to ECLIPSE, the other studies also demonstrated that prior hospital admissions strongly predicted COPD-related readmission (11-13). Global Initiative for Chronic Obstructive Lung Disease (GOLD) (7) and China’s COPD guidelines (14) adopted the results from ECLIPSE for the assessment of exacerbation risk in the future. Furthermore, even if an incident of one hospital admission previously also is recommended by the guidelines to identify frequent exacerbators. Nevertheless, there is no rigorous scientific evidence for this proposal.
As we all know, there is a vast difference in the Medicaid Services System between the USA, European Union, and China. We do not have a universal standard of AECOPD admission in China, and the disease severity varies considerably. Therefore, it may not be reasonable to assess the readmission risk in the event of only one prior admission in China.
In this paper, we aim to better understand the events of the previous admissions due to AECOPD which would be a predictor of readmission. The patients with AECOPD admitted to our hospital in the past 5 years were analyzed to recognize the clinical characteristics of the patients with frequent AECOPD and the risk factors associated with frequent readmission due to AECOPD, achieving the development of readmission reduction strategies. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1504/rc).
Methods
Study population
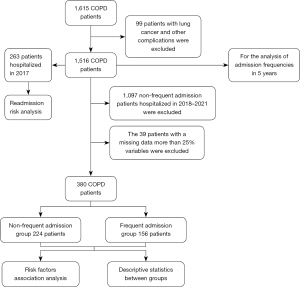
The data in this study were obtained from the inpatient database in the Third Affiliated Hospital of Chongqing Medical University from January 2017 to December 2021. A total of 1,615 subjects with a primary diagnosis of International Classification of Diseases-10 (ICD-10) coded as “chronic obstructive pulmonary disease with acute exacerbation” were recruited. Ninety-nine patients with lung cancer, pneumothorax, neumoconiosis, severe bronchiectasis, and pulmonary embolism were excluded.
Data collection
The general demography and clinical parameters were collected from recruited patients. The diagnosis of coronary heart disease, diabetes, and renal insufficiency in the enrolled subjects shall be based on the records of corresponding medical history. Whether or not to use home oxygen therapy, a home ventilator, inhaled corticosteroid (ICS), and long-acting β2-agonist (LABA) before admission were obtained from the medical records. The amount of smoking of current and former smokers was expressed in the pack years.
Analysis population
All individuals’ admissions were used to calculate the admission frequency. But, the individuals with missing data more than 25% variables were excluded from the analysis of the clinical characteristics.
We defined three or more admissions within 5 years as the frequent admissions group and the patients hospitalized only once in 2017 and less than three times all over the 5-year study period as the non-frequent admission group. The inpatients during 2018–2021 were not enrolled as non-frequent admission because they had not enough follow-up time for 5 years.
The 263 individuals with a different frequency of hospitalized exacerbations in 2017 were grouped to determine the risk of readmission in the following years. The flow chart of recruiting the study population and cohort is outlined in Figure 1.
Statistical analysis
In this study, we used descriptive statistics to report the characteristics of frequent and non-frequent admission groups. Normally distributed data are described by mean ± standard deviation (SD), and an independent sample t-test was applied to compare the variables between frequent and non-frequent admission groups. Non-normally distributed data are expressed as median and interquartile range, and the difference between the two groups was tested by Mann-Whitney U rank sum test. Count data are shown as n (%), and the chi-square test was used to compare groups. A two-sided P value of <0.05 indicates statistical significance. Multivariable stepwise logistic regression analysis was conducted to evaluate factors associated with frequent admissions.
The incidence of AECOPD-related admission in all over 5 study years and each calendar year of 2017–2021 were calculated and expressed as a per-person per-year rate. Univariable logistic regression analysis was used to analyze readmission risk based on the admission history in 2017.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Third Affiliated Hospital of Chongqing Medical University (No. 2022-089). Individual consent for this retrospective analysis was waived.
