
Risk factors of aspiration occurrence with different feeding patterns in elderly intensive care unit patients: a cross-sectional study
Highlight box
Key findings
• The characteristics of aspiration occurrence in elderly ICU patients with different feeding patterns are significantly different. We should take early and individualized preventive measures according to the patient’s characteristics and eating patterns and should supplement them with targeted nursing interventions to reduce the possibility of aspiration, thus improving the patient's prognosis and enhancing the quality of life.
What is known and what is new?
• Different feeding practices can affect the incidence of overt and silent aspiration.
• Different clinical features have a significant impact on overt versus silent aspiration.
What is the implication, and what should change now?
• In the feeding of elderly patients in the ICU, targeted nursing interventions should be adopted according to the different clinical characteristics of the patients. High priority should be given to high-risk groups and regular checkups to identify the possibility of absorption early, thus improving the quality of patient survival.
Introduction
Aspiration is the process of foreign bodies entering the respiratory tract via the glottis during feeding or non-feeding, and these foreign bodies include secretions, blood, bacteria, food, stomach contents, and so on (1). Aspiration often leads to morbidity and mortality through the direct effects of particulate matter, acid-related injuries, and aspiration pneumonia (2). According to the symptoms, it can be divided into overt aspiration and silent aspiration (3). Overt aspiration refers to the symptoms of irritating choking cough, shortness of breath, cyanosis, and asphyxia immediately after aspiration, whereas silent aspiration refers to an absence of any symptoms or symptoms including only mental depression, apathy, and unresponsiveness; it can lead to chronic cough, chronic bronchitis, interstitial fibrosis, and other diseases in the long term. The incidence of overt aspiration is 8.80–22.45% (4), and the incidence of silent aspiration is as high as 88.00% in intensive care unit (ICU) patients (5). Due to degenerative physiological changes and diseases, the rate of aspiration in elderly people is as high as 57.9%, which is a high-risk group for aspiration. Aspiration can seriously endanger the health of the elderly, and it is the main causative factor of lung infections in the elderly, which can lead to respiratory failure and even death in serious cases.
On account of the severity and specificity of their conditions, elderly patients in the ICU mainly receive nutrition through oral feeding and tube feeding (6). Some international guidelines that suggest early enteral nutrition as the standard treatment for critically ill patients (7,8). However, the resulting gastric contents reflux is one of the main reasons for aspiration risk in critically ill patients. It has a high incidence of occult aspiration, but because the occurrence of silent aspiration is not perceptible, it is often ignored by clinical staff. Since gastric contents contain gastric acid and pepsin, aspiration can induce a serious inflammatory response and directly damage the airway and alveolar-capillary membrane, which leads to protein-rich intravascular fluid leakage into the alveoli and degrades alveolar surface-active substances, eventually leading to alveolar atrophy and pulmonary atelectasis (9). In addition, gastric contents entering the airway contain large amounts of food residue, and tiny particles can cause extensive small airway obstruction, which can lead to aspiration pneumonia (10). Aspiration pneumonia accounts for approximately 80% of hospitalized elderly patients with pneumonia (11). Previous studies have found that the 5-year mortality rate of patients with respiratory failure due to aspiration pneumonia was 18.7%, which is higher than that of other types of pneumonia (12,13). It is expected to make an increasing contribution to mortality and morbidity among the elderly population in the coming decades (14). Therefore, it is important to understand the characteristics and influencing factors of the occurrence of aspiration in elderly patients with different feeding patterns, in order to enable the implementation of targeted aspiration prevention.
In recent years, several studies in China and internationally (15-19) have shown that the occurrence of aspiration is influenced by a combination of risk factors, which can be categorized as patient-specific factors and treatment-related factors, among which patient-specific factors include age, intra-abdominal hypertension (IAH), gastric retention, swallowing disorder, nausea and vomiting, primary disease, and related symptoms; treatment-related factors include mechanical ventilation, enteral nutrition route, and so on. However, the magnitude of the independent and synergistic risk for aspiration especially for the patients in ICU is not clear and the degree of association with overt aspiration and silent aspiration is less explored. Although many studies (20,21) have been conducted by Chinese and international researchers on the occurrence, assessment, and prevention of aspiration, its incidence remains high. The occurrence of aspiration pneumonia will incur a significantly longer hospital stay, affect the rehabilitation outcome, increase the mental and economic burden, and have a great impact on the long-term prognosis and quality of life of patients. In addition, some studies (22,23) have reported that overt aspiration accounts for only 10% of aspiration pneumonia, whereas silent aspiration accounts for more than 70%. This suggests that compared with overt aspiration, silent aspiration is not only insidious and difficult to diagnose, but also may be more closely associated with poor prognosis of patients. Based on previous findings and our clinical experience, we speculate that age, dysphagia, aspiration history, and gastrointestinal tumors may be risk factors for aspiration in ICU patients. However, it is not clear whether there are significant differences in the characteristics and influencing factors of overt and silent aspiration in ICU elderly patients with different feeding patterns (22). Therefore, we need investigate the incidence of overt and invisible aspiration in ICU patients and to further clarify their interrelationships as well as the degree of influence on aspiration, so as to identify the risk factors early, implement targeted preventive measures to reduce aspiration complications, and improve the prognosis of patients. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-430/rc).
Methods
Research participants
A total of 348 elderly patients treated in the ICU ward of Hai’an People’s Hospital from April 2019 to April 2022 were included in this study.
The inclusion criteria were as follows: (I) patients were ≥65 years of age, regardless of gender; (II) feeding by mouth or tube feeding enteral nutrition; (III) length of hospitalization ≥1 week.
The exclusion criteria were as follows: (I) aspiration or aspiration pneumonia had occurred at the time of ICU admission; (II) previous diagnosis of gastroesophageal reflux (Figure 1).
The patients were divided into the oral feeding group, gastric tube feeding group, and post-pyloric feeding group according to their feeding method. Finally, according to the inclusion and exclusion criteria, 348 elderly patients treated in the ICU ward were included in this study.
In this study, the incidence of overt aspiration was used as the main outcome index. According to the previous study of the research group, the incidence of overt aspiration in ICU patients was about 20%. The general rule of logistic regression requires a ratio of item number to sample size of 1:5–1:10 and our research factors are about 10. Therefore, the sample size of the study population planned for this study was 380 cases. A total of 12 cases were lost during the research process and 20 cases were excluded. The final count was 348 cases.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Hai’an People’s Hospital (No. KYLC2022036). Informed consent was provided by all patients.
