
Osteo-cartilaginous pain syndromes at the chest wall: results of costal cartilage excision
Highlight box
Key findings
• CCE is a safe treatment for various pain syndromes at the chest wall including slipping rib syndrome, 12th rib syndrome and iliocostal impingement syndrome that offers satisfying long-term results.
What is known and what is new?
• There are many causes of movement-related pain in the chest wall, of which the slipping rib syndrome is the best studied. In a heterogenous patient population, it is shown that CCE provides durable pain relief.
What is the implication, and what should change now?
• The pathology of the different chest wall pain syndromes varies and the overall frequency of the individual syndromes is rare. By grouping these clinical pictures into one group of diseases, osteo-cartilaginous pain syndromes, their understanding is simplified. With CCE, a surgical treatment approach is available that leads to freedom from pain in the majority of patients.
Introduction
Patients occasionally present themselves to thoracic surgery outpatient clinics with movement or posture related chest wall pain. In many patients, the pain is a direct result of previous severe chest injuries or previous thoracic surgery. However, after these secondary causes of pain have been excluded, a small group of patients remains in whom the pain syndrome cannot be explained by a previous chest injury. In the scientific literature, various pathological changes in the bony and cartilaginous sections of the ribs have been described which can lead to pain in the chest wall that can be triggered mechanically (Table 1) (1-8). Unfortunately, these rare osteo-cartilaginous pain syndromes (OCPSs) are still little known, even among thoracic surgeons, and often the pain complained by the patients cannot be clearly assigned to one of these pain syndromes. Diagnosis is often delayed due to non-specific clinical symptoms, unhelpful imaging results, and unclear etiology (9). In clinical practice, other diagnoses like urolithiasis, a cardiac- or pleural genesis are considered first.
Table 1
| Syndrome | Involved ribs | Pathogenesis | Most established treatment options | Reference |
|---|---|---|---|---|
| Cyriax syndrome/slipping rib syndrome/rib-tip syndrome | False ribs (8th–10th) | The cartilaginous rib tip abuts or slips under the upper rib due to hypermobility | Conservative treatment; partial rib resection with/without additional vertical plating | (1-5) |
| 12th rib syndrome | Floating ribs (11th–12th)* | Hypermobility of the affected rib | Conservative; partial rib resection | (6) |
| Iliocostal impingement syndrome | Lowest ribs (11th–12th) | Pathologically short distance between the lower ribs and the iliac crest | Conservative treatment; therapy of underlying hyperkyphosis/kyphoscoliosis; partial rib resection | (7,8) |
*, there are inconsistent definitions in the literature for 12th rib syndrome. The syndrome is described as related exclusively to the 12th rib, while others are stating that it is related to the 11th and 12th rib (6). OCPS, osteo-cartilaginous pain syndrome.
The origin for OCPS is attributed to an impingement of intercostal nerves by rib cartilages of the lower rib-cage during trunk movement. The pain is described as sharp, stabbing or burning sensation and may last from few minutes up to several days (3,10). A typical history with unilateral pain exacerbated by movement points to the diagnosis. This can be supported by reports of a popping or clicking sensation occurring with the painful movement (11). Imaging modalities including thoraco-abdominal computed tomography and magnetic resonance imaging (MRI) are useful to exclude other diseases but are not helpful to ensure OCPS diagnosis (3,4). Instead, OCPS diagnosis is made by a well conducted physical examination of the patient including the “hooking maneuver” (11,12). Recent studies show that dynamic high-frequency ultrasound has been established as a valuable tool for diagnosis of OCPS (3-5,13-15).
OCPS are usually treated by analgesics, physiotherapy or other conservative procedures with limited success (3,4). Therapeutic intercostal blocks with glucocorticoids, local anesthetics, or Botulinum toxin have a high chance of achieving temporary pain reduction, but not lasting pain relief (16,17). Surgical costal cartilage excision (CCE) has been shown to resolve symptoms (3,9,18). However, in larger studies, a failure rate exceeding 25% has been reported and additional surgical measures including rib stabilization have been suggested (14,19,20). Most studies were conducted in a pediatric population. Recently, Mazzella and coworkers reported CCE results in a series of 19 adult patients (21). Their analysis did not include patients with a preceding chest wall trauma.
