
The association between the MELD-XI score and heart failure in patients with acute myocardial infarction after coronary artery stenting-a retrospective study
Highlight box
Key findings
• The model for end-stage liver disease (MELD) score shows good ability in assessing the cardiac function of patients with acute myocardial infarction.
What is known and what is new?
• The MELD score is a marker used to evaluate end-stage liver disease in patients with liver failure, and existing scholars have found that the MELD score is also valuable in evaluating heart diseases such as heart failure.
• The MELD score without international normalized ratio (MELD-XI) can better evaluate cardiac function in patients with acute myocardial infarction, which is of certain significance in predicting the prognosis of patients.
What is the implication, and what should change now?
• MELD-XI may be useful for clinicians to determine the severity of the condition in patients with acute myocardial infarction.
Introduction
In recent years, with the increasing incidence of hypertension, diabetes, hyperlipidemia, and other diseases, the incidence of acute myocardial infarction has gradually risen in kind (1,2). Coronary artery stenting is the main means of treating acute myocardial infarction, with the main purpose being to restore blood flow to the ischemic myocardium, preventing recurrent myocardial infarction, and thus improving the prognosis of patients. Although medical technology has been greatly improved, acute myocardial infarction is still one of the main factors of death in middle-aged and older adult patients, mainly because heart failure or recurrent myocardial infarction can occur after acute myocardial infarction, resulting in death (3-5). Therefore, it is crucial to predict the long-term prognosis of patients with acute myocardial infarction after coronary artery stenting and to identify the risk factors of poor prognosis. N-terminal pro-B-type natriuretic peptide (NT-proBNP) was the most commonly used predictor in patients with acute myocardial infarction after coronary artery stenting. However, the predictive value of NT-proBNP was limited in patients complicated with renal insufficiency. The model for end-stage liver disease (MELD) score is a marker used to evaluate end-stage liver disease in patients with liver failure, and existing researchers have found that the MELD score is also valuable for evaluating heart diseases such as heart failure (6). Patients with heart failure and myocardial infarction often use anticoagulants, but this can affect the international normalized ratio (INR). Therefore, removing the INR from the MELD score to form the MELD-XI score may more accurately evaluate the cardiac function in patients with heart failure (7). Due to a lack of data in this area, this study was conducted to determine the association between the MELD-XI score and heart failure in patients with acute myocardial infarction after coronary artery stenting. We present this article in accordance with the STARD reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-562/rc).
Methods
General information
This was a retrospective study. The data of 318 patients with acute myocardial infarction admitted to The People’s Hospital of Dazu from January 2018 to January 2021 was retrospectively collected. According to the MELD-XI score on admission, the patients were divided into a high-MELD-XI score group (n=159) and a low-MELD-XI score group (n=159). The inclusion criteria were the following: (I) acute myocardial infarction, (II) coronary artery stenting implantation, (III) age ≥18 years old, and (IV) complete data. Meanwhile, the exclusion criteria were the following: (I) hepatic and renal insufficiency, (II) malignant tumors, (III) congenital heart disease, (IV) biliary tract diseases, (V) history of liver and kidney transplantation, (VI) chronic blood system diseases, and (VII) other major diseases. This study was approved by the Ethics Committee of The People’s Hospital of Dazu (No. c20210048) which exempted this study from informed consent. This study was conducted in accordance with the 2013 revision of the Declaration of Helsinki.
MELD-XI score
On admission, the MELD-XI score was calculated for each patient as follows: MELD-XI = 5.11 × In (Natural logarithm)bilirubin + 11.76 × Increatinine + 9.44. If the result was less than ≤1, the MELD-XI value was always treated as 1.
Data collection
Data on age, sex, body mass index, smoking history, history of alcoholism, hypertension, diabetes, hyperlipidemia, left ventricular ejection fraction, NT-proBNP, recurrent myocardial infarction, stent thrombosis, heart failure, and death were collected. Patients were followed up for 1 year after surgery by clinical visits and cellphone.
