
Chest vs. neck anastomotic leak post esophagectomy for malignancy: rate, predictors, and outcomes
Highlight box
Key findings
• Intrathoracic anastomotic leaks, following esophagectomy for malignancy, were associated with greater odds of needing an intervention but were not associated with higher morbidity or mortality, when compared with cervical anastomotic leaks.
What is known and what is new?
• Some surgeons avoid performing Ivor-Lewis esophagectomies due to the belief that an anastomotic leak in the chest is associated with increased morbidity and mortality.
• With the utilization of the most contemporary National Surgical Quality Improvement Project data, our study has compared the outcomes of Ivor-Lewis esophagectomies with McKeown and Transhiatal esophagectomies.
What is the implication, and what should change now?
• As surgeons continue to perform esophagectomies for esophageal cancer, we must continue to evaluate outcomes data to ensure patients continue to receive the best care. This study demonstrates similar outcomes in patients who develop an anastomotic leak postoperatively, whether the anastomosis was made in the chest or in the neck.
Introduction
Esophageal cancer is one of the most common cancers worldwide and continues to remain associated with a poor prognosis. The incidence of esophageal adenocarcinoma in the United States has recently begun to decline while the incidence of esophageal squamous cell carcinoma has been decreasing since 1986 (1,2). Esophagectomy continues to remain the mainstay of treatment in cases of certain early stage and locally advanced esophageal cancer.
Esophagectomy continues to carry a significant risk of associated morbidity and mortality. An anastomotic leak is one of the most feared complications with esophagectomies and has been associated with an increased morbidity and a reduction in overall survival (3). The surgical approach is dependent on multiple factors, including tumor location, extent of desired lymphadenectomy, and surgeon expertise and preference (4). Numerous studies and meta-analyses have been conducted, evaluating oncologic outcomes between the different surgical approaches for esophagectomy. Data from these studies have indicated that surgical approach has no significant influence on oncologic outcomes (5-8). Although there is significant variance in current literature, anastomotic leaks following esophagectomy are reported between 10–25% for cervical anastomoses and 3–25% for intrathoracic anastomoses (9,10). Prior studies have hypothesized a difference in complication rates by whether the anastomosis was made in the neck versus the chest (11,12).
There is a gap in the literature regarding a multicenter study assessing the contemporary practice of different esophagectomy techniques with a focus on the evaluation of morbidity and mortality associated with anastomotic leaks in the chest versus in the neck. Using a large national surgical database, we aim to investigate the rate and predictors of anastomotic leak following esophagectomy and compare outcomes of chest versus neck anastomotic leaks. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-37/rc).
Methods
Database and patient population
The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database including targeted files for esophagectomy was queried for patients who underwent esophagectomy for esophageal cancer between 2015 and 2019. The ACS-NSQIP contains over 135 variables captured from de-identified surgical cases performed in participating hospitals. These variables include preoperative characteristics, intraoperative events, and postoperative outcomes within 30 days of the operation.
The Current Procedural Terminology (CPT) codes 43107, 43117, 43112 were used to identify patients who underwent esophagectomy with Transhiatal, Ivor Lewis, and McKeown approach, respectively. Only patients with the following International Classification of Diseases (ICD) codes for malignant esophageal cancer diagnosis were included: ICD-9 codes: 150 Malignant neoplasm of esophagus, 150.0 Malignant neoplasm of cervical esophagus, 150.1 Malignant neoplasm of thoracic esophagus, 150.2 Malignant neoplasm of abdominal esophagus, 150.3 Malignant neoplasm of upper third of esophagus, 150.4 Malignant neoplasm of middle third of esophagus, 150.5 Malignant neoplasm of lower third of esophagus, 150.8 Malignant neoplasm of other specified part of esophagus, and 150.9 Malignant neoplasm of esophagus, unspecified site. ICD-10 codes included were C15 Malignant neoplasm of esophagus, C15.3 Malignant neoplasm of upper third of esophagus, C15.4 Malignant neoplasm of middle third of esophagus, C15.5 Malignant neoplasm of lower third of esophagus, C15.8 Malignant neoplasm of overlapping sites of esophagus, and C15.9 Malignant neoplasm of esophagus, unspecified.
Those with metastatic disease, the American Society of Anesthesiologists Physical Status Classification (ASA Class) of five, and cases done in emergent settings were excluded from the study. Patients who underwent esophagectomy for benign pathologies were not included given the heterogenicity in outcomes in these cases. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Given the de-identified nature of the data, this study was deemed exempt by the institutional review board at Virginia Commonwealth University, and individual consent for this retrospective analysis was waived.