General information questionnaire
The general information questionnaire included demographic data (such as gender, age, body mass index (BMI), history of smoking, history of alcohol consumption) and clinical data (such as whether they were taking gastrointestinal motility drugs, whether they were chronically bedridden for ≥1 month, and hypertension status).
Investigation of aspiration and its risk factors
Clinical characteristics of the occurrence of overt versus silent aspiration included age, occurrence of impaired consciousness, occurrence of dysphagia, history of aspiration, presence of gastric retention, presence of IAH, occurrence of vomiting, ability to cough spontaneously, presence of gastrointestinal tumors, and whether mechanical ventilation was required.
The criteria of overt aspiration
As for the patients who eat orally, the patient had no choking cough or cough before eating, and any of the following symptoms during or after eating were judged as overt aspiration: (I) irritating cough; (II) abnormal pronunciation; (III) cyanosis, dyspnea, asthma, and sudden drop in oxygen saturation.
As for the patients with enteral nutrition, no choking cough or cough before nasal feeding, any of the following conditions during or after nasal feeding can be judged as dominant aspiration: (I) vomiting and sudden drop in blood oxygen saturation; (II) shortness of breath, dyspnea, obvious wet rales in the lungs, sputum sound in the throat, man-machine confrontation; (III) gastric contents were aspirated from the airway or found in sputum culture; (IV) there were no clinical symptoms of inhalation, but it was diagnosed as aspiration pneumonia (24,25).
The criteria of silent aspiration
In this study, the content of pepsin in airway secretions was determined by enzyme-linked immunosorbent assay (ELISA) as a basis for determining occult aspiration (26). Secretion specimens were collected respectively from 12 to 72 hours after fasting and feeding states of patients. For patients without an artificial airway, if the content of pepsin in 2 saliva specimens was >3.6 ng/mL, the patient was considered to have an occult aspiration (27), whereas for patients with an artificial airway, if the content of pepsin in 2 airway secretion specimens was >25.0 ng/mL, the patient was considered to have an occult aspiration (28).
Statistical analysis
The software SPSS 26.0 (IBM Corp., Armonk, NY, USA) was used for statistical processing. Normality test was conducted on continuous variables, and the level of α=0.10 was considered that the population obeyed normal distribution. The skewness continuous variable data is converted from skewness data to normal data for further analysis and calculation. The measurement data were expressed as mean ± standard deviation (SD) with independent samples t-test; the count data were expressed as number of cases and percentage with chi-square test, and the two-group chi-square test was used for two-group comparison. Multiple logistic regression analysis was performed on the independent variables. A two-sided P value <0.05 was considered a statistically significant difference.
Results
Baseline data
The baseline characteristics of the patients are shown in Table 1. A total of 348 elderly patients in the ICU were included in this study, with a mean age of 68.8±3.2 years in the non-aspiration group, including 56 male patients and 43 female patients; and a mean age of 70.2±3.4 years in the aspiration group, including 132 male patients and 117 female patients. A total of 50 patients in the non-aspiration group took gastrointestinal motility drugs and 49 patients did not take them; in the aspiration group, a total of 82 patients took gastrointestinal motility drugs and 167 patients did not take them. A total of 37 patients in the non-aspiration group had a history of prolonged bed rest and 62 patients did not; a total of 128 patients in the aspiration group had a history of prolonged bed rest and 121 patients did not. There were significant differences (P<0.05) between the aspiration group and the non-aspiration group in terms of age, taking gastrointestinal motility drugs or not, and prolonged bed rest history or not (Table 1).
Table 1
| Projects | Non-aspiration group | Aspiration group | χ2/Z/t value | P value |
|---|---|---|---|---|
| Age (years) | 68.8±3.2 | 70.2±3.4 | 3.422 | 0.001 |
| Gender | 0.360 | 0.548 | ||
| Male | 56 [57] | 132 [53] | ||
| Female | 43 [43] | 117 [47] | ||
| BMI (kg/m2) | 21.07±3.39 | 20.72±2.82 | 0.971 | 0.332 |
| Smoking history | 1.370 | 0.242 | ||
| Yes | 51 [52] | 111 [45] | ||
| No | 48 [48] | 138 [55] | ||
| Drinking history | 0.588 | 0.443 | ||
| Yes | 44 [44] | 122 [49] | ||
| No | 55 [56] | 127 [51] | ||
| Hypertension or not | 0.323 | 0.570 | ||
| Yes | 42 [42] | 114 [46] | ||
| No | 57 [58] | 135 [54] | ||
| Taking gastrointestinal motility drugs | 9.292 | 0.002 | ||
| Yes | 50 [51] | 82 [33] | ||
| No | 49 [49] | 167 [67] | ||
| Long-term bed rest time | 5.594 | 0.018 | ||
| Yes | 37 [37] | 128 [51] | ||
| No | 62 [63] | 121 [49] | ||
Data are presented as mean ± SD or n [%]. BMI, body mass index; SD, standard deviation.
Status analysis of aspiration in ICU elderly patients with different feeding patterns
Among 348 elderly patients in ICU, aspiration occurred in 249, and the incidence of aspiration was 72%. Among them, there were 78 people of overt aspiration with an incidence of 22% and 171 cases of silent aspiration with an incidence of 49%. The differences in the incidence of overt and silent aspiration between the oral feeding group, the gastric tube feeding group, and the post-pyloric feeding group were statistically significant (P<0.05) (Table 2; Figure 2).
Table 2
| Group | Number of cases | Overt aspiration, n [%] | Silent aspiration, n [%] | |||
|---|---|---|---|---|---|---|
| Occurrence | Did not occur | Occurrence | Did not occur | |||
| Oral feeding group | 103 | 16 [16] | 87 [84] | 54 [52] | 49 [48] | |
| Gastric tube feeding group | 128 | 38 [30] | 90 [70] | 70 [55] | 58 [45] | |
| Post-pyloric feeding group | 117 | 24 [21] | 93 [79] | 47 [40] | 70 [60] | |
| Total | 348 | 78 [22] | 270 [78] | 171 [49] | 177 [51] | |
| χ2 value | 6.941 | 5.787 | ||||
| P value | 0.031 | 0.055 | ||||
Comparison of overt aspiration characteristics in ICU elderly patients with different feeding patterns
Among patients with overt aspiration, the differences among the 3 groups were statistically significant (P<0.05) in terms of swallowing disorder, gastric retention, IAH, spontaneous cough, and mechanical ventilation (Table 3), whereas the results of the two-way comparison showed that patients in the gastric tube feeding group had significantly higher proportions in terms of swallowing disorder and gastric retention than those in the oral feeding group and the post-pyloric feeding group. Patients in the post-pyloric feeding group had statistically significantly higher rates of intra-abdominal hypertension, spontaneous cough and presence of mechanical ventilation than those in the oral feeding and gastric tube feeding groups (P<0.05) (Table 4).