Treatment methods
Patients in both groups were given coronary artery stenting, and dual antiplatelet therapy was administered up to 1 year after surgery. Patients with hypertension, diabetes, or hyperlipidemia were provided with hypoglycemic, hypotensive, or lipid-lowering treatment, respectively.
Statistical analysis
SPSS 26.0 (IBM Corp., Armonk, NY, USA) software was used to complete the data analysis, with a P value <0.05 indicating a statistical difference (2-sided test). The count data of the 2 groups are expressed as the number and percentage, and the difference between groups was analyzed with the chi-squared test. The measurement data of both groups are expressed as mean ± standard deviation, and the difference between groups was analyzed with the independent samples t-test. The predictive value of the MELD-XI for the prognosis of patients with acute myocardial infarction after coronary artery stenting was analyzed using the receiver operating characteristic (ROC) curve.
Results
Comparison of general data between 2 groups
There was no significant difference in age, gender, body mass index, smoking history, alcohol history, hypertension, diabetes mellitus, or and hyperlipidemia between the 2 groups (P>0.05; Table 1).
Table 1
| Characteristic | High-MELD-XI score group (n=159) | Low-MELD-XI score group (n=159) | t/χ2 value | P value |
|---|---|---|---|---|
| Age (years) | 63.73±4.82 | 64.02±5.01 | 0.526 | 0.599 |
| Gender (male) | 80 (50.31) | 86 (54.09) | 0.454 | 0.501 |
| Body mass index (kg/m2) | 24.58±1.92 | 24.81±1.85 | 1.088 | 0.278 |
| History of smoking | 21 (13.21) | 25 (15.72) | 0.407 | 0.524 |
| History of alcoholism | 18 (11.32) | 21 (13.21) | 0.263 | 0.608 |
| Hypertension | 102 (64.15) | 108 (67.92) | 0.505 | 0.477 |
| Diabetes | 43 (27.04) | 35 (22.01) | 1.087 | 0.297 |
| Hyperlipidemia | 134 (84.28) | 131 (82.39) | 0.204 | 0.652 |
Data are presented as mean ± standard error or n (%). MELD-XI, model for end-stage liver disease with no international normalized ratio.
Comparison of left ventricular ejection fraction and NT-proBNP between the 2 groups
Compared with that in the low-MELD-XI score group, the left ventricular ejection fraction in the high-MELD-XI score group was significantly reduced (51.61%±7.66% vs. 60.48%±5.94%; P<0.001), while the level of NT-proBNP increased significantly in the high-MELD-XI score group (821.58±461.81 vs. 723.51±335.16 ng/L; P=0.031; Table 2).
Table 2
| Characteristic | High-MELD-XI score group (n=159) | Low-MELD-XI score group (n=159) | t value | P value |
|---|---|---|---|---|
| Left ventricular ejection fraction (%) | 51.61±7.66 | 60.48±5.94 | 11.534 | <0.001 |
| NT-proBNP (ng/L) | 821.58±461.81 | 723.51±335.16 | 2.167 | 0.031 |
Data are presented as mean ± standard error. NT-proBNP, N-terminal pro-B-type natriuretic peptide; MELD-XI, model for end-stage liver disease with no international normalized ratio.
Comparison of prognosis between the 2 groups
Compared with that in the low-MELD-XI score group, the incidence of recurrent myocardial infarction in the high-MELD-XI score group was significantly increased (10.69% vs. 3.77%; P=0.017); the incidence of heart failure was significantly higher in the high-MELD-XI score group (24.53% vs. 2.52%; P<0.001), as was mortality (5.66% vs. 1.26%; P=0.032; Table 3).
