
Modification of the Abramson procedure for minimally invasive repair of pectus carinatum: introduction of a pectus carinatum compression system
Highlight box
Surgical highlights
• The modified surgical technique involves the use of the PectusAssist™ System, a table-mounted compression system that eliminates the need for manual pressure on the chest wall during the Abramson procedure. This ensures accuracy in determining the desired bar length and curvature, simplifies the presternal tunnel creation, and reduces labor intensity for the surgical team.
What is conventional and what is novel/modified?
• The most challenging part of the Abramson procedure is creating the presternal tunnel, which may cause complications if the thoracic cavity is penetrated. The PectusAssist™ System simplifies tunnel creation by ensuring consistent compression of the chest wall.
What is the implication, and what should change now?
• We recommend standard use of the PectusAssist™ System in the Abramson procedure for minimally invasive repair of pectus carinatum. The system enables an easy and more predictable placement of the presternal metal bar.
Introduction
Background
Pectus carinatum, commonly referred to as pigeon chest, is characterized by prominence of the anterior chest wall caused by protrusion of the sternum (1,2). Its prevalence is estimated at 1 per 1,500 live births in North America, but occurs mostly during adolescence. Twenty-five percent of patients have a positive family history of anterior chest wall deformities (1,3).
Treatment of pectus carinatum consists of both non-surgical (e.g., orthotic braces, physical therapy) and surgical options (4-7). The latter include the classic open Ravitch procedure (5) and the more recently introduced minimally invasive Abramson procedure (6-8).
Minimally invasive repair of pectus carinatum (MIRPC) by the Abramson procedure, sometimes also referred to as the ‘reversed Nuss technique’, was first described in 2005 by Abramson et al. (7). During this procedure, a presternal, subpectoral metal correctional bar, secured to rib-attached stabilizers, is implanted to bring the sternum back to a more natural position (6,7). This minimally invasive technique has several advantages over the open Ravitch procedure as it preserves the present rib cartilages whilst only remodeling the sternum, as such avoiding fibrothorax during regrowth of the resected cartilage, as well as minimizing blood loss in contrast to wide dissection area and the large operative field during the Ravitch procedure. Consequently, the MIRPC is associated with less postoperative pain, a shorter hospitalization period, and better cosmetic results (6,8-12) as scars are situated laterally rather than in the frontal aspect of the chest.
Rationale
Numerous steps of this procedure, such as modeling of the bar to the targeted patient’s chest contour, and insertion and definitive positioning of the bar, involve the application of manual compression over the sternum to reduce the deformity in view of the estimation of the intended position of the sternum. In order to ease the procedure and reduce variability we identified the need for the introduction of a temporary reduction device of the sternum. After thoughtful consideration, we introduced the PectusAssist™ System (Thompson Surgical Instruments, Traverse City, Michigan, USA) (13). This instrument is installed on a table-mounted system and generates a constant mechanical compression over the protruding sternum to maintain its intended neutral position during surgery.
Objective
This device was first introduced in Europe at the University Hospitals Leuven, Belgium. Given the easiness of use of this system, we also introduced it in another large chest wall unit which also embarked on the Abramson procedure, where until then sternal reposition was only achieved by manual compression. In this manuscript, we describe the implementation of this novel aid during the Abramson procedure in these two high-volume chest wall centers. We present this article in accordance with the SUPER reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-642/rc).
Preoperative preparations and requirements
The procedure starts as described in detail by Abramson et al. (6-8). Prior to surgery, an epidural catheter is inserted at T4-T5 level. The procedure is performed under general anesthesia with double lung ventilation. Antibiotic prophylaxis is achieved by administration of cefazoline. After induction, the patient is positioned in the supine position with both arms abducted on armrests. Perioperative photographs and a video are published with the patient’s written informed consent.
Step-by-step description
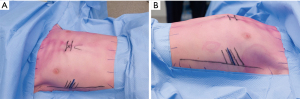
Skin markings are made as follows (Figure 1): (I) point of greatest sternal protrusion; (II) transverse line through the point of greatest protrusion, indicating the future bar position whilst applying manual compression; (III) selected ribs for placement of pericostal attached stabilizers.