Table 3
| Variables | Oral feeding group | Gastric tube feeding group | Post-pyloric feeding group | Test statistic | P value |
|---|---|---|---|---|---|
| Age (years) | 69.19±4.02 | 70.74±4.21 | 71.17±2.84 | 1.390 | 0.255 |
| Disorders of consciousness | 5 [31] | 23 [61] | 13 [54] | 3.906 | 0.142 |
| Swallowing disorder | 5 [31] | 24 [63] | 8 [33] | 7.362 | 0.025 |
| History of aspiration | 9 [56] | 13 [34] | 11 [46] | 2.417 | 0.299 |
| Gastric retention | 4 [25] | 21 [55] | 5 [21] | 8.908 | 0.012 |
| Intra-abdominal hypertension | 4 [25] | 14 [37] | 15 [63] | 6.438 | 0.040 |
| Vomiting | 5 [31] | 13 [34] | 6 [25] | 0.588 | 0.745 |
| Spontaneous cough | 3 [19] | 12 [32] | 15 [63] | 9.246 | 0.010 |
| Gastrointestinal tumors | 6 [38] | 15 [39] | 12 [50] | 0.858 | 0.651 |
| Mechanical ventilation | 4 [25] | 15 [39] | 16 [67] | 7.610 | 0.022 |
| Intra-abdominal hypertension | 4 [25] | 14 [37] | 15 [63] | 6.438 | 0.040 |
| Vomiting | 5 [31] | 13 [34] | 6 [25] | 0.588 | 0.745 |
Data are presented as mean ± SD or n [%]. SD, standard deviation.
Table 4
| Group | Swallowing disorders | Gastric retention | Intra-abdominal hypertension | Spontaneous cough | Mechanical ventilation |
|---|---|---|---|---|---|
| Oral feeding group with gastric feeding group comparison | 0.032 | 0.042 | 0.399 | 0.337 | 0.309 |
| Oral feeding group with post-pyloric feeding groups comparison | 0.890 | 0.757 | 0.020 | 0.006 | 0.010 |
| Gastric feeding group with oral feeding group comparison | 0.022 | 0.007 | 0.049 | 0.017 | 0.037 |
Comparison of silent aspiration characteristics in ICU elderly patients with different feeding patterns
Among patients with silent aspiration, the differences among the 3 groups were statistically significant (P<0.05) in terms of impaired consciousness, swallowing disorder, vomiting, and mechanical ventilation (Table 5). The results of the two-way comparisons showed that the proportion of patients with impaired consciousness in the oral feeding group was lower than that in the post-pyloric feeding group, and the proportions of patients with vomiting and swallowing disorder were lower than that in the gastric tube feeding group. The proportion of patients with spontaneous cough was higher in the post-pyloric feeding group than in the oral feeding group, whereas in terms of mechanical ventilation, the proportion of patients was higher than that in the gastric tube feeding group, with statistically significant differences (all P<0.05) (Table 6).
Table 5
| Group | Oral feeding group | Gastric tube feeding group | Post-pyloric feeding group | Test statistic | P value |
|---|---|---|---|---|---|
| Age (years) | 70.19±2.95 | 69.93±3.67 | 69.96±2.80 | 0.108 | 0.898 |
| Disordered consciousness | 14 [26] | 30 [43] | 24 [51] | 7.102 | 0.029 |
| Swallowing disorder | 9 [17] | 26 [37] | 14 [30] | 6.292 | 0.043 |
| History of aspiration | 18 [33] | 24 [34] | 18 [38] | 0.305 | 0.858 |
| Gastric retention | 9 [17] | 16 [23] | 10 [21] | 0.744 | 0.689 |
| Intra-abdominal hypertension | 22 [41] | 28 [40] | 24 [51] | 1.609 | 0.447 |
| Vomiting | 12 [22] | 32 [46] | 18 [38] | 7.396 | 0.025 |
| Spontaneous cough | 16 [30] | 32 [46] | 26 [56] | 7.043 | 0.03 |
| Gastrointestinal tumors | 21 [39] | 36 [51] | 21 [45] | 1.955 | 0.376 |
| Mechanical ventilation | 20 [37] | 22 [31] | 26 [55] | 6.946 | 0.031 |
Data are presented as mean ± SD or n [%]. SD, standard deviation.
Table 6
| Group | Disorders of consciousness | Swallowing disorders | Vomiting | Spontaneous cough | Mechanical ventilation |
|---|---|---|---|---|---|
| Oral feeding group with gastric feeding group comparison | 0.051 | 0.012 | 0.007 | 0.068 | 0.513 |
| Oral feeding group with post-pyloric feeding groups comparison | 0.009 | 0.117 | 0.078 | 0.009 | 0.066 |
| Gastric feeding group with oral feeding group comparison | 0.383 | 0.411 | 0.427 | 0.308 | 0.010 |
Independent risk factors for overt aspiration in ICU elderly patients
We performed a multiple logistic regression analysis of the 10 independent factors in the single-factor analysis and found that in the oral feeding group, swallowing disorders, history of aspiration, and gastrointestinal tumors had an effect on the occurrence of overt aspiration and were risk factors for it (Table 7; Figure 3A,3B), whereas in the gastric tube feeding group, we found that impaired consciousness, swallowing disorders, history of aspiration, and gastric retention significantly affected the incidence of overt aspiration (Table 8; Figure 3C,3D). In the post-pyloric feeding group, age, mechanical ventilation, IAH, and spontaneous cough were independent risk factors for the occurrence of overt aspiration (Table 9; Figure 3E,3F).