In our clinical practice, we recurrently encounter patients OCPS pathology that emerged at first after a documented rib fracture. In those patients, the preceding chest wall injury had completely resolved and any persistent injury (e.g., non-union rib fractures, pseudoarthrosis) had been ruled out. Those patients likewise may benefit from CCE. Therefore, we assessed the clinical benefit of CCE for OCPS treatment in a heterogeneous patient cohort. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1479/rc).
Methods
Study design
We performed a retrospective case series from two institutions including OCPS patients that were treated by CCE from 2014 to 2022. Data collected included the first out-patient examination, the hospitalization and a follow-up examination after 5 to 10 weeks. OCPS was suspected in included patients based on the clinical examination. Other thoracic or abdominal pathologies as possible causes of pain had been ruled out in the patients beforehand.
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval was waived by the local Ethics Committees of Würzburg University Hospital and Magdeburg University Hospital in view of the retrospective nature of the study and all the procedures being performed were part of the routine care. Patient data are published in pseudonymised form, so that no informed consent is required from the patients.
Diagnostic work-up
Primary diagnostics consisted of a thorough history with a physical examination. The latter included the “hooking maneuver”: with the patient standing, the examiner hooks the fingers under the inferior margin of the ribs at the affected side and then carefully deflects them cranially. For a meaningful examination technique, the examiner has to work with a little force in order to be able to detect pathological changes in the chest wall and to avoid false positive findings. The maneuver is positive if it reproduces the pain or rib movement. Existing imaging (chest X-ray, computed tomography, MRI) was reviewed to exclude non-OCPS pathologies. For follow-up, the history and physical examination were repeated.
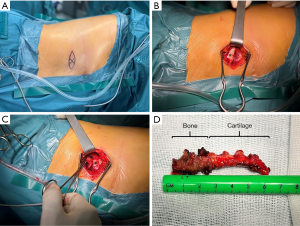
Surgical technique
All operations were conducted under general anaesthesia. The point of tenderness was marked preoperatively with the patient awake. Depending on OCPS localization, patients were positioned laterally or supine. The skin incision (3–5 cm) was made above the lesion and the perichondrium was isolated. The palpable end of the rib was mobilized and resected to allow for at least one finger widths distance to the superior rib (Figure 1). In every case, only one rib was operated on. Based on the existing rib morphology, rib pieces of different lengths had to be removed from different patients (approx. 2–4 cm). Care was taken to leave the parietal pleura intact. Depending on the soft tissue trauma, a Redon drainage was inserted.
Statistical analysis
Patient data included age, gender, body weight, body size, point of tenderness, time from first symptom to diagnosis, previous thoracic trauma or surgery, length of hospital stay and resolution of symptoms. If patients did not show up for follow-up, it was reported separately. Continuous variables are reported as mean and standard deviation. Categorical variables are reported as frequency and proportion. The statistical analysis has been performed by χ2 test for categorical variables and Student’s t-test and Mann-Whitney test for continuous variables, utilizing SPSS version 25.0 (SPSS Inc., Chicago, IL, USA). The difference was considered as significant for P values <0.05.
Literature review
We revisited the existing literature for cases of patients with Cyriax syndrome (CS) that underwent surgical treatment. PubMed was searched for “Cyriax syndrome” and for “slipping rib syndrome”. We included all literature published in the years 2012 till 2022 in English language describing case reports or case series with primary surgery for CS.
Results
The patients were operated consecutively at two different centers by the same surgical team.
Baseline patient characteristics
Our case series consists of 11 patients (72.7% female; median age, 43.5±17.1 years) (Table 2). Body mass index (BMI) was normal (23.6±3.4; range, 18.5–29.6 kg/m2). OCPS was present in 54.5% on the left side, 36.4% on the right side an in 9.1% bilateral. Three patients fulfilled the definition for CS and 8 patients for 12th rib syndrome (including 11th and 12th rib). While onset of symptoms were inexplicable in the majority of patients, five patients had preceding chest wall trauma. For three out of these patients, the preceding trauma was simultaneous with symptom onset. Average time between onset of symptoms and OCPS diagnosis was 2.6 years (range, 3–127 months).