Patient demographics and clinical characteristics, and study outcomes
The patients were classified into two groups; patients who underwent Ivor Lewis esophagectomy [ILE, chest leak (CL)] and patients who underwent transhiatal esophagectomy (THE) or McKeown esophagectomy [ME, neck leak (NL)]. The following preoperative variables were studied: demographic and anthropomorphic information [age, gender, body mass index (BMI)], ASA class, lab values (pre-operative white blood cell (WBC) count, creatinine, and albumin), smoking (within the last year), history of comorbid conditions (diabetes mellitus, hypertension, chronic obstructive pulmonary disease (COPD), congestive heart failure, and chronic renal failure requiring dialysis. The primary surgeon specialty: thoracic surgery or general surgery were compared. Oncological data included tumor size (T), nodal involvement (N), staging, pathology (adenocarcinoma, squamous cell carcinoma, others), and positive resection margin in addition to perioperative chemotherapy and radiation were recorded.
Patients who had leak were reported by ACS-NSQIP and were classified whether interventional means were required. Postoperative adverse outcomes included: pneumonia, pulmonary embolism (PE), prolonged intubation (>48 hours), unplanned re-intubation, wound infection, urinary tract infection (UTI), acute renal failure, myocardial infarction (MI), bleeding requiring transfusion, stroke, sepsis, numeric length of stay (truncated to the nearest day), extended length of hospital stay (>6 days), and 30-day mortality. Other postoperative outcomes included: rates of discharge to a facility, reoperation, and readmission.
Within the group of patients with chest anastomoses, patients with leak were compared to patients without leak and the same comparison was performed within the neck anastomoses patients. Separate analyses were performed to determine the predictors of each type of leak. An adjusted analysis was then performed to determine if the outcomes of patients with chest leaks differed from those with neck leaks. The outcomes investigated were pneumonia, unplanned intubation, sepsis, a leak requiring intervention, any postoperative complication, and 30-day mortality.
Statistical analyses
Continuous variables were presented as mean ± standard deviation (SD) or median and IQR and compared between the surgical groups using Wilcoxon signed-rank test, whereas categorical variables were summarized via frequency and percentage and compared using Pearson’s Chi-squared or Fisher’s exact test. For the adjusted analysis, multivariable linear or logistic regression models with a backward selection procedure via Akaike information criterion (AIC) were constructed to determine predictors of each type of leak and postoperative complications associated with each leak type. Covariates considered in the model building process were preoperative demographics, comorbidities, oncological characteristics, surgical approach, and surgeon specialty. Differences or odds ratios along with 95% confidence intervals were computed for each of the estimated parameters in the model. IBM SPSS Statistics for Windows, Version 27 (IBM Corp., Armonk, NY, USA) and SAS V9.4 (SAS Institute, Cary, NC, USA) were used for all analyses and statistical significance was determined if P<0.05.
Results
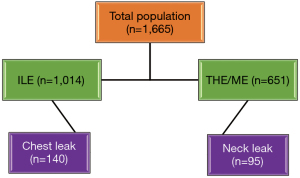
Throughout the study time period, 1,665 patients underwent esophagectomy for esophageal malignancy with 235 (14.1%) reported post-operative leak. One thousand and fourteen patients (61%) underwent ILE, of which 140 patients (13.8%) experienced a chest leak. Six hundred and fifty-one patients (39%) underwent THE or ME, of which 95 (14.6%) experienced a neck leak (Figure 1).
Chest leak: pre-operative characteristics, comorbidities, and cancer staging
The mean age of patients who underwent an ILE was 65.0 years old and 85.2% (n=864) of these patients were males, 28.3% (n=287) of patients had a history of smoking and 25.9% (n=263) had >10% weight loss prior to surgery. Eight hundred and sixty-eight patients (85.6%) had an ASA classification of three or four. Patients who experienced a chest leak had significantly higher rates of diabetes and a significantly higher BMI compared to patients without leak. Oncological data are demonstrated in Table 1. Adenocarcinoma was the most common pathological cause of malignancy detected (n=888).