Table 7
| Group | Related factors | B | SE | Wald | P value | OR | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Overt aspiration | Age | 0.047 | 0.128 | 0.135 | 0.713 | 1.048 | 0.815 | 1.348 |
| Mechanical ventilation | −0.646 | 1.006 | 0.412 | 0.512 | 0.524 | 0.073 | 3.765 | |
| Disorders of consciousness | 0.691 | 0.852 | 0.657 | 0.418 | 1.996 | 0.376 | 10.606 | |
| Swallowing disorders | −3.052 | 1.303 | 5.486 | 0.019 | 0.047 | 0.004 | 0.608 | |
| History of aspiration | −2.587 | 0.900 | 8.255 | 0.004 | 0.075 | 0.013 | 0.439 | |
| Gastric retention | −0.608 | 0.990 | 0.378 | 0.539 | 0.544 | 0.078 | 3.787 | |
| Intra-abdominal hypertension | −1.691 | 0.939 | 3.244 | 0.072 | 0.174 | 0.029 | 1.161 | |
| Vomiting | −0.376 | 0.897 | 0.176 | 0.675 | 0.686 | 0.118 | 3.981 | |
| Spontaneous cough | −1.383 | 1.123 | 1.515 | 0.218 | 0.251 | 0.028 | 2.268 | |
| Gastrointestinal tumors | −2.301 | 1.048 | 4.820 | 0.028 | 0.100 | 0.013 | 0.781 | |
| Silent aspiration | Age | 0.203 | 0.100 | 4.125 | 0.042 | 1.226 | 1.007 | 1.492 |
| Mechanical ventilation | −1.429 | 0.775 | 3.397 | 0.065 | 0.240 | 0.052 | 1.095 | |
| Disorders of consciousness | 0.582 | 0.661 | 0.775 | 0.379 | 1.790 | 0.49 | 6.537 | |
| Swallowing disorders | −1.966 | 1.222 | 2.587 | 0.108 | 0.140 | 0.013 | 1.536 | |
| History of aspiration | −1.584 | 0.778 | 4.148 | 0.042 | 0.205 | 0.045 | 0.942 | |
| Gastric retention | −0.269 | 0.849 | 0.100 | 0.751 | 0.764 | 0.145 | 4.032 | |
| Intra-abdominal hypertension | −2.183 | 0.762 | 8.207 | 0.004 | 0.113 | 0.025 | 0.502 | |
| Vomiting | −0.088 | 0.759 | 0.013 | 0.908 | 0.916 | 0.207 | 4.052 | |
| Spontaneous cough | −1.968 | 0.900 | 4.778 | 0.029 | 0.140 | 0.024 | 0.813 | |
| Gastrointestinal tumors | −2.768 | 0.918 | 9.096 | 0.003 | 0.063 | 0.010 | 0.379 | |
SE, standard error; CI, confidence interval; OR, odds ratio.
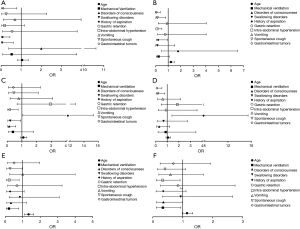
Table 8
| Group | Related factors | B | SE | Wald | P value | OR | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Overt aspiration | Age | 0.095 | 0.101 | 0.885 | 0.347 | 1.099 | 0.902 | 1.339 |
| Mechanical ventilation | −0.942 | 0.778 | 1.467 | 0.226 | 0.390 | 0.085 | 1.79 | |
| Disorders of consciousness | −1.992 | 0.746 | 7.137 | 0.008 | 0.136 | 0.032 | 0.588 | |
| Swallowing disorders | −1.579 | 0.759 | 4.331 | 0.037 | 0.206 | 0.047 | 0.912 | |
| History of aspiration | 1.396 | 0.681 | 4.206 | 0.040 | 4.038 | 1.064 | 15.326 | |
| Gastric retention | −1.740 | 0.736 | 5.584 | 0.018 | 0.176 | 0.041 | 0.743 | |
| Intra-abdominal hypertension | 1.076 | 0.752 | 20046 | 0.153 | 2.931 | 0.671 | 12.799 | |
| Vomiting | −0.242 | 0.699 | 0.120 | 0.729 | 0.785 | 0.2 | 3.089 | |
| Spontaneous cough | −0.785 | 0.781 | 1.010 | 0.315 | 0.456 | 0.099 | 2.107 | |
| Gastrointestinal tumors | −0.865 | 0.856 | 1.022 | 0.312 | 0.421 | 0.079 | 2.253 | |
| Silent aspiration | Age | 0.072 | 0.092 | 0.619 | 0.432 | 1.075 | 0.898 | 1.288 |
| Mechanical ventilation | −0.141 | 0.706 | 0.040 | 0.841 | 0.868 | 0.218 | 3.465 | |
| Disorders of consciousness | −1.161 | 0.691 | 2.818 | 0.093 | 0.313 | 0.081 | 1.215 | |
| Swallowing disorders | −0.377 | 0.707 | 0.284 | 0.594 | 0.686 | 0.172 | 2.744 | |
| History of aspiration | 1.539 | 0.612 | 6.320 | 0.012 | 4.658 | 1.404 | 15.456 | |
| Gastric retention | −0.098 | 0.698 | 0.020 | 0.888 | 0.907 | 0.231 | 3.557 | |
| Intra-abdominal hypertension | 0.626 | 0.691 | 0.821 | 0.365 | 1.871 | 0.482 | 7.253 | |
| Vomiting | −0.473 | 0.630 | 0.563 | 0.453 | 0.623 | 0.181 | 2.143 | |
| Spontaneous cough | −1.591 | 0.697 | 5.204 | 0.023 | 0.204 | 0.052 | 0.799 | |
| Gastrointestinal tumors | −2.117 | 0.778 | 7.402 | 0.007 | 0.120 | 0.553 | 0.026 | |
SE, standard error; CI, confidence interval; OR, odds ratio.