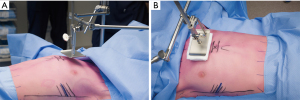
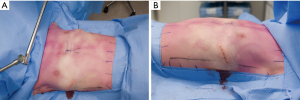
After prepping and draping of the surgical field, the PectusAssist™ System is installed on a table-mounted Thompson system consisting of two table-mounted posts and a transverse rod (Thompson Surgical Instruments, Traverse City, Michigan, USA) and positioned 2–3 cm cranially to the point of greatest sternal protrusion (Figure 2); placement of the PectusAssist™ System directly over the point of greatest protrusion would otherwise hinder the creation of the presternal tunnel later during the procedure. A sterile gauze or soft sterile cloth is placed between the PectusAssist™ System and the skin to avoid direct contact with the metal compression plate as to prevent pressure ulcers. The PectusAssist™ System is equipped with a ratcheting pulley, for the purpose of this intervention pointed towards the patient as to deliver compression. By advancing the PectusAssist™ System downwards, the pressure on the chest wall is gradually increased until a neutral position of the sternum is obtained. The surgery is then continued as originally described by Abramson et al. (6-8), using the Universal Pectus System (MedXpert, Eschbach, Germany). Appropriate bar size and curvature are determined using a template, taking into account the length between both midaxillary lines. Actual bending of the bar into its desired configuration is performed using a hand bender as to provide a contour that adheres as best as possible to the newly obtained external form of the entire anterior chest wall (Figure 3).

Bilateral transverse skin incisions of about 3 cm in length are made over the intercostal spaces between the selected ribs from the midaxillary line towards the anterior aspect of the chest. In female patients, the skin incisions are preferably made in the inframammary fold, admittedly making the reach of the target ribs a bit more difficult as they are for these aesthetical reasons to be approached from a more medial aspect than intended initially. After diathermic dissection of the subcutaneous tissue, the underlying serratus anterior muscle is split, revealing the anterolateral chest wall. Now the definitive alignment and position of the bar and stabilizers are reassessed in vivo, determining the definitive cranial and caudal rib fixation points for the stabilizers. The periosteum of the selected ribs is consecutively opened by diathermia perpendicular to the course of the rib. A raspatory is used to create a narrow circumferential subperiosteal tunnel around the selected ribs (Figure 4). The inferior-posterior part of the subperiosteal tunnel is created with great caution to avoid damage to the underlying parietal pleura and intercostal neurovascular bundle. We prefer to create the subperiosteal and subpleural pericostal tunnels during apnea combined with ventilator disconnection, to minimize the risk of injury to eventual expanding lung parenchyma during this maneuver. Then the rib is encircled with a blunt-tipped bone hook (Figure 5A) via which a small caliber silicon catheter is drawn through the subperiosteal tunnel. Subsequently, the catheter is used as a guide for the safe placement of pericostal steel wires of 1.1 mm diameter (Pioneer Surgical Technology Inc., Marquette, MI, USA). These sutures seem to be rigid enough for temporary semi-rigid fixation onto the lateral chest wall. These will partly lose their function once natural fixation between the chest wall and the stabilizers has taken place after healing and inflammation reactions in the pocket have subsided (Figure 5B).

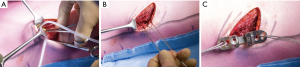
Following steel wire placement, the stabilizers are parachuted into the submuscular pocket (Figure 5C). None of the stabilizers is tied down to the lateral chest wall at this stage, as this would impede the insertion of the bar into the stabilizers as well as orientation of the stabilizers towards the bar.
First blunt finger dissection and subsequent long atraumatic soft tissue clamps like an aortic vascular clamp are used to create a bilateral retromuscular tunnel behind the serratus anterior and pectoralis major from each side of the thorax connecting the two lateral submuscular pockets. The tunnel passes medially close to the sternal attachments of the pectoralis major. This is a technically difficult part of the procedure as the two tunnels need to be connected at the level of the sternum where the amount of subcutaneous tissue is limited, for which also the lateral fascia of the pectoralis muscle needs to be perforated. Care must be taken to avoid skin perforation in the presternal area, as well as not to enter the chest with the bent tip of the blunt soft tissue clamps. The use of the continuous, temporary but rigid reduction device at the level of the anterior chest wall helps in this other essential step as to prevent these deleterious technical complications, opposed to the otherwise varying compression levels in force as in time of repetitive manual compression performed by the assistant surgeons.