Table 1
| Variables | No leak (N=874) | Leak (N=140) | P value |
|---|---|---|---|
| Age (years) | 65.00 (58.00–71.00) | 65.00 (59.50–71.00) | 0.407 |
| Male gender | 747 (85.47) | 117 (83.57) | 0.557 |
| BMI (Kg/m2) | 26.62 (23.11–30.18) | 27.98 (24.82–31.94) | 0.008 |
| Pre-operative serum creatinine (mg/dL) | 0.81 (0.70–0.97) | 0.88 (0.75–1.03) | 0.016 |
| Pre-operative serum albumin (g/dL) | 3.90 (3.60–4.20) | 3.90 (3.60–4.10) | 0.335 |
| Diabetes | 50 (5.72) | 21 (15.00) | <0.001 |
| Smoking (within one year) | 242 (27.69) | 45 (32.14) | 0.277 |
| COPD | 79 (9.04) | 8 (5.71) | 0.192 |
| CHF (30 days before surgery) | 4 (0.46) | 0 (0.00) | 0.423 |
| Hypertension (on medications) | 403 (46.11) | 87 (62.14) | <0.001 |
| Weight loss (>10% last 6 months) | 239 (27.35) | 24 (17.14) | 0.011 |
| Steroid use for chronic condition | 17 (1.95) | 2 (1.43) | 0.610 |
| ASA classification | 0.034 | ||
| ASA Class 1 & 2 | 134 (15.23) | 12 (8.57) | |
| ASA Class 3 & 4 | 740 (84.77) | 128 (91.43) | |
| Total operative time (minutes) | 340.00 (271.00–438.00) | 396.00 (311.00–484.00) | <0.001 |
| Surgeon specialty | 0.079 | ||
| Thoracic surgery | 617 (70.92) | 89 (63.57) | |
| General surgery | 253 (29.08) | 51 (36.43) | |
| T (tumor) stage | 0.675 | ||
| T0/Tis | 84 (10.05) | 16 (12.21) | |
| T1 | 199 (23.80) | 36 (27.48) | |
| T2 | 168 (20.10) | 21 (16.03) | |
| T3 | 375 (44.86) | 57 (43.51) | |
| T4 | 10 (1.20) | 1 (0.76) | |
| N (node) stage | 0.477 | ||
| N0 | 467 (55.93) | 71 (53.38) | |
| N1 | 207 (24.79) | 31 (23.31) | |
| N2 | 109 (13.05) | 24 (18.05) | |
| N3 | 52 (6.23) | 7 (5.26) | |
| Pathology | 0.164 | ||
| Adenocarcinoma | 760 (87.06) | 128 (91.43) | |
| Squamous cell | 71 (8.13) | 5 (3.57) | |
| Other malignancy | 42 (4.81) | 7 (5.00) | |
| Perioperative chemotherapy† | 628 (71.85) | 90 (64.29) | 0.100 |
| Perioperative radiotherapy† | 528 (60.41) | 78 (55.71) | 0.404 |
Continuous variables are presented as median (range) and categorical variables as number (percentage). †, within 90 days of surgery. BMI, body mass index; COPD, chronic obstructive pulmonary disease; CHF, congestive heart failure; ASA, American Society of Anesthesiologists.
Chest leak: complications, outcomes, and independent predictors
Thirty-day postoperative complications and outcomes following ILE are presented in Table 2. Patients who experienced a chest leak had significantly higher rates of pneumonia, prolonged intubation >48 hours, reintubation, sepsis, cardiac arrest, and bleeding requiring transfusions than patients who did not experience a chest leak. Length of stay was significantly longer in patients who experienced a chest leak (16 vs. 9 days, P<0.001) and a significantly larger number of patients remained the hospital over 30 days (20.00% vs. 2.75%, P<0.001). There were also higher rates of reoperation, readmission, and 30-day mortality in patients who experienced a chest leak.
Table 2
| Complications | No leak (N=874) | Leak (N=140) | P value |
|---|---|---|---|
| Pneumonia | 109 (12.47) | 49 (35.00) | <0.001 |
| Prolonged intubation >48 hours | 65 (7.44) | 38 (27.14) | <0.001 |
| Unplanned intubation | 76 (8.70) | 34 (24.29) | <0.001 |
| Urinary tract infection | 17 (1.95) | 3 (2.14) | 0.876 |
| Sepsis | 28 (3.20) | 24 (17.14) | <0.001 |
| Cardiac arrest requiring CPR | 9 (1.03) | 5 (3.57) | 0.017 |
| Myocardial infarction | 7 (0.80) | 1 (0.71) | 0.914 |
| Acute renal failure | 10 (1.14) | 4 (2.86) | 0.107 |
| Bleeding requiring transfusion | 87 (9.95) | 24 (17.14) | 0.011 |
| Reoperation | 88 (10.07) | 85 (60.71) | <0.001 |
| Length of stay (days) | 9.00 (7.00–12.00) | 16.00 (9.00–24.00) | <0.001 |
| Length of stay >6 days | 770 (88.10) | 119 (85.00) | 0.300 |
| Length of stay >30 days | 24 (2.75) | 28 (20.00) | <0.001 |
| 30-day operative mortality | 22 (2.52) | 9 (6.43) | 0.013 |
| Discharge destination | <0.001 | ||
| Death | 19 (2.19) | 13 (10.40) | |
| Home | 751 (86.52) | 98 (78.40) | |
| Other facility | 98 (11.29) | 14 (11.20) | |
| Readmission | 73 (8.35) | 34 (24.29) | <0.001 |
Continuous variables are presented as median (range) and categorical variables as number (percentage). CPR, Cardiopulmonary resuscitation.