Table 2
| Characteristics | Patient | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| Age (years) | 45 | 19 | 51 | 31 | 22 | 72 | 32 | 68 | 47 | 32 | 59 |
| Gender | Female | Male | Female | Female | Male | Female | Male | Female | Female | Female | Female |
| Heights (cm) | 169 | 187 | 170 | 154 | 183 | 152 | 179 | 158 | 170 | 169 | 166 |
| Weight (kg) | 56 | 80 | 63 | 51 | 85 | 55 | 79 | 74 | 85 | 71 | 51 |
| BMI (kg/m2) | 19.6 | 22.9 | 21.8 | 21.5 | 25.4 | 21.6 | 24.7 | 29.6 | 29.4 | 24.9 | 18.5 |
| Time from first symptom to diagnosis (weeks) | 34 | 50 | 400 | 13 | 52 | 550 | 81 | 26 | 39 | 21 | 260 |
| Anamnesis for trauma | Yes, side unknown | Yes, side unknown | Yes, ipsilateral | No | No | Yes, ipsilateral | No | Yes, bilateral | No | No | No |
| Clinically secondary OCPS | No | No | Yes | No | No | Yes | No | Yes | No | No | No |
| Hooking-maneuver performed | Yes, positive | Yes, positive | Yes, positive | Yes, positive | Yes, negative | Yes, positive | Yes, positive | Yes, positive | Yes, negative | Yes, positive | Yes, positive |
BMI, body mass index; OCPS, osteo-cartilaginous pain syndrome.
Surgical treatment
CCE was performed in all patients (Table 3). Patients received oral analgesics for postoperative pain control. The postoperative course was uneventful and all patients were discharged after 2.3±0.6 days. The histopathological work-up of the resected costal specimen was striking in two cases. Follow-up visits took place after 4–18 weeks. By then, OCPS symptomatic had ceased in all but two patients: 5 of 9 patients reported no residual pain (56%) and the remaining 4 patients reported a significant reduction in pre-operative discomfort. No patient underwent reoperation on the basis of recurrence. Two patients missed their follow-up appointments.
Table 3
| Parameters | Patient | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| Localization | C11 right | C11 right | C9 left | C11 left | C11 bilateral | C10 left | C11 left | C11 right | C11 right | C11 left | C9 left |
| Treatment | Partial resection of rib C11 | Partial resection of ribs C10/C11 | Partial resection of rib C9 | Partial resection of rib C11 | Partial resection of both ribs C11 | Partial resection of rib C10 | Partial resection of rib C11 | Partial resection of rib C11 | Partial resection of rib C11 | Partial resection of rib C11 | Partial resection of rib C9 |
| Histopathological result | NA | B-cell lymphocyte aggregation | Chronic periostitis | Unremarkable rib | Unremarkable ribs | Unremarkable rib | Unremarkable rib | Periosteal chondroma | Unremarkable rib | NA | Unremarkable rib |
| Discharge on postoperative day | 2 | 2 | 2 | 2 | 2 | 3 | 3 | 3 | 1 | 2 | 3 |
| Follow-up after discharge (weeks) | Patient failed to appear | 7 | 5 | 10 | 6 | 5 | 18 | 5 | 5 | 4 | Patient declined a follow-up |
| Follow-up result | – | Wound pain | No pain | No pain | No pain | Significant pain reduction | Mild persisting pain most likely intercostal neuralgia | Wound pain | Paresthesia, no pain | Paresthesia, no pain | – |
C, rib; NA, not available.
Discussion
In our analysis CCE for OCPS results in clear reduction in discomfort in all patients with half of the patients showing complete pain relief.
Postural or exercise dependent localized pain points at the costal arch may represent OCPS and need to be diagnosed by thoracic surgeons to be able to offer a sustainable treatment to patients. All the more since OCPS may handicap healthy adolescents and young athletes (4,5). Timely diagnosis requires clinical suspicion and skillful physical examination techniques since chest imaging is generally not helpful. Even though dynamic ultrasound has been shown to be helpful diagnosing CS (3-5,13-15).
Delayed diagnosis is common in OCPS due to a low degree of familiarity in the entire medical profession and thoracic surgeons alike (21). Patients may suffer for years until a focussed physical examination identifies the diagnosis. As a consequence, significant amounts of health care costs are spent on unhelpful imaging studies and secondary psychiatric diagnoses and treatments (5).
The pathogenesis of some OCPS is well understood: in CS it is the lack of cartilaginous or fibrous attachments of the ribs 7th to 10th building the costal arch (11,16,21). This impaired connection results in a non-physiological mobility of the ribs eventually culminating in an anterior or posterior subluxation following certain movements including deep breathing, sneezing, coughing and sitting. The costal tips may impinge the intercostal nerve running above the affected rib causing sharp, stabbing or burning sensations. Other possible components in pain development may be irritation of the periosteum, the perichondrium or the parietal pleura.