Results
The clinical characteristics of patients with frequent admissions
After excluding 10 and 29 patients with insufficient data from the groups of frequent and non-frequent exacerbation admissions, respectively. A total of 1,097 patients with admission less than 3 times in 2018–2021 were excluded because their follow-up time was less than 5 years. In total, 156 patients with frequent admission and 224 non-frequent admissions were included in the analysis of their clinical characteristics. The results are shown in Table 1. There were significant differences in the smoking, average admission days, admission expenses, pH, and arterial CO2 pressure (PaCO2) in blood gas and blood eosinophils counts, as well as in the proportion of patients with comorbidities (coronary heart disease, diabetes), respiratory tract infection with pseudomonas aeruginosa during admission, use of ICS/LABA, home oxygen therapy and home ventilator before admission (P<0.05–0.001). There was a marked tendency for more severe disease severity in the frequent admission group than in the non-frequent admission group.
Table 1
| Variables | All (n=380) | Frequent admission (n=156) | Non-frequent admission (n=224) | P value |
|---|---|---|---|---|
| Age (years) | 74.58±8.72 | 75.31±8.47 | 74.08±8.88 | 0.176 |
| Gender | 0.086 | |||
| Male | 303 (79.7) | 131 (84.0) | 172 (76.8) | |
| Female | 77 (20.3) | 25 (16.0) | 52 (23.2) | |
| Smoking (pack years) | 30 [0, 50] | 35 [15.75, 50] | 20 [0, 40] | 0.005 |
| Admission days | 8 [6, 10] | 8 [7, 10.25] | 7 [5, 9] | 0.001 |
| Admission expenses (yuan) | 8,053.6 [6,179.6, 11,397.5] | 9,557.2 [6,985.1, 14,117.6] | 7,120.4 [6,263.8, 9,353.2] | 0.001 |
| ICS/LABA | 173 (45.5) | 120 (76.9) | 53 (23.7) | 0.001 |
| Home oxygen therapy | 68 (17.9) | 55 (35.3) | 13 (5.8) | 0.001 |
| Home noninvasive ventilator | 11 (2.9) | 10 (6.4) | 1 (0.4) | 0.002 |
| Coronary heart disease | 71 (18.7) | 38 (24.4) | 33 (14.7) | 0.018 |
| Cor pulmonale | 115 (30.3) | 55 (35.3) | 60 (26.8) | 0.077 |
| Diabetes | 28 (7.4) | 19 (12.2) | 9 (4.0) | 0.003 |
| Abnormal renal function | 22 (5.8) | 8 (5.1) | 14 (6.3) | 0.638 |
| pH | 7.42 [7.38, 7.45] | 7.41 [7.37, 7.44] | 7.43 [7.39, 7.46] | 0.002 |
| PaO2 (mmHg) | 74.5 [61, 92] | 73. 5 [58, 93.5] | 70 [61, 91] | 0.526 |
| PaCO2 (mmHg) | 46 [40, 57] | 48 [41, 59] | 42 [38, 57] | 0.003 |
| D-dimer (ng/mL) | 198 [113, 373] | 238 [117, 436.75] | 180 [102, 323] | 0.115 |
| WBC (×109/L) | 8.25 [6.20, 10.42] | 8.28 [6.66, 10.81] | 8.66 [6.49, 10.98] | 0.157 |
| NEU (×109/L) | 6.33 [4.44, 8.41] | 6.36 [4.76, 8.80] | 6.74 [4.65, 9.45] | 0.095 |
| EOS (×109/L) | 0.05 [0.01, 0.16] | 0.07 [0.02, 0.17] | 0.04 [0.01, 0.10] | 0.006 |
| EOS (%) | 0.7 [0.1, 2.1] | 1.2 [0.2, 2.4] | 0.4 [0.1, 1.5] | 0.003 |
| CRP (mg/L) | 19.77 [5.31, 60.78] | 21.09 [6.33, 66.19] | 28.29 [5.33, 78.43] | 0.169 |
| PCT (ng/mL) | 0.08 [0.04, 0.20] | 0.08 [0.04, 0.20] | 0.08 [0.05, 0.26] | 0.959 |
| Sputum culture aeruginosa (+) | 21 (5.8) | 15 (10.6) | 6 (2.8) | 0.002 |
| Mechanical ventilation | 34 (8.9) | 29 (18.8) | 5 (2.2) | 0.001 |
| Days of inhaled hormone use (days) | 6 [4.25, 9] | 7 [5, 10] | 5 [5, 7] | 0.001 |
| Days of using antibacterial drugs (days) | 6 [3, 8] | 7 [5, 9] | 5 [0, 7] | 0.001 |
Distribution: for normally distributed data, described by mean ± SD, for categorical variables, the absolute count n (%) or median [25th–75th percentiles] of the distribution is reported. ICS/LABA, inhaled corticosteroid/long-acting β2-agonist; PaO2, arterial O2 pressure; PaCO2, arterial CO2 pressure; WBC, white blood cell; NEU, blood neutrophil; EOS, blood eosinophil; CRP, C-reactive protein; PCT, procalcitonin; SD, standard deviation.
