Thoracic surgery in India: challenges and opportunities
Introduction
The field of cardiothoracic and vascular surgery encompasses three major disciplines—cardiac, general thoracic and vascular surgery. In the early stages of evolution, these three fields were practiced by the same individuals. This is the case even now in several practice settings all over the world. However, maturity in the development of each discipline led to sub-specialization and specific training programs, clinical product lines and academic departments, not necessarily in that order. The last 50 years have seen that happen, particularly to general thoracic surgery, in North America and Europe. This sub-specialization has led to focused research and clinical innovation which in turn has led to significant improvement in patient outcomes.
Cardiothoracic surgery departments in India started out in a similar fashion, but over the last three decades have become cardiac surgery departments with little emphasis on and clinical activity in general thoracic surgery. In contradiction to this trend, the burden of thoracic diseases has continued to increase. This article documents the need for the emergence of general thoracic surgery in India as a distinct surgical specialty and the challenges and the opportunities for such an evolution.
Disease burden
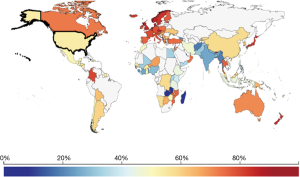
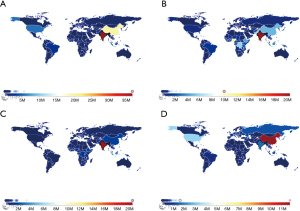
Rigorous statistics for disease burden in India are lacking due to widespread underreporting. However, with these limitations, some illustrative numbers can be obtained from the Global Burden of Diseases Study 2013 (http://www.healthdata.org). Figure 1 depicts a summary of the most common respiratory diseases encountered world-wide and their impact on society measured as disability adjusted life years (DALY). Compared to the rest of the world, India has a high burden of non-cancer lung pathology (1). This includes chronic respiratory illnesses such as COPD, asbestosis, pneumoconiosis and other debilitating illnesses. In addition, pulmonary diseases that were a thing of the past in the western world such as tuberculosis are still rampant in India. The social and economic impact of such a disease is amplified by the fact that, unlike cancer, tuberculosis affects young people in the prime of their productive life. It is the abundance of this non-cancer pathology that places India at the top of global lung disease burden. The incidence of lung cancer in India is relatively low. This may in part be due to the decreased longevity of the average Indian compared to the West. However, the median age of incidence of lung cancer in India is 56 years, which is significantly lower than in the USA, increasing the impact of this disease on the nation’s productivity (2).
Challenges, opportunities and potential solutions
Manpower
For a country as populous as India, manpower shortage in the medical field is rampant. The actual shortage is unquantifiable as accurate statistics are lacking. However, based on personal experience of the author, it is extremely difficult for a patient with a lung problem to access the services of a dedicated thoracic surgeon in what would be considered reasonable travel distance. Existing thoracic surgeons come from a variety of backgrounds, the most common being the rare cardiac surgeon who, by necessity has to take care of patients with general thoracic problems, or the surgical oncologist that has developed expertise in thoracic surgical oncology and occasionally strays into the world of benign problems to consider a challenging thoracic case. The number of cardiothoracic surgeons available is inadequate to service the needs for cardiac surgery, let alone that of general thoracic surgery. Therefore, emphasis needs to be placed on increasing the number of trainees and finding means to attract the best talent to this important clinical area. This issue is discussed later in this manuscript.
A second, often neglected issue is the availability or lack thereof of qualified allied health workers. Thoracic surgery is not practiced in a vacuum. Good thoracic surgery involves the active participation of well-trained nursing staff, respiratory therapists, physical therapists and biomedical engineers. Generally, these allied medical staff are poorly trained and poorly compensated. A tremendous opportunity to increase both the qualification and performance of allied health workers exists. Increased compensation and inclusion of these individuals as valued members of the surgical team has a huge potential to increase their ability and productivity.
Affordability
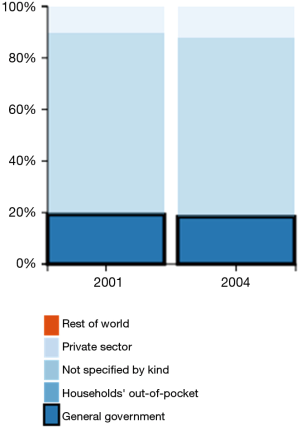
Affordable health care is a problem in India as a whole. India spends an abysmally low 2–4% of its GDP on health care (compared to an average of 10.2% average for most other countries). In addition, most of the health care expenses are borne by individual savings. Only about 20% of the country’s health care is spent by the government (1), in distinction to the western world (Figures 2,3). While there has been anguish expressed in the media about the patient’s plight in these circumstances, an important point to stress is the physician’s plight of attempting to provide a modicum of decent care with these financial limitations. Over the last decade, there has been a proliferation of public health schemes that provide a fixed reimbursement to hospitals for the care of the indigent with specific health care issues. In most instances, the reimbursement for a lobectomy for a hospital under these schemes is ~USD 750. This includes the hospital admission, professional fees and all consumables used during the admission, including the cost of any complications arising from the surgery. It is impossible to conduct a modern lobectomy, even if performed open without any expensive and sophisticated minimally invasive equipment, in this financial scope. This is particularly true for the conduct of surgery for TB which is more complex and fraught with more intra-operative and post-operative problems than surgery for cancer. If a surgeon chooses to perform a surgery in these circumstances following which a post-operative complication occurs, the surgeon is left in the ethical dilemma of discontinuing further care capable of salvaging the patient vs. the ire of hospital authorities unwilling to accept a financial loss for the case. Therefore, it is understandable when a conscientious physician chooses not to take on any but the most straightforward thoracic surgical cases.