Neck leak: pre-operative characteristics, comorbidities, and cancer staging
The mean age of patients who underwent a THE or ME was 65.0 years old and 83.9% (n=546) of these patients were males, 24.0% (n=156) of patients had a history of smoking and 21.0% (n=137) had >10% weight loss prior to surgery. Five hundred and forty-eight (84.2%) of patients undergoing THE or ME had an ASA classification of three or four (Table 3). Adenocarcinoma was the most common pathological cause of malignancy detected (n=539).
Table 3
| Variables | No leak (N=556) | Leak (N=95) | P value |
|---|---|---|---|
| Age (years) | 66.00 (58.00–71.00) | 65.00 (58.00–71.00) | 0.937 |
| Male gender | 470 (84.53) | 76 (80.00) | 0.267 |
| BMI (kg/m2) | 26.92 (23.86–30.45) | 27.24 (24.63–32.14) | 0.203 |
| Pre-operative serum creatinine | 0.83 (0.70–0.98) | 0.87 (0.70–1.10) | 0.260 |
| Pre-operative serum albumin | 3.80 (3.50–4.10) | 3.90 (3.50–4.20) | 0.900 |
| Diabetes | 26 (4.68) | 16 (16.84) | <.001 |
| Smoking (within one year) | 131 (23.56) | 25 (26.32) | 0.561 |
| COPD | 39 (7.01) | 10 (10.53) | 0.231 |
| CHF (30 days before surgery) | 3 (0.54) | 0 (0.00) | 0.473 |
| Hypertension (on medications) | 268 (48.20) | 50 (52.63) | 0.425 |
| Weight loss (>10% last 6 months) | 117 (21.04) | 20 (21.05) | 0.998 |
| Steroid use for chronic condition | 17 (3.06) | 2 (2.11) | 0.610 |
| ASA classification | 0.233 | ||
| ASA Class 1 & 2 | 91 (16.40) | 11 (11.58) | |
| ASA Class 3 & 4 | 464 (83.60) | 84 (88.42) | |
| Total operative time (minutes) | 302.00 (228.50–420.00) | 370.00 (243.00–445.00) | 0.020 |
| Surgeon specialty | 0.426 | ||
| Thoracic surgery | 223 (40.11) | 34 (35.79) | |
| General surgery | 333 (59.89) | 61 (64.21) | |
| T (tumor) stage | 0.426 | ||
| T0/Tis | 63 (12.19) | 14 (15.73) | |
| T1 | 165 (31.91) | 25 (28.09) | |
| T2 | 88 (17.02) | 20 (22.47) | |
| T3 | 195 (37.72) | 28 (31.46) | |
| T4 | 6 (1.16) | 2 (2.25) | |
| N (node) stage | 0.520 | ||
| N0 | 323 (61.17) | 48 (53.93) | |
| N1 | 114 (21.59) | 24 (26.97) | |
| N2 | 61 (11.55) | 10 (11.24) | |
| N3 | 30 (5.68) | 7 (7.87) | |
| Pathology | 0.378 | ||
| Adenocarcinoma | 457 (82.34) | 82 (88.17) | |
| Squamous cell | 73 (13.15) | 8 (8.60) | |
| Other malignancy | 25 (4.50) | 3 (8.60) | |
| Perioperative chemotherapy† | 384 (69.69) | 64 (68.09) | 0.755 |
| Perioperative radiotherapy† | 343 (62.25) | 58 (61.70) | 0.919 |
Continuous variables are presented as mean ± SD and categorical variables as number (percentage). †, within 90 days of surgery. BMI, body mass index; COPD, chronic obstructive pulmonary disease; CHF, congestive heart failure; ASA, American Society of Anesthesiologists; SD, standard deviation.
Neck leak: complications, outcomes, and independent predictors
Thirty-day postoperative complications and outcomes following THE and ME are presented in Table 4. Bleeding requiring transfusion, pneumonia, and reintubation were the three most common complications. Patients who experienced a neck leak had significantly higher rates of pneumonia, prolonged intubation >48 hours, reintubation, sepsis, cardiac arrest, and acute renal failure than patients who did not experience a neck leak. Length of stay was significantly longer in patients who experienced a neck leak (15 vs. 8 days, P<0.001). There was a significantly larger number of patients who remained the hospital over 30 days if postoperative course was complicated by a neck leak (15.79% vs. 3.24%, P<0.001). There were also higher rates of reoperation, readmission, and 30-day mortality in patients who experienced a neck leak.