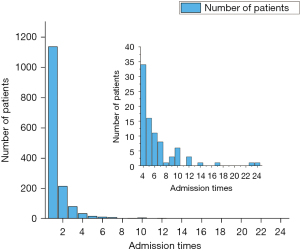
The frequency of admissions in 2017–2021 (Figure 2)
In this 5 years longitudinal study, we enrolled 1,516 individuals with 2,351 admissions to analyze the admission frequency. Among them, 89.1% were non-frequent inpatients, and only 10.9% were frequent exacerbation admission. However, the individuals with frequent admissions had a total of 787 admissions over the 5 years, accounting for 33.5% of admissions. The admission frequency was 4.1 times that of the patients with non-frequent admission (0.95 vs. 0.23 per person per year).
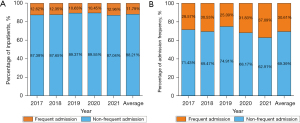
The annual frequency of admission
In each natural year within 5 years, most patients (88.2%) experienced admission only once, and 11.8% had two or more admissions (Figure 3A). Nevertheless, their average number of admission in each natural year was 3.3 times that of those who only had one admission in each year (Figure 3B).
The readmission rate based on different admission frequencies in the previous year
Among the 263 individuals who recorded one admission in 2017, only 39 (14.8%) remained COPD-related readmissions in the next year, and 70 experienced readmissions in the following 4 years (positive predictive value, 26.6%). While, of 42 individuals who had at least two admissions in 2017, 23 individuals in the next and 27 in the following 4 years experienced readmission (positive predictive value, 54.8%, and 64.3%, respectively). Moreover, the accumulated readmission rates of those who occurred 2 or >2 admissions in 2017 were 87.3% and 78.9%, respectively during the 4 years following-up (Figure 4). The readmission frequency in patients with at least two admissions in 2017 was significantly higher than that of those who had only one admission in 2017 (P<0.001).
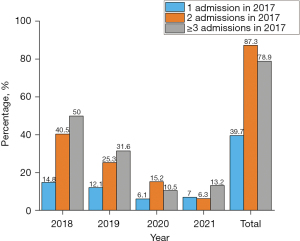
Over the 4 years following 2017, the readmission rate of patients who had admission in 2017 was the highest in the next year [2018], then decreased gradually (Figure 4).
The risk of readmission by the history of admission events
The history of more admissions was very strongly predictive of AECOPD-related readmissions. The individuals with 2 and ≥3 times admissions in the previous year had respectively 4.1- and 7.5-fold higher risk of readmission [crude odds ratio (OR): 4.10, 95% confidence interval (CI): 1.24–13.58, P<0.05 and crude OR: 7.51, 95% CI: 3.81–16.68, P<0.001] than those with only one admission in the previous year (Table 2). In addition, the risk of readmission of individuals with two or more admissions did not further increase in the following 4 years (Table 2).