A trapezium-like bent introducer is then inserted in the retromuscular tunnel under guidance of the soft tissue clamps and advanced from the right to the left submuscular pocket. Once the tip of the pectus introducer is visualized, a 28Fr chest tube is placed over the tip. Next, the introducer is pulled back in the tunnel from left to right (Figure 6A) as to provide a guide for later bar insertion. Then the introducer is removed from the chest tube and subsequently, the tip of the metal correctional bar is pushed into to the left open end of the tube and transfixated with a thread. The Abramson bar is now advanced in the tunnel by use of the chest tube as a guide, with the convexity of the bar initially caudally, with automatic orientation of the bar when gliding into the tunnel position, facing posteriorly in the end (Figure 6B).
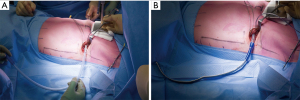
Both ends of the bar are placed into the stabilizers and temporarily locked with the screw (Figure 7A). The steel wires can now be manually tightened down as not to overpower the cable threads, securing the stabilizer-bar complex onto the lateral chest wall (Figure 7B,7C) and thus providing fixation of the system onto the ribs.

Now the pectus compression device can be released, showing an already large reduction of the initial present pectus carinatum. The final correction can now be carried out by bilateral adjustment of the definitive position of both bar ends in their respective stabilizers, this time by final manual compression of the chest, as to achieve an as good as possible adherence of the bar contours to the chest wall favoring a symmetric reduction and minimize postoperative visualization of the subcutaneously positioned bar. Hereafter, the bar is locked into the stabilizers by tightening the screws for permanent fixation. At this point, final correction of the deformity and stable fixation of the implant has been reached. In principle, the minimally invasive Abramson procedure is performed with the use of one bar. Finally, the PectusAssist™ System is dismantled, and the wounds are closed in layers (Figure 8).
Postoperative considerations and tasks
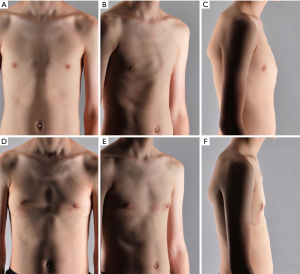
A plain chest radiograph is routinely acquired just before anesthetic lead-out or at the post-anesthesia recovery unit. Thoracic epidural analgesia is ceased and transitioned to oral pain medication per protocol on the second or third postoperative day. Postoperative physical therapy is started on the first postoperative day. Patients are discharged from the hospital after achievement of adequate pain control and sufficient mobilization. Standard length of hospital stay in our centers is 4 days. All patients enter a two-year follow-up program with outpatient clinic follow-up appointments every three months. Conventional photographs and three-dimensional images are obtained during follow-up for evaluation of the aesthetic outcome. The Abramson bar is removed after a mean in-situ period of two years.
As an example, Figure 9 displays the preoperative and postoperative photographs of a patient treated at our institutions with the use of the PectusAssist™ System, demonstrating an adequate correction.
Tips and pearls
Video 1 demonstrates the step of the procedure in which the PectusAssist™ System is advanced downwards until the sternum is redressed to its neutral position. Given the innate large anteroposterior distance of the chest, we have up to now never seen any cardiac impact whilst performing this maneuver as the chest wall remodels towards the lateral parts of the chest wall.
Discussion
Surgical highlights
Surgical correction of pectus carinatum is considered the next step in the treatment algorithm for patients who are not suitable for conservative treatment or when bracing therapy fails. Adequate patient selection is therefore crucial, as incorrect usage of orthotic treatment can delay the need for surgery and increase the overall costs of treatment. Factors such as asymmetric deformations, increased age which is associated with increased chest wall rigidity, as well as poor treatment compliance are linked to high failure rates of orthotic treatment. Furthermore, recurrence is more commonly reported in younger patients before the end of their growth spurt.