The 12th rib syndrome is the result of a hypermobility of the affected rib due to its lack of any bony attachments. The pain is than caused by irritation of the adjacent intercostal nerve. Similarly, a hypermobile 11th rib may cause comparable pain. In our experience, hypermobility of both floating ribs results in the same clinical symptoms and should be treated alike. Evidence regarding 12th rib syndrome is scarce. The existing literature suggest that analogous to CS 12th rib syndrome may be treated by partial rib resection, leading to long-lasting pain relief (6).
Iliocostal impingement syndrome on the other hand is associated with thoracic hyperkyphosis and kyphoscoliosis (7). In another case series, all patients had noticed a significant loss of height and the symptoms were associated with osteoporosis (8). Contact between the lowest rib and the iliac crest seems to be the cause of the pain (7,8). Literature regarding the treatment of iliocostal impingement is even further limited, but partial resections for these patients has been shown to offer relief of symptoms. (8). A different but interesting approach focussed on treatment of the underlying hyperkyphosis and kyphoscoliosis by a weighted kypho-orthosis and a back strengthening program, also led to successful pain management (7).
In our experience, patients with rib fractures, the bone fragments may dislocate and heal misaligned. In case of serial rib fractures, this effect may emerge at several broken ribs. The costal misalignment may translate into an axial deviation of the rib resulting in narrowing an intercostal space. The tip of the misaligned rib may now be able to impinge an intercostal nerve during certain movements that did not cause pain before the trauma.
Numerous clinical case series that were published in the past observed the emergence of CS in patients following chest trauma (Table 4) (9,10,16,17,19-27). In numerous additional case reports, respiratory diseases, pregnancy and childbirth have been suggested as yet other causes for CS (28). In one study, CS was diagnosed as an iatrogenic complication following thoracic surgery (29). In summary, patients benefitted from CCE and experienced sustained freedom from pain, although recent studies indicate that a relevant proportion of these patients retain pain over a long period of time and may further benefit from vertical plating in addition to CCE (19). Thus, our observation of OCPS emergence after chest trauma is not new. However, the shared patho-mechanism was not deducted from those clinical observations so far.
Table 4
| Publication | Patients in the case series [patients that received surgery for CS] | Surgical technique | History for trauma | Median age (years) | Follow-up of the patients that received surgery for CS |
|---|---|---|---|---|---|
| Zairi et al., 2019 (9) | 1 [1] | CCE | Acquired (subluxation of the 7th–9th ribs) | 36 | After 4 months, patient satisfied |
| Fu et al., 2012 (10) | 7 [7] | CCE | 2 patients with clinical CS and nonunion fractures were excluded | 16.1 | After 0.9 years, 1 patient with reoccurring pain at a different location, 1 with persistent but reduced pain |
| Foley et al., 2019 (16) | 54 [10] | CCE | 15 times posttraumatic | 19.1 | Date unknown, 7 patients reported relief of pain |
| van Delft et al., 2016 (17) | 1 [1] | CCE | Posttraumatic | 47 | After 2 months, no pain |
| Mazzella et al., 2020 (21) | 19 [19] | CCE | 3 times trauma reported | 41 | After 4 months, 14 patients recommend operation |
| Turcios, 2013 (22) | 1 [1] | CCE | No trauma reported | 15 | After 3 months, no pain |
| Alshammari et al., 2018 (23) | 17 [1] | CCE | Unknown | 14.9 | No pain at admission (thoracoscopic resection) |
| McMahon et al., 2021 (19) | 85 [70] | At initial surgery: 59% CCE and 41% CCE with plating | 21 inciting events | 17.7 | Mean follow-up after 2.97 years. 17.1% recurrent CS without additional plating, 3.4% recurrent CS with additional plating |
| Hansen et al., 2020 (24) | 42 [29] | Sutured rib fixation without resection | Unknown | 50 | After 6 months, in 80% pain improvement |
| Squillaro et al., 2020 (25) | 4 [4] | Laparoscopic CCE | No trauma reported | 16.5 | After 6 months, no pain |
| Romano et al., 2022 (26) | 4 [4] | CCE | Trauma excluded | 29.3 | Immediately and after 2 years no pain |
| Fraser et al., 2021 (20) | 49 [49] | CCE | Unknown | 15.4 | Median follow-up of 4.5 years, 11 reoperations, 72% complete cure, 83% rating their satisfaction >7/10 |
| MacGregor et al., 2022 (27) | 13 [13] | CCE | 2 posttraumatic | 12.5 | Median after 3.5 months, 91% improvement/resolution of symptoms, 9% continued use of opioids |
The PubMed database was searched for the terms “Cyriax syndrome” and “slipping rip syndrome”. The search was limited to publications between 2012 and 2022 in German or English language. CS, Cyriax syndrome; CCE, costal cartilage excision.