Table 3
| Characteristic | High-MELD-XI score group (n=159) | Low-MELD-XI score group (n=159) | χ2 value | P value |
|---|---|---|---|---|
| Recurrent myocardial infarction | 17 (10.69) | 6 (3.77) | 5.671 | 0.017 |
| Stent thrombus | 12 (7.55) | 11 (6.92) | 0.047 | 0.829 |
| Heart failure | 39 (24.53) | 4 (2.52) | 32.943 | <0.001 |
| Mortality | 9 (5.66) | 2 (1.26) | 4.614 | 0.032 |
Data are presented as n (%). MELD-XI, model for end-stage liver disease with no international normalized ratio.
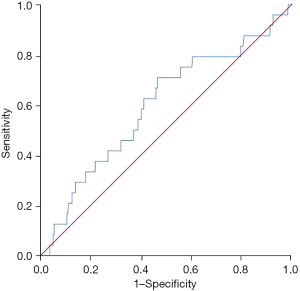
Predictive value of MELD-XI score for recurrent myocardial infarction in patients with acute myocardial infarction after coronary artery stenting
The MELD-XI score had no significant predictive value for recurrent myocardial infarction in patients with acute myocardial infarction after coronary artery stenting, and the area under the curve was 0.596 (95% CI: 0.474–0.728; P=0.118; Figure 1).
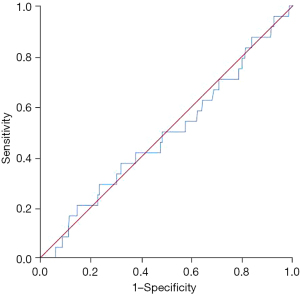
Predictive value of MELD-XI score for stent thrombosis in patients with acute myocardial infarction after coronary artery stenting
The MELD-XI score had no obvious predictive value for stent thrombus in patients with acute myocardial infarction after coronary artery stenting, and the area under the curve was 0.491 (95% CI: 0.368–0.613; P=0.877; Figure 2).
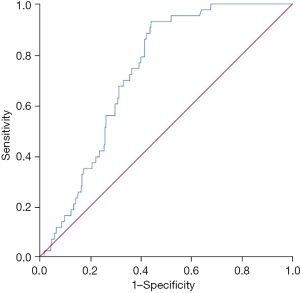
Predictive value of MELD-XI score in patients with acute myocardial infarction after coronary artery stenting
The MELD-XI score had a degree of predictive value for heart failure in patients with acute myocardial infarction after coronary artery stenting, and the area under the curve was 0.730 (95% CI: 0.670–0.791; P<0.001; Figure 3).
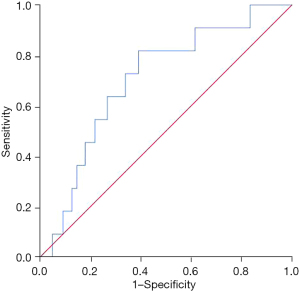
Predictive value of MELD-XI score for death after coronary artery stenting in patients with acute myocardial infarction
The MELD-XI score had a degree of predictive value for death after coronary artery stenting in patients with acute myocardial infarction, and the area under the curve was 0.704 (95% CI: 0.564–0.843; P=0.022; Figure 4).
Correlation between MELD-XI and left ventricular ejection fraction and NT-proBNP in patients with acute myocardial infarction after coronary artery stenting
The MELD-XI score was significantly negatively correlated with left ventricular ejection fraction (r=–0.444; P<0.001). There was no significant correlation between MELD-XI and NT-proBNP (r=0.068; P=0.224; Figure 5).

Discussion
Different biological indicators have been investigated for determining the early prognosis of different diseases to enable early treatment and the discovery of new therapeutic targets for improving prognosis (8-11). In order to predict the prognosis of patients after coronary artery stenting in patients with acute myocardial infarction, researchers have studied a variety of indicators, including NT-proBNP (12-15). However, these have thus far proven insufficient; for instance, NT-proBNP is elevated in patients with renal insufficiency, and thus it is difficult to accurately predict the prognosis of patients; consequently, the development of better biological indicators is needed. The present study examined the predictive value of MELD-XI score in patients with acute myocardial infarction after coronary artery stenting and found that the MELD-XI score correlated with left ventricular ejection fraction and had certain value in predicting postoperative heart failure and death.