Table 4
| Complications | No leak (N=556) | Leak (N=95) | P value |
|---|---|---|---|
| Pneumonia | 61 (10.97) | 21 (22.11) | 0.003 |
| Prolonged Intubation >48 hours | 36 (6.47) | 20 (21.05) | <0.001 |
| Unplanned intubation | 46 (8.27) | 29 (30.53) | <0.001 |
| Urinary tract infection | 8 (1.44) | 1 (1.05) | 0.766 |
| Sepsis | 14 (2.52) | 22 (23.16) | <0.001 |
| Cardiac arrest requiring CPR | 10 (1.80) | 5 (5.26) | 0.038 |
| Myocardial infarction | 6 (1.08) | 2 (2.11) | 0.402 |
| Acute renal failure | 2 (0.36) | 3 (3.16) | 0.004 |
| Bleeding requiring transfusion | 67 (12.05) | 16 (16.84) | 0.196 |
| Reoperation | 63 (11.33) | 51 (53.68) | <0.001 |
| Length of stay (days) | 8.00 (7.00–11.00) | 15.00 (10.00–22.00) | <0.001 |
| Length of stay >6 days | 438 (78.78) | 81 (85.26) | 0.146 |
| Length of stay >30 days | 18 (3.24) | 15 (15.79) | <0.001 |
| 30-day operative mortality | 11 (1.98) | 7 (7.37) | 0.003 |
| Discharge destination | <0.001 | ||
| Mortality | 11 (2.01) | 8 (9.09) | |
| Home | 491 (89.76) | 59 (67.05) | |
| Other facility | 45 (8.23) | 21 (23.86) | |
| Readmission | 48 (8.71) | 22 (23.16) | <0.001 |
Continuous variables are presented as mean ± SD and categorical variables as number (percentage). CPR, cardiopulmonary resuscitation; SD, standard deviation.
Comparing chest leak vs. neck leak
Preoperatively, the patients had comparable comorbidities and oncological characteristics (Table S1). Table 5 demonstrates the comparison of complications and outcomes with chest leaks and neck leaks. The only significant complication that was seen in the chest leak group when compared with the neck leak group was pneumonia (35.00% vs. 22.11%, P=0.034). Rates of PE, prolonged intubation, reintubation, UTI, sepsis, MI, acute renal failure, and bleeding requiring transfusion were similar between the chest leak and neck leak groups. Additionally, a significant association between the type of anastomotic leak and the management was identified, although there was no difference in reoperation rates between chest and neck leaks. The length of stay, discharge destination, mortality rate, and readmission rate were similar between the chest leak and neck leak groups.
Table 5
| Complications | Chest leak (N=140) | Neck leak (N=95) | P value |
|---|---|---|---|
| Pneumonia | 49 (35.00) | 21 (22.11) | 0.034 |
| Prolonged intubation >48 hours | 38 (27.14) | 20 (21.05) | 0.288 |
| Unplanned intubation | 34 (24.29) | 29 (30.53) | 0.289 |
| Urinary tract infection | 3 (2.14) | 1 (1.05) | 0.526 |
| Sepsis | 24 (17.14) | 22 (23.16) | 0.254 |
| Cardiac arrest requiring CPR | 5 (3.57) | 5 (5.26) | 0.528 |
| Myocardial infarction | 1 (0.71) | 2 (2.11) | 0.351 |
| Acute renal failure | 4 (2.86) | 3 (3.16) | 0.894 |
| Bleeding requiring transfusion | 24 (17.14) | 16 (16.84) | 0.952 |
| Reoperation | 85 (60.71) | 51 (53.68) | 0.284 |
| Management | 0.021 | ||
| Non-interventional means | 15 (10.71) | 20 (21.05) | |
| Interventional means | 57 (40.71) | 30 (31.58) | |
| Length of stay (days) | 16.00 (9.00–24.00) | 15.00 (10.00–22.00) | 0.599 |
| Length of stay >6 days | 119 (85.00) | 81 (85.26) | 0.956 |
| Length of stay >30 days | 28 (20.00) | 15 (15.79) | 0.413 |
| 30-day operative mortality | 9 (6.43) | 7 (7.37) | 0.779 |
| Discharge destination | 0.049 | ||
| Expired | 13 (10.40) | 8 (9.09) | |
| Home | 98 (78.40) | 59 (67.05) | |
| Other facility | 14 (11.20) | 21 (23.86) | |
| Readmission | 34 (24.29) | 22 (23.16) | 0.842 |
Continuous variables are presented as mean ± SD and categorical variables as number (percentage). CPR, cardiopulmonary resuscitation; SD, standard deviation.