The deformity can be surgically corrected by the open, modified Ravitch procedure, or the minimally invasive Abramson procedure. Nowadays, the Abramson procedure has gained worldwide acceptance as it is superior to the open Ravitch procedure for surgical correction of pectus carinatum in terms of postoperative pain, hospitalization period, and cosmetic results (9). Therefore, the Ravitch procedure is primarily reserved for the correction of rigid or extremely severe and asymmetric deformities. The ideal age range for surgical repair by the Abramson method is during puberty, between 12 and 18 years of age, corresponding to a phase of rapid growth when the chest wall has relatively high flexibility, reducing the forces encountered during the procedure.
In the present manuscript, we describe a safe and easy-to-use modification of the original Abramson procedure for minimally invasive correction of pectus carinatum by implementing a temporary rigid compression of the anterior chest wall, facilitating optimal bending as well as safe placement of the bar.
Strengths and limitations
The introduction of the table-mounted PectusAssist™ System most importantly eliminates the necessity of applying manual repetitive, usually incoherent, and thus varying pressure on the deformity and maintains a more stable sternal position whilst creating the submuscular tunnel.
This will ensure accuracy of the template used to determine the desired bar length and curvature. Also, use of the PectusAssist™ System makes the procedure less labor intensive, especially for the assistant-surgeons. In our experience, the PectusAssist™ System does not cause skin damage related to the temporarily applied pressure.
Comparison with other surgical techniques and researches
Creation of the presternal tunnel during the Abramson procedure is considered to be the technically most challenging part (6-8) with still some chance to penetrate the thoracic cavity when trying to follow the protruded contour of the chest wall. Özkaya et al. (14) proposed a minor modification in which they use Doyen bowel clamps for its creation. Moreover, they use the Doyen bowel clamp to grasp the metal bar and move the bar along the tunnel, eliminating the necessity to use the introducer and attached chest tube drain to guide the metal bar. In our experience, the position of the hinge close to the handle and the narrowness of the submuscular tunnel might limit sufficient opening of the jaws and as such make grasping of the bar at the opposite end of the tunnel difficult. Therefore, we use the aortic clamps for tunnel creation, followed by the insertion of a specifically designed tunnel device.
The modification we propose also simplifies this part of the procedure as the two retromuscular tunnels, that need to be connected presternally, are better aligned throughout the procedure due to a more stable position of the sternum with the PectusAssist™ System.
Park’s Flare Compressor device (Primemed, Seoul, South Korea), as inspired by Park, is a comparable, double-post table-mounted instrument that can be used to apply external mechanical compression to the anterior chest wall (15). Instead of a decentralized table-mounted position as with our proposed system, PectusAssist™ System, these posts are centered at the level of the sternal zone to be compressed and can as such be in the way during dissection and tunnel creation. Use of Park’s Flare Compressor has been described for the sandwich technique to correct pectus carinatum with an accompanying pectus excavatum, a so-called pectus concavo-convexus combining intrathoracic and extrathoracic bar placement (15).
The Rultract retractor (Rultract Inc., Cleveland, Ohio, USA), often used in the USA during cardiothoracic surgical procedures, is only intended for lifting of the sternum, and as such cannot provide a consistent compression of the protruded anterior chest wall.
Implications and actions recommended
Many hospitals already have the basic compounds of the Thompson Retractor system available for use within open heart surgery, various types of visceral surgery, open thoracic surgery, orthopedic and neurosurgery, with at least one or two table posts and an interconnecting rod on shelf. Unlike most other non-European designed devices, the Thompson retractor is certified for use within the EU which makes the transition for use within chest wall surgery only a small step, legally and financially. Application of the PectusAssist™ System in the Abramson procedure requires a one-time investment in the purchase of the PectusAssist™ System. Larger tertiary pectus referral centers already use the Thompson retractor add-on in the crane technique during MIRPC (16,17), thus eliminating the additional costs as the compressor plate is oppositely mounted to the crane hook (13).
Unlike for the Nuss procedure (18), there is currently no literature available on the learning curve of the Abramson procedure. Furthermore, a threshold for an optimal caseload based on complication rates has also not been established yet and requires further research in order to determine whether the Abramson procedure should be centralized.