Table 9
| Group | Related factors | B | SE | Wald | P value | OR | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Overt aspiration | Age | 0.289 | 0.104 | 7.758 | 0.005 | 1.335 | 1.089 | 1.635 |
| Mechanical ventilation | −1.555 | 0.664 | 5.479 | 0.019 | 0.211 | 0.057 | 0.776 | |
| Disorders of consciousness | −1.120 | 0.671 | 2.791 | 0.095 | 0.326 | 0.088 | 1.214 | |
| Swallowing disorders | −0.178 | 0.667 | 0.071 | 0.789 | 0.837 | 0.226 | 3.092 | |
| History of aspiration | −1.292 | 0.699 | 3.414 | 0.065 | 0.275 | 0.070 | 1.082 | |
| Gastric retention | −0.397 | 0.804 | 0.243 | 0.622 | 0.673 | 0.139 | 3.253 | |
| Intra-abdominal hypertension | −1.492 | 0.643 | 5.381 | 0.020 | 0.225 | 0.064 | 0.793 | |
| Vomiting | 0.001 | 0.707 | 0.000 | 0.999 | 1.001 | 0.250 | 4.000 | |
| Spontaneous cough | −1.286 | 0.639 | 4.050 | 0.044 | 0.276 | 0.079 | 0.967 | |
| Gastrointestinal tumors | −0.682 | 6.695 | 0.962 | 0.327 | 0.506 | 0.129 | 1.975 | |
| Silent aspiration | Age | 0.133 | 0.079 | 2.847 | 0.092 | 1.143 | 0.979 | 1.334 |
| Mechanical ventilation | −1.092 | 0.524 | 4.340 | 0.037 | 0.336 | 0.120 | 0.937 | |
| Disorders of consciousness | −1.038 | 0.527 | 3.886 | 0.049 | 0.354 | 0.126 | 0.994 | |
| Swallowing disorders | −0.072 | 0.537 | 0.018 | 0.894 | 0.931 | 0.325 | 2.667 | |
| History of aspiration | −1.057 | 0.592 | 3.184 | 0.074 | 0.348 | 0.109 | 1.110 | |
| Gastric retention | −0.172 | 0.603 | 0.082 | 0.775 | 0.842 | 0.258 | 2.745 | |
| Intra-abdominal hypertension | −1.113 | 0.520 | 4.578 | 0.032 | 0.329 | 0.911 | 0.119 | |
| Vomiting | −0.532 | 0.538 | 0.979 | 0.322 | 0.587 | 0.204 | 1.686 | |
| Spontaneous cough | −0.894 | 0.503 | 3.156 | 0.076 | 0.409 | 0.153 | 1.097 | |
| Gastrointestinal tumors | −0.376 | 0.526 | 0.510 | 0.475 | 0.687 | 0.245 | 1.927 | |
SE, standard error; CI, confidence interval; OR, odds ratio.
Independent risk factors for silent aspiration in ICU elderly patients
We performed a multiple logistic regression analysis of the 10 independent factors in the single-factor analysis and found that age, history of aspiration, IAH, spontaneous cough, and gastrointestinal tumor had an effect on the occurrence of silent aspiration in the trans-pyloric feeding group and were risk factors for it (Table 7; Figure 3A,3B), whereas in the trans-pyloric feeding group, we found that history of aspiration, spontaneous cough, and gastrointestinal tumor significantly affected the incidence of silent aspiration. In the post-pyloric feeding group, mechanical ventilation, impaired consciousness, and IAH were independent risk factors for the occurrence of silent aspiration (Table 8; Figure 3C,3D).
Discussion
The incidence of aspiration is different in ICU elderly patients with different clinical features
Aspiration is a process in which a variable amount of food, oral secretions, or gastroesophageal reflux accidentally enters the airway under the voice box and the lungs during feeding due to lesions in the innervated motor nerves, which affect the function of the tongue muscles, soft palate, and pharynx (29). The occurrence of aspiration often leads to serious consequences, such as aspiration pneumonia, acute respiratory distress syndrome, pulmonary fibrosis, and even worse, death. Therefore, the clinical characteristics of each patient are different, and their probability of aspiration is also different (30). According to our findings, there was a significant difference between the aspiration group and the non-aspiration group in terms of age, whether they were taking gastrointestinal motility drugs, and if they had been bedridden for a long time (P<0.05). The incidence of aspiration was significantly higher in patients who were older, were not taking gastrointestinal motility drugs, and had a history of being bedridden for a long time.
The incidence of aspiration was different in ICU elderly patients with different feeding patterns
ICU patients are critically ill and have diverse and complex therapeutic measures. For critically ill elderly patients, early and reasonable gastrointestinal nutritional support can reduce protein depletion and malnutrition. Meanwhile, they also maintain the structure and function of the vital organs of the body (31). Therefore, nasal feeding has become the preferred mode of nutritional therapy for patients in the ICU. The results of this study showed that the differences in the incidence of overt aspiration among the oral feeding group, the gastric tube feeding group, and the post-pyloric feeding group were statistically significant (P<0.05). The incidence of aspiration was higher in the gastric tube feeding group than in the other 2 groups for both overt and silent aspiration. Some studies (3,32) have shown that the incidence of aspiration in ICU patients ranges from 8.80% to 46.73%. In our study, the incidence of overt aspiration in the gastric tube feeding group was 29.5% and the incidence of silent aspiration was 55%, indicating that the incidence of aspiration in elderly patients feeding through the gastric tube in ICU is still at a high level. The probability of overt aspiration and silent aspiration in the pyloric feeding group was lower than that in the gastric tube feeding group. This may be because nasogastric tube feeding requires the nutrient solution to be emptied through the stomach before entering the intestine, whereas the nasogastric tube nutrient solution can enter the intestine directly through the pylorus, effectively avoiding the occurrence of gastric retention due to gastric emptying obstacle. In addition, ICU patients not only receive nutrients through enteral nutrition, but also some of them receive nutrients through oral feeding, but there are few studies focusing on patients who receive nutrients through oral feeding (33). In our study, although the incidence of overt aspiration in the oral feeding group was only 15.5%, which was the lowest among the 3 groups, the incidence of silent aspiration was 52.4%, which was higher than that in the post-pyloric feeding group. Compared with the overt aspiration, the silent aspiration is insidious and difficult to diagnose, and may be more harmful to elderly patients than the overt aspiration. Therefore, health care professionals should pay attention to the problem of aspiration in elderly ICU patients who are fed orally, and it is necessary to assess the feeding ability of these patients and provide them with feeding education to minimize the possibility of aspiration and improve their prognosis.