Independent predictors and outcomes associated with anastomotic leak
An adjusted analysis looking into predictors of post esophagectomy anastomotic leak can be seen in Table 6. The use of chronic steroids, diabetes mellitus, hypertension, esophageal cancer (stage N2 vs. N0), and operative time were all significantly associated with chest leak. When evaluating factors independently associated with neck leaks, diabetes mellitus and operative time were significant positive predictors.
Table 6
| Chest leak | OR/estimate | OR (95% CI) | P value |
|---|---|---|---|
| Chronic steroids use | 2.547 | 1.069–6.068 | 0.034 |
| Thoracic vs. general surgeon specialty | 0.676 | 0.448–1.019 | 0.061 |
| Diabetes mellitus | 2.347 | 1.269–4.343 | 0.006 |
| Hypertension on medications | 2.021 | 1.352–3.022 | <0.001 |
| Esophageal cancer stage N2 vs. N0 | 1.916 | 1.112–3.303 | 0.019 |
| Operative time (per 30 minutes increase) | 1.062 | 1.014–1.113 | 0.011 |
| Neck leak | |||
| Pre-operative WBC | 1.101 | 0.996–1.216 | 0.059 |
| Diabetes mellitus | 3.587 | 1.745–7.372 | <0.001 |
| Operative time (per 30 minutes increase) | 1.059 | 1.003–1.117 | 0.037 |
OR, odds ratio; CI, confidence interval; WBC, white blood cell.
Of all post-operative outcomes examined, there was significantly greater odds of a patient with an intrathoracic leak requiring an intervention (OR: 0.166, P=0.001), however, the anastomosis site did not correlate with an increase in morbidities (Table 7).
Table 7
| Independent outcomes | OR/estimate | OR (95% CI) | P value |
|---|---|---|---|
| Pneumonia | 0.563 | 0.298–1.064 | 0.077 |
| Unplanned Intubation | 1.148 | 0.608–1.064 | 0.670 |
| Sepsis | 1.917 | 0.948–3.877 | 0.070 |
| Leak requiring intervention | 0.166 | 0.056–0.494 | 0.001 |
| Any complications | 0.880 | 0.489–1.584 | 0.670 |
| Mortality | 0.884 | 0.273–2.870 | 0.838 |
NL, neck leak; CL, chest leak; OR, odds ratio; CI, confidence interval.
Discussion
Esophagectomy techniques have progressed over time, but complications are still seen in over one-third of cases (13). Anastomotic leak continues to be a feared and costly complication following esophagectomy as it has a significant impact on patient morbidity and mortality (14). Prior studies have demonstrated an increased risk for leak with cervical anastomosis due to the need for a gastric conduit to be placed higher which can place increased tension on the anastomosis and compromise the vascular supply (15,16). Some surgeons continue to advocate for a cervical anastomosis, with knowledge of this increased risk, due to the thought that the sequelae of a cervical anastomotic leak are less severe, as the leak can drain from the cervical wound (17). We found there to be a lack of contemporary research comparing the risk factors, complications, and outcomes of chest anastomotic leaks with neck anastomotic leaks. In our study, we demonstrated a lack of statistical difference in many complications and outcomes in patients with a chest anastomotic leak compared with a neck leak.
Although chronic steroid use was not significantly associated with chest or neck leak in the preoperative characteristics of the study, after multivariate analysis, it was found to be an independent predictor of chest leaks following an ILE. Chronic steroid use suppresses the immune system which has been shown to delay wound and intestinal healing (18). With this finding, surgeons may consider substituting/weaning of steroids or a cervical anastomosis in patients who cannot be weaned off steroids prior to their esophagectomy.
Additionally, hypertension was found to be a predictor of a chest anastomotic leak in patients with an intrathoracic anastomosis. Uncontrolled hypertension is known to contribute to macrovascular disease and affects the microvasculature of the gastrointestinal tract, mainly in the serosal layer. Although the submucosal layer is believed to be the most important layer in anastomotic healing, the submucosa receives its blood supply from the serosal plexus. Diseased vasculature in the proximal serosal vessels, may lead to decreased blood flow and healing of the submucosal layer in patients with hypertension (19,20).
In our study, we found multiple complications that were significantly associated with an anastomotic leak, whether in the chest or in the neck. Pulmonary complications, including pneumonia, prolonged intubation (>48 hours), and reintubation, were higher. Patients undergoing esophagectomy regardless of experiencing an anastomotic leak are at increased risk of postoperative aspiration pneumonia due to the loss of the lower esophageal sphincter and distension of the gastric conduit in the thoracic cavity (21). When comparing pneumonia occurrence between intrathoracic and cervical leaks, the was no significant difference in the odds of one type of leak versus the other. Sepsis was higher in patients who experienced leak compared to patients without leak but was not more prevalent in the chest leak group which contradicts the belief that performing a cervical anastomosis would decrease the risk of sepsis. During this investigation, we found that overall hospital length of stay, prolonged admission, and 30-day mortality rate were all significantly increased in patients experiencing anastomotic leaks, whether chest or neck secondary to aforementioned complications. Higher rates of sepsis, pneumonia, reintubation, and cardiac arrest have been associated with prolonged length of stay and increased mortality rates (22,23).