The published literature confirms our own clinical findings that both patients with primary and secondary OCPS benefit from CCE (Table 4). In all of our patients, CCE resulted in significant pain reduction or lasting freedom from pain. All of our patients that had a follow-up indicated to have an improvement in pain as well as function. Following the definition of recurrence as development of pain combined with exam findings consistent with OCPS requiring resection in the same area, we had no recurrences in our cohort (20).
Our analysis is limited by its retrospective approach, the small patient number and the heterogenous pathology of OCPS patients. Furthermore, our small study group does not allow for advanced statistical analyses, but larger studies also report positive results after CCE. The two largest case series (McMahon et al. and Fraser et al.) for CS show a recurrence rate after CCE alone of 17% and 22% (19,20). In their studies, McMahon et al. could reduce the recurrence rate to 3% with additional plating (19); Fraser et al. demonstrated a failure to complete cure of 28% after CCE, but they were also able to elucidate high levels of satisfaction after resection, even if complete cure was not perceived (20). The surgical procedure is limited to the chest wall preserving pleural integrity and therefore can be performed without single-lung ventilation. However, a modified surgical approach preserving the entire cartilage by suture fixation has been reported (24). Recently, a laparoscopic approach for CCE has been suggested for pediatric patients (2).
Conclusions
OCPS should be suspected in case of recurrent immobilizing pain of the lower chest and especially the costal arch. Physical examination with a positive “hooking maneuver” and dynamic ultrasound aid the diagnosis. CCE has been shown to be an effective and reliable treatment guaranteeing sustained pain relief.
Acknowledgments
The authors thank Jean-Marie Wihlm (Service de Chirurgie Thoracique, Strasbourg) for inspiring the work and Ivan Aleksic and Ina Schade (Department of Cardiothoracic Surgery, University Hospital of Würzburg) for their clinical support. Parts of the data presented in this manuscript were communicated at the 30th Annual Congress of the German Society for Thoracic Surgery (22–24 September 2021, Erfurt, Germany).
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1479/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1479/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1479/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1479/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval was waived by the local Ethics Committees of Würzburg University Hospital and Magdeburg University Hospital in view of the retrospective nature of the study and all the procedures being performed were part of the routine care. Patient data are published in pseudonymised form, so that no informed consent is required from the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cyriax EF. On various conditions that may simulate the referred pains of visceral disease, and a consideration of these from the point of view of cause and effect. Practitioner 1919;102:314-22.
- McBeath AA, Keene JS. The rib-tip syndrome. J Bone Joint Surg Am 1975;57:795-7. [Crossref] [PubMed]
- McMahon LE. Slipping Rib Syndrome: A review of evaluation, diagnosis and treatment. Semin Pediatr Surg 2018;27:183-8. [Crossref] [PubMed]
- Foley Davelaar CM. A Clinical Review of Slipping Rib Syndrome. Curr Sports Med Rep 2021;20:164-8. [Crossref] [PubMed]
- Gress K, Charipova K, Kassem H, et al. A Comprehensive Review of Slipping Rib Syndrome: Treatment and Management. Psychopharmacol Bull 2020;50:189-96. [PubMed]
- Urits I, Noor N, Fackler N, et al. Treatment and Management of Twelfth Rib Syndrome: A Best Practices Comprehensive Review. Pain Physician 2021;24:E45-50. [PubMed]