The characteristics of overt aspiration were different in ICU elderly patients with different feeding patterns
In this study, analysis revealed that in the overt aspiration group, there were significant differences between the 3 groups in terms of whether the patients had swallowing disorders, gastric retention, IAH, whether they could cough spontaneously, and whether they needed mechanical ventilation (P<0.05). A two-way comparison showed that among patients with dysphagia and gastric retention, there were significant differences between the gastric tube feeding group and the other 2 groups. The incidence of dysphagia and gastric retention in the gastric tube feeding group was significantly higher than in the other 2 groups. Among the patients who could cough spontaneously or not and whether they needed mechanical ventilation, there were significant differences between the post-pyloric feeding group and other 2 groups, respectively. The percentage of patients who could not cough spontaneously and needed mechanical ventilation was significantly higher in the post-pyloric feeding group than in the other 2 groups. This may be due to the fact that ICU patients are in a critical condition, receive various and complex treatment measures, often require the placement of artificial airway catheters such as oropharyngeal ventilation tubes and tracheal intubation, as well as the use of enteral nutrition lines such as gastric and jejunal tubes, which artificially destroy the swallowing function and cough reflex of patients. The incidence of overt aspiration is significantly higher in ICU patients with dysphagia or requiring mechanical ventilation or are unable to cough on their own (34). Patients with overt aspiration often show symptoms such as irritant choking, abnormal pronunciation, shortness of breath, and sudden drop in oxygen saturation, and in severe cases, cyanosis and dyspnea may occur, which endanger the safety of patients (3). In clinical work, especially in the ICU ward, mechanical ventilation and the use of gastric or intestinal tubes are more common, and the resulting aspiration is more easily ignored. Therefore, for elderly patients in the ICU, in addition to focusing on whether the patient has gastric retention and IAH, medical and nursing staff should promptly assess the patient’s swallowing function and ability to cough on their own, and take targeted preventive measures early to reduce the occurrence of serious adverse consequences such as overt aspiration and aspiration pneumonia or even asphyxia.
The characteristics of silent aspiration were different in ICU elderly patients with different feeding patterns
The results of this study showed that among patients with silent aspiration, there were significant differences between the 3 groups in terms of whether they had impaired consciousness, dysphagia, vomiting, whether they could cough spontaneously, and whether they needed mechanical ventilation (P<0.05). The percentage of each characteristic was generally higher in the post-pyloric feeding group than in the oral feeding group, which was slightly different from the characteristics of the occurrence of overt aspiration. The results of the two-way comparison showed that in patients with impaired consciousness who were unable to cough spontaneously and were receiving mechanical ventilation, there was a significant difference between the post-pyloric feeding group and the other 2 groups (P<0.05). In contrast, in the comparison between the oral feeding group and the gastric tube feeding group, the difference between the 2 features of dysphagia and vomiting was statistically significant in the 2 groups (both P<0.05). The reason for this may be that when the patient is unconscious, the pharyngeal sensory perception is dulled and the swallowing function as well as the cough reflex is diminished or absent. In recent years, it has been shown that acquired swallowing disorders in ICU patients can be caused by disease, treatment, or other medical factors such as tracheal intubation. For example, 44–83% of mechanically ventilated patients have swallowing disorders after extubation (35,36). When patients have dysphagia or vomiting, food stays in the mouth for a long time and pharyngeal residues increase, resulting in accidental aspiration of food residues or oral secretions into the airway. The silent aspiration is often diagnosed only with the help of auxiliary means because of its insidious nature, and it has a certain lag, which may have a greater impact on the long-term prognosis of patients. Therefore, for these patients, medical and nursing staff should focus on whether patients fed through a gastric tube and orally are at high risk for silent aspiration, and dynamically assess the risk of silent aspiration in ICU patients with different feeding patterns in order to prevent occult aspiration at an early stage.
The risk factors of aspiration were different in ICU elderly patients with different feeding patterns
According to the study, the history of aspiration and gastrointestinal tumor were the common independent influencing factors for the occurrence on both overt and silent aspiration in the oral feeding group. In patients who experienced aspiration, their previous medical conditions were more severe, and they may have had sequelae such as swallowing disorders, which may predispose them to secondary aspiration, especially during the process of oral feeding. The US consensus for nutritional assessment and supportive treatment of critically ill patients also state that the history of aspiration is a risk factor for aspiration (6). Therefore, patients with the history of aspiration should be screened and evaluated early in the clinical setting, and a high degree of attention should be paid to this group of patients to reduce the incidence of aspiration by slowing down the feeding rate according to their specific conditions. In addition, our findings suggest that gastrointestinal tumors are a common and independent risk factor for both overt and silent aspiration. The reason for this is that the distal end of the patient's intraoperative nasogastric tube needs to be delivered to the jejunum 25–30 cm below the anastomosis. When the tracheal tube or gastric tube is removed after surgery, the nasogastric tube may be taken out of its intended position due to improper operation or excessive force, and if the tip of the tube stays in the esophagus or is entangled in the stomach, there is a high possibility of regurgitation of nutrient solution during the infusion of enteral nutrition, leading to aspiration. The thicker the diameter of the catheter, the greater the dilating and opening effect on the lower esophageal sphincter, which makes it more likely that regurgitation of gastric contents will occur and lead to accidental aspiration (37). Therefore, for elderly patients with gastrointestinal tumors, the possibility of aspiration should be dynamically assessed and every effort should be made to avoid serious consequences.
In the gastric tube feeding group, in addition to history of aspiration as a common independent influencing factor for both overt and silent aspiration, impaired consciousness, dysphagia, and gastric retention were independent risk factors for overt aspiration, whereas spontaneous cough and gastrointestinal tumor were independent risk factors for silent aspiration. In the ICU, 80% of elderly people experience impaired consciousness (38). When patients experience disordered consciousness, the pharyngeal sensory perception is blunted, and the swallowing function as well as the cough reflex are weakened or lost, which makes it easy for aspiration to occur. Metheny et al. (39) found that a Glasgow Coma Scale (GCS) score <9 (P=0.021) was a risk factor for aspiration in a prospective study of factors influencing aspiration involving 360 ICU enteral nutrition patients. In a study of risk factors for aspiration in patients with impaired consciousness in carbon monoxide poisoning, Sohn et al. (40) also concluded that a GCS score <8 was directly associated with aspiration in patients. Gastric retention is an important indicator to assess the tolerance of enteral nutrition and gastric emptying status of patients, and when the gastric retention reaches a certain threshold, it will cause an increase in intragastric pressure and intolerance such as nausea, vomiting, abdominal distention, and reflux of gastric contents, which will easily increase the risk of aspiration. This suggests that when patients have gastric retention, healthcare professionals should implement timely measures to monitor the amount of gastric residue; in severe cases, nasal feeding can be suspended to correct the patient’s gastrointestinal dysfunction and effectively avoid the occurrence of aspiration. When spontaneous cough is weakened or absent, the patient’s ability to clear respiratory secretions is also reduced, resulting in a large amount of secretions gathering in the respiratory tract and not being cleared in time, which can easily lead to aspiration. Therefore, for elderly patients in ICU, healthcare staff should encourage patients to cough as much as possible, so as to reduce the incidence of aspiration.