Table 2
| Factors | Number of admissions | ||||
|---|---|---|---|---|---|
| Adm. 1 vs. Adm. 2 | Adm. 1 vs. Adm. ≥3 | ||||
| OR (95% CI) | P value | OR (95% CI) | P value | ||
| Readmission risk in next year | 4.10 (1.24–13.58) | 0.021 | 7.51 (3.81–16.68) | <0.001 | |
| Readmission risk in next 4 years | 3.86 (1.186–12.56) | 0.025 | 5.51 (2.45–12.36) | <0.001 | |
Adm. 1, one admission; Adm. 2, two admissions; Adm. ≥3, admission ≥3 times; OR, odds ratio; CI, confidence interval.
Risk factors associated with frequent admission due to AECOPD
Factors associated with frequent readmissions based on a univariate and multivariate regression analysis are shown in Tables 3,4. The independent risk factors associated with frequent readmissions were smoking index, diabetes, mechanical ventilation, pseudomonas aeruginosa infection, and days of use of antibiotics in the previous hospitalization.
Table 3
| Variable | Regression coefficients | Standard errors | Wald | P | OR | 95% CI | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Smoking index | 0.011 | 0.004 | 8.159 | 0.004 | 1.011 | 1.004 | 1.019 |
| pH | −6.444 | 2.083 | 9.574 | 0.002 | 0.002 | 0.000 | 0.094 |
| PaCO2 | 0.021 | 0.007 | 7.754 | 0.005 | 1.021 | 1.006 | 1.036 |
| Coronary heart disease | 0.623 | 0.265 | 5.513 | 0.019 | 1.864 | 1.108 | 3.134 |
| Diabetes | 1.198 | 0.419 | 8.167 | 0.004 | 3.313 | 1.457 | 7.534 |
| Days of use antibiotics in hospitalization | 0.086 | 0.027 | 9.865 | 0.002 | 1.090 | 1.033 | 1.150 |
| Pseudomonas aeruginosa infection | 1.424 | 0.496 | 8.244 | 0.004 | 4.154 | 1.571 | 10.979 |
| Mechanical ventilation | 2.314 | 0.497 | 21.673 | 0.000 | 10.115 | 3.818 | 26.796 |
OR, odds ratio; CI, confidence interval; PaCO2, arterial CO2 pressure.
Table 4
| Variables | Regression coefficients | Standard errors | Wald | P | Crude OR | 95% CI | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Smoking | 0.012 | 0.005 | 5.382 | 0.020 | 1.012 | 1.002 | 1.022 |
| Diabetes | 1.865 | 0.680 | 7.514 | 0.006 | 6.457 | 1.702 | 24.500 |
| Days of use antibiotics in hospitalization | 0.111 | 0.049 | 5.033 | 0.025 | 1.117 | 1.014 | 1.230 |
| Mechanical ventilation | 1.824 | 0.736 | 6.138 | 0.013 | 6.195 | 1.464 | 26.218 |
| Pseudomonas aeruginosa infection | 1.437 | 0.692 | 4.315 | 0.038 | 4.207 | 1.085 | 16.320 |
OR, odds ratio; CI, confidence interval.
Discussion
A COPD phenotype for frequently hospitalized exacerbation has been identified from our data in 5 years. Our study defined the phenotype as three or more admissions during the 5-year study period. Though only a few individuals (10.9%) had frequent admissions, their average number of admissions was 4.1 times that of the non-frequent admission individuals, suggesting those were prone to experience exacerbation.
However, it is not very practical to identify for identifying the frequent exacerbators by a 5-year history of admissions. Therefore, we also analyzed the frequency of admission in each calendar year during the 5-year study period. We found that the vast majority of individuals occurred only one admission each year, and only a tiny percentage of individuals (11.8%) occurred two or more admissions with much higher average admissions per year (3.33 per person per year).
In the ECLIPSE study, a frequent exacerbation (≥2 events) phenotype tended to remain relatively stable for all 3 years of the study (8). So, a history of frequent exacerbation may be a strong predictor for subsequent exacerbation. Therefore, the COPD guidelines recommend a history of ≥2 exacerbations as an index of the high risk of exacerbation in the future. The guideline also proposed a label of exacerbation risk even if there was only one admission in the previous year.