- Brubaker ML, Sinaki M. Successful management of iliocostal impingement syndrome: A case series. Prosthet Orthot Int 2016;40:384-7. [Crossref] [PubMed]
- Wynne AT, Nelson MA, Nordin BE. Costo-iliac impingement syndrome. J Bone Joint Surg Br 1985;67:124-5. [Crossref] [PubMed]
- Zairi S, Hadj Dahmane M, Attia M, et al. Cyriax syndrome: a misdiagnosed condition of the chest wall. Asian Cardiovasc Thorac Ann 2019;27:609-11. [Crossref] [PubMed]
- Fu R, Iqbal CW, Jaroszewski DE, et al. Costal cartilage excision for the treatment of pediatric slipping rib syndrome. J Pediatr Surg 2012;47:1825-7. [Crossref] [PubMed]
- Fares MY, Dimassi Z, Baydoun H, et al. Slipping Rib Syndrome: Solving the Mystery of the Shooting Pain. Am J Med Sci 2019;357:168-73. [Crossref] [PubMed]
- Heinz GJ, Zavala DC. Slipping rib syndrome. JAMA 1977;237:794-5. [Crossref] [PubMed]
- Patel NG, Patel DM, Patel MV, et al. Diagnostic Value of Dynamic High-frequency Ultrasound for the Slipping Rib and Twelfth Rib Syndrome: A Case Series with Review. Curr Med Imaging 2021;17:459-63. [Crossref] [PubMed]
- Van Tassel D, McMahon LE, Riemann M, et al. Dynamic ultrasound in the evaluation of patients with suspected slipping rib syndrome. Skeletal Radiol 2019;48:741-51. [Crossref] [PubMed]
- Girbau A, Álvarez-Rey G, Cano-Herrera CL, et al. Slipping rib syndrome: A clinical and dynamic-sonographic entity. A serial cases report. J Back Musculoskelet Rehabil 2022;35:253-9. [Crossref] [PubMed]
- Foley CM, Sugimoto D, Mooney DP, et al. Diagnosis and Treatment of Slipping Rib Syndrome. Clin J Sport Med 2019;29:18-23. [Crossref] [PubMed]
- van Delft EA, van Pul KM, Bloemers FW. The slipping rib syndrome: A case report. Int J Surg Case Rep 2016;23:23-4. [Crossref] [PubMed]
- Gould JL, Rentea RM, Poola AS, et al. The effectiveness of costal cartilage excision in children for slipping rib syndrome. J Pediatr Surg 2016;51:2030-2. [Crossref] [PubMed]
- McMahon LE, Salevitz NA, Notrica DM. Vertical rib plating for the treatment of slipping rib syndrome. J Pediatr Surg 2021;56:1852-6. [Crossref] [PubMed]
- Fraser JA, Briggs KB, Svetanoff WJ, et al. Long-term outcomes and satisfaction rates after costal cartilage resection for slipping rib syndrome. J Pediatr Surg 2021;56:2258-62. [Crossref] [PubMed]
- Mazzella A, Fournel L, Bobbio A, et al. Costal cartilage resection for the treatment of slipping rib syndrome (Cyriax syndrome) in adults. J Thorac Dis 2020;12:10-6. [Crossref] [PubMed]
- Turcios NL. Slipping rib syndrome in an adolescent: an elusive diagnosis. Clin Pediatr (Phila) 2013;52:879-81. [Crossref] [PubMed]
- Alshammari DM, Talon I, Rod J, et al. Thoracoscopic Rib Resection in Children. J Laparoendosc Adv Surg Tech A 2018;28:106-10. [Crossref] [PubMed]
- Hansen AJ, Toker A, Hayanga J, et al. Minimally Invasive Repair of Adult Slipped Rib Syndrome Without Costal Cartilage Excision. Ann Thorac Surg 2020;110:1030-5. [Crossref] [PubMed]
- Squillaro AI, Sanders K, Onwubiko C, et al. Laparoscopic Treatment of Slipping Rib Syndrome in Pediatric Patients. J Laparoendosc Adv Surg Tech A 2020;30:1253-6. [Crossref] [PubMed]
- Romano R, Gavezzoli D, Gallazzi MS, et al. A new sign of the slipping rib syndrome? Interact Cardiovasc Thorac Surg 2022;34:331-2. [Crossref] [PubMed]
- MacGregor RM, Schulte LJ, Merritt TC, et al. Slipping Rib Syndrome in Children: Natural History and Outcomes Following Costal Cartilage Excision. J Surg Res 2022;280:204-8. [Crossref] [PubMed]
- Parry W, Breckenridge I, Khalil YF. Bilateral clicking ribs. Thorax 1989;44:72-3. [Crossref] [PubMed]
- Patel N, John JK, Pakeerappa P, et al. Slipping rib syndrome: case report of an iatrogenic result following video-assisted thoracic surgery and chest tube placement. Pain Manag 2021;11:555-9. [Crossref] [PubMed]