This problem is less acute with patients in a higher social bracket. Even in this population, patients are cost-conscious. It is not uncommon for patients to choose open surgery over VATS due to lower operative costs. While many cost comparisons in the west demonstrate the cost savings of VATS over open surgery (3), the differing cost structures in the two health systems lead to different outcomes. The daily costs of a hospital bed in India is much lower, even in relative terms, than in the west and therefore, the reduced length of stay by a couple of days does not offset the increased cost of equipment and endo-staplers required for an anatomic resection. The cost problem is further accentuated by the use of the robot which, while remaining an exciting development, has unproven advantages over VATS (4).
These restrictions on cost, however, have opportunities for innovation with world-wide applicability. Indeed, such a brand of innovation has engendered a specific name—‘Jugaad’. This is a colloquial Hindi work that means a simple fix or an innovation to get around a problem. Surgeons have overcome some obstacles in thoracic surgery with using staplers for specific vessels, modifying operative techniques to minimize stapler use, reusing disposable instruments after sterilization and the development of low cost instruments. In fact, the opportunities for companies to develop low cost staplers or reusable staplers, and energy devices capable of vessel sealing obviating the use of some staplers, to tap the country’s thoracic surgery market are enormous. These advances can help other countries reduce their cost of thoracic surgery as well.
Training opportunities
Unfortunately, students graduating from general surgery programs have increasingly chosen other career options and an increasing proportion of cardiothoracic residency positions have gone unfilled in the last few years. Barriers to popularity of CT surgical training include the length of training, the absence of training paradigms that incorporate progressive operative responsibility, the extremely hierarchical nature of most practice positions with inequitable distribution of income generated by group practices, and the reduced remuneration per case secondary to proliferation of public health schemes. Specifically looking at training programs targeted at the development of general thoracic surgery positions, only three such training programs exist in the country, graduating a total of six trainees a year. These training programs are de-linked from cardiac surgery training for the most part and have been in existence for only approximately three years. A significant exception is the surgical oncology training program at the Tata Memorial Cancer Center which provides a concentrated experience in thoracic oncology work. However, the existence of a single program highlights the problem, not even taking into consideration that this program does not provide any experience with management of benign thoracic conditions.
Therefore, a significant opportunity exists to increase the thoracic surgical workforce in the country. Increasingly, there has developed a perception that thoracic surgery is viable from a financial viewpoint for the hospital as well as the practitioner. In addition the visibility and excitement around minimally invasive approaches such as video-assisted thoracic surgery (VATS) and robotic surgery has a greater chance of attracting young talent to the field. Hopefully, existing cardiothoracic surgery departments will identify individuals interested in general thoracic surgery and reclaim the field.
Another limitation in training is the absence of continuing education requirements for licensing or for periodic board certifications. Combined with a general lack of access to the latest medical publications, this decreases the impetus of the practicing surgeon to familiarize himself with current treatment paradigms and pathways to improve care. The increasing availability of the internet and open access publishing should hopefully ameliorate this problem.
Social issues
A major barrier to seeking quality care is the social stigma attached to both tuberculosis as well as cancer. Most patients and family members are reticent in discussion of and seeking help with both these conditions. Very often, families request the physician to not disclose the diagnosis to the patients themselves. Therefore, a lot can be done to increase awareness of the treatability of these conditions in India.
In terms of liability, the medical field in India has, by and far, not become litigious. Liability insurance is affordable and does not pose a financial burden on doctors. However, whether this lack of readily available legal recourse limits physician accountability is debatable.
Hospital systems
Hospital systems in India are far behind the times. Although greatly improved from just a couple of decades ago, there is a long way to go. Electronic medical records are gaining ground only very slowly and most medical records are hand written. Digital imaging, though, has become extremely popular and easily available. The absence of a rapid response system (such as ‘911’ in the United States) limits the outcome of true surgical emergencies and thoracic trauma. Real tumor boards with equivocal participation by all relevant specialists are rare outside academic environments. Particularly for lung cancer, comprehensive staging is lacking. However, adoption of established paradigms existing outside the country should go a long way to improving these system-based issues.
Conclusions
The amount of surgically treatable lung cancer pathology in India is large, with the vast proportion of patients not having access to dedicated general thoracic surgeons. Despite all the limitations outlined in this manuscript, the needs of the populace provide a huge opportunity for the rapid increase and maturation of this surgical specialty in India. These limitations also provide an environment that mandates innovation to meet the unique challenges of this vulnerable population.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Institute for Health Metrics and Evaluation (IHME). Seattle, WA: IHME, University of Washington, 2015. Available online: http://www.healthdata.org/
- Noronha V, Dikshit R, Raut N, et al. Epidemiology of lung cancer in India: focus on the differences between non-smokers and smokers: a single-centre experience. Indian J Cancer 2012;49:74-81. [Crossref] [PubMed]
- Farjah F, Backhus LM, Varghese TK, et al. Ninety-day costs of video-assisted thoracic surgery versus open lobectomy for lung cancer. Ann Thorac Surg 2014;98:191-6. [Crossref] [PubMed]
- Nakamura H. Systematic review of published studies on safety and efficacy of thoracoscopic and robot-assisted lobectomy for lung cancer. Ann Thorac Cardiovasc Surg 2014;20:93-8. [Crossref] [PubMed]