In 2010, at the 61st annual meeting of the American Association for the Study of Liver Disease, it was proposed that the MELD score can predict the prognosis of patients with heart failure, with a higher MELD score indicating a worse the prognosis (6). The MELD score is calculated using a formula based on INR, creatinine, and bilirubin levels. Because patients with heart disease often use anticoagulants that can affect INR levels, INR was removed in the MELD to form the MELD-XI scores. When heart failure occurs, cardiac output decreases, blood supply to the liver decreases, and ischemic damage occurs. Furthermore, venous blood stasis can also lead to congestion, resulting in liver cell damage and elevated bilirubin. In addition, in heart failure patients, renal hypoperfusion causes the body to activate the neurosympathetic system, resulting in further reduction of renal blood flow and eventually elevated creatinine, which is how the MELD-XI score predicts patient prognosis. One study found that the MELD-XI score can be used as a risk stratification tool for older adult patients with ST-segment elevation myocardial infarction requiring coronary artery stenting, with MELD-XI ≥13 being a risk factor of poor prognosis (7). Another study showed that the MELD-XI score had a good predictive value in the prognosis of older adult patients with non-ST-segment elevation myocardial infarction (16), which is consistent with the findings of our study. We further found that the MELD-XI score correlated with the left ventricular ejection fraction, which has certain value in predicting postoperative heart failure and death, as left ventricular ejection fraction is an important measure of cardiac function. Reduced left ventricular ejection fraction indicates a decrease in cardiac function (17-20), and thus an increased MELD-XI score may be associated with reduced cardiac function after coronary artery stenting in patients with acute myocardial infarction, and ultimately with a poor prognosis.
Limitations
This study employed a retrospective clinical design with a postoperative follow-up of only 1 year, and thus fewer deaths occurred than might be expected with a longer follow-up. Moreover, this was a retrospective study, therefore the results may be subject to selection bias and confounding factors. In addition, this was a single center study. Large-sample studies with long-term follow up are needed to confirm the predictive value of MELD-XI score for the long-term prognosis of patients with acute myocardial infarction. Finally, the study did not provide information on the interobserver variability in MELD-XI score calculations. Future studies should evaluate the interobserver agreement of MELD-XI score calculations to ensure its reliability and validity.
Conclusions
The MELD-XI score can better evaluate the cardiac function of patients with acute myocardial infarction after coronary artery stenting implantation and may thus be valuable for predicting prognosis.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-562/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-562/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-562/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-562/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Ethics Committee of The People’s Hospital of Dazu (No. c20210048) which exempted this study from informed consent. This study was conducted in accordance with the 2013 revision of the Declaration of Helsinki.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhdan VM, Oksak GA, Radomskyi OV, et al. Epidemiology of acute myocardial infarction in Ukraine and Poltava region. Wiad Lek 2018;71:751-6. [PubMed]
- Deng D, Liu L, Xu G, et al. Epidemiology and Serum Metabolic Characteristics of Acute Myocardial Infarction Patients in Chest Pain Centers. Iran J Public Health 2018;47:1017-29. [PubMed]
