AB 84. Pharmacokinetics of moxifloxacin in patients with severe exacerbations of COPD
Background: Although moxifloxacin is widely used in patients with COPD exacerbation, its penetration in bronchial secretions has not been evaluated sufficiently. This study aims to investigate pk/pd of moxifloxacin in serum and secretions of patients with severe exacerbations of COPD.
Patients and methods: 13 patients, age 70.77±8.39 years, with presumably infectious exacerbation of COPD were included. 4 patients were admitted in the ICU and 9 in common chambers. All patients received 400 mg intravenous moxifloxacin o.d. and all samples were taken in steady state condition. Venous blood samples were obtained at 0/1/1.5/2/3/4/6/9/12 and 24 hours and bronchial secretions were taken in 0/2/4/6/9/12 and 24 hours. Plasma and bronchial secretions concentrations were measured by a HPLC method using fluorescence detection and pharmacokinetic parameters were determined by the use of WinNonlin software. Penetration was expressed as AUCsecretions/ AUCplasma ratio. Pharmacodynamic target attainment was estimated for the MICs of the most common respiratory pathogens (AUC24/ MIC>30 for Gram positive and >125 for Gram negative pathogens). Drug concentrations in bronchial secretions of patients admitted in the ICU were compared to those of the patients hospitalized in common chambers.
Results: Table 1.
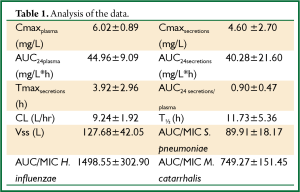
Full table
pk/pd parameters were similar in both groups with the exception of Cmax in ICU patients bronchial secretions which was lower compared to non critically ill patients (2.5 vs. 5.53 mg/L) but the difference only reached marginal statistical significance (P=0.058).
Conclusions: Moxifloxacin penetration in bronchial secretions in patients with severe exacerbation of COPD appears to be sufficient (90%). Pharmacodynamic target is attained for the most common pathogens, regardless of the required level of care. Lower Cmax in bronchial secretions of ICU patients could be attributed to a variety of reasons, including the co-existence of clinically appreciable hemodynamic alterations.