Unexpectedly, we found that the positive predictive value for readmission risk by one admission history was inferior, only 14.8%. This is inconsistent with the recommendation by the COPD guidelines. We consider that the ambiguity arises from neither the scientific standard of AECOPD nor the severity grading (15). Instead, symptom-based and event-based definitions are proposed to define AECOPD and its severity grading (7,10). As there is no strict standard for AECOPD admission in China, there may be a significant difference in the severity of patients admitted to the hospital. The data from a national, multicenter registry study for AECOPD in China showed that the average arterial O2 pressure (PaO2) and PaCO2 of the recruited inpatients were 69.5 mmHg and 42.0 mmHg (16), which suggests that the majority of patients with AECOPD hospitalized were not severe exacerbators. We could not provide exact data about severity grading in our study. Still, more than half of admitted patients were not severe by rough statistics based on diagnosis without respiratory failure. So, the hospitalized exacerbation in our study represented mainly moderate/severe severity.
There is a considerable limitation that one admission event together with a history of two exacerbations is proposed as an index of high risk for future exacerbation because it has not enough evidence. In SHERLOCK (17) and ECLIPSE (10) studies, the subsequent exacerbations were significantly higher in individuals who experienced two or more exacerbations than those who had only one.
Furthermore, the 3-year prospective data from SPIROMICS cohort (18) indicated that the exacerbation status of most individuals varies markedly from year to year, and only a few (<10% of all patients) had a persistent exacerbation during the 3 study years (18).
In this study, the readmission rate of the patients with one and ≥2 admissions in the previous year was respectively 14.8% and 54.8%, which are very similar to that of the infrequent and frequent exacerbators in the ECLIPSE study (16.8% and 60.0%, respectively) (10). Therefore, we suppose that the two categories of different readmission rates in the prior year represent the subtypes of infrequent and frequent hospitalized exacerbation. So, only an incident of admission is not a good predictor for future readmission due to AECOPD.
In addition to the patient’s history of acute exacerbation or admission, many other factors, such as age, severity, complicated heart disease, diabetes, gastroesophageal reflux, oral corticosteroid use, and blood eosinophilia are associated with the risk of repeated exacerbation too (19-22). We also found that smoking, comorbidity with diabetes, mechanical ventilation, and infection with pseudomonas aeruginosa were associated with readmission. Specially, infection with pseudomonas aeruginosa as an independent risk factor was our important finding. The risk factors differ in different studies, suggesting that the influencing factors are diversified and individualized. It is perhaps more reasonable and accurate to assess the exacerbation risk in the future with multiple parameters, including a history of exacerbation and other confirmed risk factors.
Limitations
As a retrospective study, we had no data on the patients experiencing exacerbations or going to other clinics or hospitals for treatment after discharge from our hospital. So, it may underestimate the readmission rate, especially non-serious exacerbation. However, the readmission rate for those with only one admission is too low, so a few missing data would not change the conclusion.
Conclusions
There is a subtype of frequent admission due to AECOPD, which can be identified by the frequent admissions three or more times in 5 consecutive years or two or more in a year. The disease severity of inpatients in our study was moderate/severe AECOPD. The strong predictor for COPD-related readmission was two or more admissions in the prior year. Nevertheless, an incident of one admission in the previous year was not a good predictor of future readmission.