- Yeo YH, Wang M, He X, et al. Excess risk for acute myocardial infarction mortality during the COVID-19 pandemic. J Med Virol 2023;95:e28187. [Crossref] [PubMed]
- Cheng SY, Wang H, Lin SH, et al. Association of admission hyperglycemia and all-cause mortality in acute myocardial infarction with percutaneous coronary intervention: A dose-response meta-analysis. Front Cardiovasc Med 2022;9:932716. [Crossref] [PubMed]
- Vieira RCP, Marcolino MS, Silva LGSE, et al. Assessment of the Impact of the Implementation of a Pre-Hospital Ambulance System on Acute Myocardial Infarction Mortality in a Developing Country. Arq Bras Cardiol 2022;119:756-63. [PubMed]
- Gotou M, Suzuki A, Shiga T, et al. Implication of modified MELD scores for postdischarge prognosis in hospitalized patients with heart failure. Heart Vessels 2023;38:535-42. [Crossref] [PubMed]
- He SJ, Weng JX, Chen HJ, et al. The prognostic value of MELD-XI in elderly patients with ST-segment elevation myocardial infarction: an observational study. BMC Cardiovasc Disord 2021;21:53. [Crossref] [PubMed]
- Chen Y, Wang J, Zhang X, et al. Correlation between apparent diffusion coefficient and pathological characteristics of patients with invasive breast cancer. Ann Transl Med 2021;9:143. [Crossref] [PubMed]
- Qi A, Li Y, Yan S, et al. Effect of postoperative chemotherapy on blood glucose and lipid metabolism in patients with invasive breast cancer. Gland Surg 2021;10:1470-7. [Crossref] [PubMed]
- Qi A, Li Y, Yan S, et al. Effect of anthracycline-based postoperative chemotherapy on blood glucose and lipid profiles in patients with invasive breast cancer. Ann Palliat Med 2021;10:5502-8. [Crossref] [PubMed]
- Teng D, Xia S, Hu S, et al. miR-887-3p Inhibits the Progression of Colorectal Cancer via Downregulating DNMT1 Expression and Regulating P53 Expression. Comput Intell Neurosci 2022;2022:7179733. [Crossref] [PubMed]
- Shen T, Yang X, Zhang Z. Positive Relationship of RDW with NT-proBNP and cTnI in Acute Myocardial Infarction Patients. Clin Lab 2022; [Crossref] [PubMed]
- McLeod P, Coffey S, Sneddon K, et al. Clinically Acquired High Sensitivity Cardiac Troponin T is a Poor Predictor of Reduced Left Ventricular Ejection Fraction After ST Elevation Myocardial Infarction: A National Cohort Study-ANZACS-QI 65. Heart Lung Circ 2022;31:1513-23. [Crossref] [PubMed]
- Firani NK, Hartanti KD, Purnamasari P. Hematological Parameter as Predictor Mortality in Acute Myocardial Infarction Patients. Int J Gen Med 2022;15:6757-63. [Crossref] [PubMed]
- Duhin OA, Kalinskaya AI, Rusakovich GI, et al. The state of platelet and plasma hemostasis as a predictor of coronary blood flow in patients with acute myocardial infarction. Kardiologiia 2022;62:31-7. [Crossref] [PubMed]
- Çınar T, Şaylık F, Selçuk M, et al. The predictive value of the MELD-XI score for short- and long-term mortality in elderly patients with non-ST elevation myocardial infarction. Aging Clin Exp Res 2022;34:887-95. [Crossref] [PubMed]
- Mahdavi-Roshan M, Ghorbani Z, Gholipour M, et al. Evaluation of cardiometabolic risk markers linked to reduced left ventricular ejection fraction (LVEF) in patients with ST-elevation myocardial infarction (STEMI). BMC Cardiovasc Disord 2022;22:224. [Crossref] [PubMed]
- Heber S, Haller PM, Kiss A, et al. Association of Plasma Methylglyoxal Increase after Myocardial Infarction and the Left Ventricular Ejection Fraction. Biomedicines 2022;10:605. [Crossref] [PubMed]
- Hanada K, Sasaki S, Seno M, et al. Reduced Left Ventricular Ejection Fraction Is a Risk for Sudden Cardiac Death in the Early Period After Hospital Discharge in Patients With Acute Myocardial Infarction. Circ J 2022;86:1490-8. [Crossref] [PubMed]
- Butcher SC, Lustosa RP, Abou R, et al. Prognostic implications of left ventricular myocardial work index in patients with ST-segment elevation myocardial infarction and reduced left ventricular ejection fraction. Eur Heart J Cardiovasc Imaging 2022;23:699-707. [Crossref] [PubMed]