Through multivariable regression, we identified a lack of differences in outcomes between chest and neck leaks, although chest leaks were found to have greater odds of requiring an intervention, A possible explanation for the lack of differences between chest and neck anastomotic leaks could be due to the implementation of interventional techniques that are currently used for intrathoracic leaks. Kauer et al. demonstrated that covered metal stents are an effective treatment option for intrathoracic anastomotic leaks (24). Stenting across a cervical anastomosis has been studied and found to be technically challenging and resulted in the development of new problems, including migration, overgrowth, and major erosive complications (25). Although the placement of an esophageal stent across an intrathoracic anastomosis requires additional procedures to place and remove the stent, the feared complication of an uncontrolled chest leak can be controlled, further reducing morbidity and mortality. To avoid the risk of stent migration, endoluminal vacuum (EndoVAC) therapy has recently become increasingly utilized for intrathoracic anastomotic leaks following esophagectomy (26). Similar to the esophageal stent, EndoVAC therapy cannot be easily performed for cervical leaks, as EndoVAC therapy requires the use of a sponge on a tube which is redirected through the nose (26). These interventions can potentially explain the significantly greater odds of chest leaks requiring interventions while nullifying other differences in outcomes.
There were limitations to this study that were inherent to the use of the ACS-NSQIP database, and the variable collected in it. ACS-NSQIP does not track any morbidities or mortalities after 30 days, which does not allow for any long-term data to be followed. Additionally, the data is deidentified which does not allow for comparisons between surgeon and hospital volume. Also, ACS-NSQIP does not report the esophagectomy reconstruction substitute, preventing patients who had a colonic reconstruction substitute from being excluded from our analysis. Furthermore, the lack of leak severity data in the ACS-NSQIP database provides an additional limitation, as we cannot discern mild anastomotic leaks from severe anastomotic leaks. Another limitation that is included with the use of a national database is the underestimated errors in coding which can result in reporting bias. However, we elected to use ACS-NSQIP database because it is a large national database, derived from over 700 hospitals throughout the United States. This database is collected directly from patients’ charts, and it is risk-adjusted (to account for differences in risk factors between patients), and case-mix-adjusted (to account for difference between hospitals) (27). These qualities made ACS-NSQIP database particularly suitable to answer our questions regarding the preoperative characteristics and post-operative complications in patients undergoing esophagectomy who experience an anastomotic leak. In addition to the relatively large sample size, an adjusted statistical analysis was utilized to assess independent predictors of post-operative leak in esophagectomy patients.
Conclusions
Post-esophagectomy chest and neck leak are associated with higher mortality and significantly increased post-operative complications. Diabetes and operative time were independent predictors for both leaks while steroid use, hypertension and advanced disease stage predicted intrathoracic leak. Intrathoracic leaks were associated with greater odds of needing an intervention but, contrary to conventional wisdom, were not associated with higher morbidity or mortality.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-37/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-37/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-37/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-37/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Given the de-identified nature of the data, this study was deemed exempt by the institutional review board at Virginia Commonwealth University, and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- He H, Chen N, Hou Y, et al. Trends in the incidence and survival of patients with esophageal cancer: A SEER database analysis. Thorac Cancer 2020;11:1121-8. [Crossref] [PubMed]
- Patel N, Benipal B. Incidence of Esophageal Cancer in the United States from 2001-2015: A United States Cancer Statistics Analysis of 50 States. Cureus 2018;10:e3709. [Crossref] [PubMed]