Acknowledgments
Funding: The study was supported by Key Projects in the Field of Special Setting Development for Technological Innovation and Application in Chongqing City (No. 2022TIAD-KPX0226).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1504/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1504/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1504/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1504/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Third Affiliated Hospital of Chongqing Medical University (No. 2022-089). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health CPH study): a national cross-sectional study. Lancet 2018;391:1706-17. [Crossref] [PubMed]
- Fang X, Wang X, Bai C. COPD in China: the burden and importance of proper management. Chest 2011;139:920-9. [Crossref] [PubMed]
- Seemungal TA, Donaldson GC, Paul EA, et al. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998;157:1418-22. [Crossref] [PubMed]
- Donaldson GC, Seemungal TA, Bhowmik A, et al. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 2002;57:847-52. [Crossref] [PubMed]
- Guarascio AJ, Ray SM, Finch CK, et al. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res 2013;5:235-45. [PubMed]
- Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, et al. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 2005;60:925-31. [Crossref] [PubMed]
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease. Available online: https://goldcopd.org/wp-content/uploads/2021/12/GOLD-REPORT-2022-v1.1-22Nov2021_WMV.pdf
- Jacobs DM, Noyes K, Zhao J, et al. Early Hospital Readmissions after an Acute Exacerbation of Chronic Obstructive Pulmonary Disease in the Nationwide Readmissions Database. Ann Am Thorac Soc 2018;15:837-45. [Crossref] [PubMed]
- Baker CL, Zou KH, Su J. Risk assessment of readmissions following an initial COPD-related hospitalization. Int J Chron Obstruct Pulmon Dis 2013;8:551-9. [PubMed]
- Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010;363:1128-38. [Crossref] [PubMed]
- Roberts MH, Clerisme-Beaty E, Kozma CM, et al. A retrospective analysis to identify predictors of COPD-related rehospitalization. BMC Pulm Med 2016;16:68. [Crossref] [PubMed]
- Garcia-Aymerich J, Farrero E, Félez MA, et al. Risk factors of readmission to hospital for a COPD exacerbation: a prospective study. Thorax 2003;58:100-5. [Crossref] [PubMed]
- Chen L, Chen S. Prediction of readmission in patients with acute exacerbation of chronic obstructive pulmonary disease within one year after treatment and discharge. BMC Pulm Med 2021;21:320. [Crossref] [PubMed]
- Chronic Obstructive Pulmonary Disease Group of Chinese Thoracic Society. Guidelines for the diagnosis and management of chronic obstructive pulmonary disease (revised version 2021). Zhonghua Jie He He Hu Xi Za Zhi 2021;44:170-205. [PubMed]
- Burge S, Wedzicha JA. COPD exacerbations: definitions and classifications. Eur Respir J Suppl 2003;41:46s-53s. [Crossref] [PubMed]
- Liang C, Mao X, Niu H, et al. Characteristics, Management and In-Hospital Clinical Outcomes Among Inpatients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease in China: Results from the Phase I Data of ACURE Study. Int J Chron Obstruct Pulmon Dis 2021;16:451-65. [Crossref] [PubMed]
- Haughney J, Lee AJ, Nath M, et al. The long-term clinical impact of COPD exacerbations: a 3-year observational study (SHERLOCK). Ther Adv Respir Dis 2022;16:17534666211070139. [Crossref] [PubMed]
- Han MK, Quibrera PM, Carretta EE, et al. Frequency of exacerbations in patients with chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohort. Lancet Respir Med 2017;5:619-26. [Crossref] [PubMed]
- Müllerova H, Maselli DJ, Locantore N, et al. Hospitalized exacerbations of COPD: risk factors and outcomes in the ECLIPSE cohort. Chest 2015;147:999-1007. [Crossref] [PubMed]
- Bernabeu-Mora R, García-Guillamón G, Valera-Novella E, et al. Frailty is a predictive factor of readmission within 90 days of hospitalization for acute exacerbations of chronic obstructive pulmonary disease: a longitudinal study. Ther Adv Respir Dis 2017;11:383-92. [Crossref] [PubMed]
- Bahadori K, FitzGerald JM. Risk factors of hospitalization and readmission of patients with COPD exacerbation--systematic review. Int J Chron Obstruct Pulmon Dis 2007;2:241-51. [PubMed]
- Faner R, Tal-Singer R, Riley JH, et al. Lessons from ECLIPSE: a review of COPD biomarkers. Thorax 2014;69:666-72. [Crossref] [PubMed]