In the post-pyloric feeding group, mechanical ventilation and IAH were common independent influencing factors for the occurrence of both overt and covert aspiration. It has been shown that aspiration pneumonia due to aspiration accounts for 5–15% of hospitalized patients with pneumonia, and its mortality rate ranges from 20% to 65% (41,42). Mechanical ventilation is an effective measure commonly used in the clinical management of critically ill patients, which refers to the maintenance of patient airway patency, improvement of ventilation and oxygenation, and prevention of organismal hypoxia and carbon dioxide accumulation through ventilatory support (43). However, mechanical ventilation disrupts the patient’s swallowing and coughing reflexes, making the patient unable to defend themselves through swallowing and coughing mechanisms, thus predisposing them to aspiration. Another important independent factor is IAH, which is defined as a sustained or repeated increase in intra-abdominal pressure (IAP) ≥12 mmHg; when IAP ≥20 mmHg is combined with organ dysfunction and failure, it is defined as abdominal compartment syndrome (ACS) (44). According to the survey, 50–80% of critically ill adult patients will develop IAH during treatment, and 2.7–51.7% of critically ill patients will further develop ACS (45). The abdominal pressure increases with the degree of abdominal distension, which affects the organ function. In addition, increased IAP can lead to increased intestinal permeability and intestinal mucosal damage, which in turn affects the digestive and absorption functions of the intestine and further leads to reduced gastrointestinal motility and slowed gastric emptying. IAH can easily lead to gastric retention and gastrointestinal intolerance symptoms such as abdominal distention, vomiting, and gastric contents reflux, which in turn increases the risk of aspiration.
In conclusion, it is necessary to assess patients’ ability to eat and provide them with pre-feeding education for oral feeding. For patients who are fed through the gastric tube or through the post-pylorus, the possibility of aspiration should be assessed according to the patient’s condition and the presence of risk factors, and targeted measures such as encouraging voluntary coughing and gastrointestinal decompression should be taken in advance to reduce the possibility of aspiration.
The main shortcomings of this study were the insufficient case samples collected due to limited manpower and time, and the failure to follow up patient outcomes and survival. Future studies are recommended to expand the sample size and further follow-up of patients.
Conclusions
Among the elderly patients in the ICU, the incidence of aspiration, whether the overt or the silent was the highest in the gastric tube feeding group. There were significant differences in the influencing factors and characteristics of aspiration among the elderly patients in ICU with different feeding patterns. We should take personalized precautions early according to the characteristics and feeding patterns of patients, so as to reduce the possibility of aspiration.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-430/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-430/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-430/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-430/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Hai’an People’s Hospital (No. KYLC2022036). Informed consent was provided by all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Guo WA, Davidson BA, Ottosen J, et al. Effect of high advanced glycation end-product diet on pulmonary inflammatory response and pulmonary function following gastric aspiration. Shock 2012;38:677-84. [Crossref] [PubMed]
- Ashford A, Eastaugh-Waring T. Regurgitation and aspiration. Anaesthesia & Intensive Care Medicine 2021;22:621-4. [Crossref]
- Byun SE, Shon HC, Kim JW, et al. Risk factors and prognostic implications of aspiration pneumonia in older hip fracture patients: A multicenter retrospective analysis. Geriatr Gerontol Int 2019;19:119-23. [PubMed]
- Benjamin E, Haltmeier T, Chouliaras K, et al. Witnessed aspiration in trauma: Frequent occurrence, rare morbidity--A prospective analysis. J Trauma Acute Care Surg 2015;79:1030-6; discussion 1036-7. [Crossref] [PubMed]
- Jaillette E, Martin-Loeches I, Artigas A, et al. Optimal care and design of the tracheal cuff in the critically ill patient. Ann Intensive Care 2014;4:7. [Crossref] [PubMed]
- McClave SA, Martindale RG, Vanek VW, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 2009;33:277-316. [Crossref] [PubMed]
- Padar M, Starkopf J, Starkopf L, et al. Enteral nutrition and dynamics of citrulline and intestinal fatty acid-binding protein in adult ICU patients. Clin Nutr ESPEN 2021;45:322-32. [Crossref] [PubMed]
- Singer P, Blaser AR, Berger MM, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr 2019;38:48-79. [Crossref] [PubMed]
- Raghavendran K, Davidson BA, Knight PR, et al. Surfactant dysfunction in lung contusion with and without superimposed gastric aspiration in a rat model. Shock 2008;30:508-17. [Crossref] [PubMed]
- Raghavendran K, Davidson BA, Huebschmann JC, et al. Superimposed gastric aspiration increases the severity of inflammation and permeability injury in a rat model of lung contusion. J Surg Res 2009;155:273-82. [Crossref] [PubMed]
- Nakamura K. Aspiration pneumonia in elderly stroke patients in a convalescent rehabilitation ward: Risk factors and effects on recovery after stroke. Nihon Ronen Igakkai Zasshi 2020;57:45-52. [Crossref] [PubMed]
- Prather AD, Smith TR, Poletto DM, et al. Aspiration-related lung diseases. J Thorac Imaging 2014;29:304-9. [Crossref] [PubMed]
- Bakowitz M, Bruns B, McCunn M. Acute lung injury and the acute respiratory distress syndrome in the injured patient. Scand J Trauma Resusc Emerg Med 2012;20:54. [Crossref] [PubMed]
- Almirall J, Boixeda R, de la Torre MC, et al. Aspiration pneumonia: A renewed perspective and practical approach. Respir Med 2021;185:106485. [Crossref] [PubMed]
- Butler SG, Stuart A, Markley L, et al. Aspiration as a Function of Age, Sex, Liquid Type, Bolus Volume, and Bolus Delivery Across the Healthy Adult Life Span. Ann Otol Rhinol Laryngol 2018;127:21-32. [Crossref] [PubMed]
- Noguchi S, Yatera K, Kato T, et al. Impact of the number of aspiration risk factors on mortality and recurrence in community-onset pneumonia. Clin Interv Aging 2017;12:2087-94. [Crossref] [PubMed]
- Omura T, Matsuyama M, Nishioka S, et al. Association Between the Swallowing Reflex and the Incidence of Aspiration Pneumonia in Patients With Dysphagia Admitted to Long-term Care Wards: A Prospective Cohort Study of 60 Days. Arch Phys Med Rehabil 2021;102:2165-71. [Crossref] [PubMed]
- Sparn MB, Widmann B, Pietsch U, et al. Risk factors and outcomes of postoperative aspiration pneumonia in abdominal surgery patients: An exact matching and weighting analysis. Surgery 2021;170:1432-41. [Crossref] [PubMed]
- Xu Z, Chen J, Xu R. A randomised controlled study: efficacy of ICU nursing risk management combined with the cluster nursing model and its effect on quality of life and inflammatory factor levels of patients with acute respiratory distress syndrome and ventilator-associated pneumonia. Ann Palliat Med 2021;10:7587-95. [Crossref] [PubMed]
- Narawane A, Rappazzo C, Hawney J, et al. Vocal Fold Movement and Silent Aspiration After Congenital Heart Surgery. Laryngoscope 2022;132:701-5. [Crossref] [PubMed]
- Shay EO, Meleca JB, Anne S, et al. Natural history of silent aspiration on modified barium swallow studies in the pediatric population. Int J Pediatr Otorhinolaryngol 2019;125:116-21. [Crossref] [PubMed]
- Velayutham P, Irace AL, Kawai K, et al. Silent aspiration: Who is at risk? Laryngoscope 2018;128:1952-7. [Crossref] [PubMed]
- Marvin S, Thibeault SL. Predictors of Aspiration and Silent Aspiration in Patients With New Tracheostomy. Am J Speech Lang Pathol 2021;30:2554-60. [Crossref] [PubMed]
- Chang H, Zhao J, Zhang S, et al. Evaluation of effects of quantification of food thickness on prevention of aspiration in stroke patients with dysphagia. Chinese Journal of Nursing 2018;32-5.