- Rutegård M, Lagergren P, Rouvelas I, et al. Intrathoracic anastomotic leakage and mortality after esophageal cancer resection: a population-based study. Ann Surg Oncol 2012;19:99-103. [Crossref] [PubMed]
- Sabra MJ, Alwatari YA, Wolfe LG, et al. Ivor Lewis vs Mckeown esophagectomy: analysis of operative outcomes from the ACS NSQIP database. Gen Thorac Cardiovasc Surg 2020;68:370-9. [Crossref] [PubMed]
- Barreto JC, Posner MC. Transhiatal versus transthoracic esophagectomy for esophageal cancer. World J Gastroenterol 2010;16:3804-10. [Crossref] [PubMed]
- Bizekis C, Kent MS, Luketich JD, et al. Initial experience with minimally invasive Ivor Lewis esophagectomy. Ann Thorac Surg 2006;82:402-6; discussion 406-7. [Crossref] [PubMed]
- Merritt RE. Initial experience of total thoracoscopic and laparoscopic Ivor Lewis esophagectomy. J Laparoendosc Adv Surg Tech A 2012;22:214-9. [Crossref] [PubMed]
- Takahashi C, Shridhar R, Huston J, et al. Esophagectomy from then to now. J Gastrointest Oncol 2018;9:903-9. [Crossref] [PubMed]
- Manghelli JL, Ceppa DP, Greenberg JW, et al. Management of anastomotic leaks following esophagectomy: when to intervene? J Thorac Dis 2019;11:131-7. [Crossref] [PubMed]
- Turkyilmaz A, Eroglu A, Aydin Y, et al. The management of esophagogastric anastomotic leak after esophagectomy for esophageal carcinoma. Dis Esophagus 2009;22:119-26. [Crossref] [PubMed]
- Lam TC, Fok M, Cheng SW, et al. Anastomotic complications after esophagectomy for cancer. A comparison of neck and chest anastomoses. J Thorac Cardiovasc Surg 1992;104:395-400. [Crossref] [PubMed]
- Walther B, Johansson J, Johnsson F, et al. Cervical or thoracic anastomosis after esophageal resection and gastric tube reconstruction: a prospective randomized trial comparing sutured neck anastomosis with stapled intrathoracic anastomosis. Ann Surg 2003;238:803-14. [Crossref] [PubMed]
- Gockel I, Exner C, Junginger T. Morbidity and mortality after esophagectomy for esophageal carcinoma: a risk analysis. World J Surg Oncol 2005;3:37. [Crossref] [PubMed]
- Famiglietti A, Lazar JF, Henderson H, et al. Management of anastomotic leaks after esophagectomy and gastric pull-up. J Thorac Dis 2020;12:1022-30. [Crossref] [PubMed]
- Markar SR, Arya S, Karthikesalingam A, et al. Technical factors that affect anastomotic integrity following esophagectomy: systematic review and meta-analysis. Ann Surg Oncol 2013;20:4274-81. [Crossref] [PubMed]
- Fabbi M, Hagens ERC, van Berge Henegouwen MI, et al. Anastomotic leakage after esophagectomy for esophageal cancer: definitions, diagnostics, and treatment. Dis Esophagus 2021;34:doaa039. [PubMed]
- Ubels S, Verstegen M, Bouwense S, et al. Commentary: endoscopic vacuum therapy for anastomotic leakage after esophagectomy and total gastrectomy: obstacles to finding true evidence. Dis Esophagus 2021;34:doab023. [Crossref] [PubMed]
- Phillips B. Reducing gastrointestinal anastomotic leak rates: review of challenges and solutions. Open Access Surg 2016;9:5-14. [Crossref]
- Fawcett A, Shembekar M, Church JS, et al. Smoking, hypertension, and colonic anastomotic healing; a combined clinical and histopathological study. Gut 1996;38:714-8. [Crossref] [PubMed]
- Post IL, Verheijen PM, Pronk A, et al. Intraoperative blood pressure changes as a risk factor for anastomotic leakage in colorectal surgery. Int J Colorectal Dis 2012;27:765-72. [Crossref] [PubMed]
- Zhang R, Zhang L. Feasibility of complete nasogastric tube omission in esophagectomy patients. J Thorac Dis 2019;11:S819-23. [Crossref] [PubMed]
- Paoli CJ, Reynolds MA, Sinha M, et al. Epidemiology and Costs of Sepsis in the United States-An Analysis Based on Timing of Diagnosis and Severity Level. Crit Care Med 2018;46:1889-97. [Crossref] [PubMed]
- Giuliano KK, Baker D, Quinn B. The epidemiology of nonventilator hospital-acquired pneumonia in the United States. Am J Infect Control 2018;46:322-7. [Crossref] [PubMed]
- Kauer WK, Stein HJ, Dittler HJ, et al. Stent implantation as a treatment option in patients with thoracic anastomotic leaks after esophagectomy. Surg Endosc 2008;22:50-3. [Crossref] [PubMed]
- Speer E, Dunst CM, Shada A, et al. Covered stents in cervical anastomoses following esophagectomy. Surg Endosc 2016;30:3297-303. [Crossref] [PubMed]
- Möschler O, Nies C, Mueller MK. Endoscopic vacuum therapy for esophageal perforations and leakages. Endosc Int Open 2015;3:E554-8. [Crossref] [PubMed]
- ACS NSQIP. 2018 PUF User Guide. 2019. Available online: https://www.facs.org/media/xunbqzy5/nsqip_puf_userguide_2018.pdf