- Jiang QX, Liu J, Liu YX. Pilot study on effects of two different angles of head of bed elevationon aspiration and pressure ulcers prevention for patients undergoing ventilation. Chinese Journal of Nursing 2016;51:927-32.
- Johnston N, Dettmar PW, Ondrey FG, et al. Pepsin: biomarker, mediator, and therapeutic target for reflux and aspiration. Ann N Y Acad Sci 2018;1434:282-9. [Crossref] [PubMed]
- Du X, Wang F, Hu Z, et al. The diagnostic value of pepsin detection in saliva for gastro-esophageal reflux disease: a preliminary study from China. BMC Gastroenterol 2017;17:107. [Crossref] [PubMed]
- Jaillette E, Brunin G, Girault C, et al. Impact of tracheal cuff shape on microaspiration of gastric contents in intubated critically ill patients: study protocol for a randomized controlled trial. Trials 2015;16:429. [Crossref] [PubMed]
- Sue Eisenstadt E. Dysphagia and aspiration pneumonia in older adults. J Am Acad Nurse Pract 2010;22:17-22. [Crossref] [PubMed]
- Gupte T, Knack A, Cramer JD. Mortality from Aspiration Pneumonia: Incidence, Trends, and Risk Factors. Dysphagia 2022;37:1493-500. [Crossref] [PubMed]
- Xiao Q, Wang YL, Wu Y, et al. Reflux and Aspiration of Gastric Contents and Its Influencing Factors of Patients in Neurosurgical ICU. Journal of Nursing(China) 2014;50-3.
- Hayashi M, Iwasaki T, Yamazaki Y, et al. Clinical features and outcomes of aspiration pneumonia compared with non-aspiration pneumonia: a retrospective cohort study. J Infect Chemother 2014;20:436-42. [Crossref] [PubMed]
- Chen S, Xian W, Cheng S, et al. Risk of regurgitation and aspiration in patients infused with different volumes of enteral nutrition. Asia Pac J Clin Nutr 2015;24:212-8. [PubMed]
- Zhou M, Hu K, Shi L, et al. Risk factors of acquired swallowing disorders among patients after cardiac surgery. Chinese Journal of Nursing 2016;51:420-3.
- Macht M, Wimbish T, Bodine C, et al. ICU-acquired swallowing disorders. Crit Care Med 2013;41:2396-405. [Crossref] [PubMed]
- Bordon A, Bokhari R, Sperry J, et al. Swallowing dysfunction after prolonged intubation: analysis of risk factors in trauma patients. Am J Surg 2011;202:679-82; discussion 682-3. [Crossref] [PubMed]
- Ferrer M, Bauer TT, Torres A, et al. Effect of nasogastric tube size on gastroesophageal reflux and microaspiration in intubated patients. Ann Intern Med 1999;130:991-4. [Crossref] [PubMed]
- Khan BA, Perkins AJ, Campbell NL, et al. Pharmacological Management of Delirium in the Intensive Care Unit: A Randomized Pragmatic Clinical Trial. J Am Geriatr Soc 2019;67:1057-65. [Crossref] [PubMed]
- Metheny NA, Clouse RE, Chang YH, et al. Tracheobronchial aspiration of gastric contents in critically ill tube-fed patients: frequency, outcomes, and risk factors. Crit Care Med 2006;34:1007-15. [Crossref] [PubMed]
- Sohn CH, Huh JW, Seo DW, et al. Aspiration Pneumonia in Carbon Monoxide Poisoning Patients with Loss of Consciousness: Prevalence, Outcomes, and Risk Factors. Am J Med 2017;130:1465.e21-6. [Crossref] [PubMed]
- DiBardino DM, Wunderink RG. Aspiration pneumonia: a review of modern trends. J Crit Care 2015;30:40-8. [Crossref] [PubMed]
- Pikus L, Levine MS, Yang YX, et al. Videofluoroscopic studies of swallowing dysfunction and the relative risk of pneumonia. AJR Am J Roentgenol 2003;180:1613-6. [Crossref] [PubMed]
- Lin Z, Huang X, Shan X. Development and validation of a survival prediction model for patients received mechanical ventilation in the intensive care unit: a large sample size cohort from the MIMIC database. Ann Palliat Med 2022;11:2071-84. [Crossref] [PubMed]
- Kirkpatrick AW, Roberts DJ, De Waele J, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med 2013;39:1190-206. [Crossref] [PubMed]
- Lee RK, Gallagher JJ, Ejike JC, et al. Intra-abdominal Hypertension and the Open Abdomen: Nursing Guidelines From the Abdominal Compartment Society. Crit Care Nurse 2020;40:13-26. [Crossref] [PubMed]
(English Language Editor: J. Jones)