Conclusions
The use of the PectusAssist™ System enables an easy and more predictable placement of the presternal metal bar during the Abramson procedure for pectus carinatum, as variation due to manual compression is reduced thanks to this table-mounted compression system. Moreover, labor intensity is minimized, without interfering with the safety of the procedure. We, therefore, suggest standard use of the PectusAssist™ System during MIRPC by the Abramson procedure.
Acknowledgments
The authors gratefully acknowledge Ernst van Loon, Medical Photographer (Zuyderland Medical Centre, Heerlen, The Netherlands), for the acquisition of the video documentation of the procedure, as well as the acquisition of the perioperative photographs.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Thoracic Disease, for the series “Minimally Invasive Treatment of Pectus Deformities”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-642/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-642/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-642/coif). The series “Minimally Invasive Treatment of Pectus Deformities” was commissioned by the editorial office without any funding or sponsorship. HGLW is a consultant for Thompson Surgical Instruments. ERdL and JHTD served as unpaid Guest Editors of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All images are published with the patient’s consent. Written informed consent for publication of perioperative photographs and a video was obtained.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fonkalsrud EW, Dunn JC, Atkinson JB. Repair of pectus excavatum deformities: 30 years of experience with 375 patients. Ann Surg 2000;231:443-8. [Crossref] [PubMed]
- Goretsky MJ, Kelly RE Jr, Croitoru D, et al. Chest wall anomalies: pectus excavatum and pectus carinatum. Adolesc Med Clin 2004;15:455-71. [Crossref] [PubMed]
- Shamberger RC, Welch KJ. Surgical correction of pectus carinatum. J Pediatr Surg 1987;22:48-53. [Crossref] [PubMed]
- Frey AS, Garcia VF, Brown RL, et al. Nonoperative management of pectus carinatum. J Pediatr Surg 2006;41:40-5; discussion 40-5. [Crossref] [PubMed]
- Ravitch MM. Unusual sternal deformity with cardiac symptoms operative correction. J Thorac Surg 1952;23:138-44. [Crossref] [PubMed]
- Abramson H, D'Agostino J, Wuscovi S. A 5-year experience with a minimally invasive technique for pectus carinatum repair. J Pediatr Surg 2009;44:118-23; discussion 123-4. [Crossref] [PubMed]
- Abramson H. A Minimally Invasive Technique to Repair Pectus Carinatum. Preliminary Report. Archivos de Bronconeumología ((English Edition)) 2005;41:349-51.
- Abramson H, Aragone X, Blanco JB, et al. Minimally invasive repair of pectus carinatum and how to deal with complications. J Vis Surg 2016;2:64. [Crossref] [PubMed]
- Geraedts TCM, Daemen JHT, Vissers YLJ, et al. Minimally invasive repair of pectus carinatum by the Abramson method: A systematic review. J Pediatr Surg 2022;57:325-32. [Crossref] [PubMed]
- Yüksel M, Bostanci K, Evman S. Minimally invasive repair of pectus carinatum using a newly designed bar and stabilizer: a single-institution experience. Eur J Cardiothorac Surg 2011;40:339-42. [Crossref] [PubMed]
- Özkaya M, Bilgin M. Minimally invasive repair of pectus carinatum: a retrospective analysis based on a single surgeon's 10 years of experience. Gen Thorac Cardiovasc Surg 2018;66:653-7. [Crossref] [PubMed]
- Katrancioglu O, Akkas Y, Karadayi S, et al. Is the Abramson technique effective in pectus carinatum repair? Asian J Surg 2018;41:73-6. [Crossref] [PubMed]
- PectusAssist™ System. Available online: https://www.thompsonretractor.com/system/pectusassist-system/
- Özkaya M, Bilgin M. Minimally invasive repair of pectus carinatum by modification of the Abramson technique. Wideochir Inne Tech Maloinwazyjne 2018;13:383-7. [Crossref] [PubMed]
- Park HJ, Kim KS. The sandwich technique for repair of pectus carinatum and excavatum/carinatum complex. Ann Cardiothorac Surg 2016;5:434-9. [Crossref] [PubMed]
- Haecker FM, Krebs T, Kocher GJ, et al. Sternal elevation techniques during the minimally invasive repair of pectus excavatum. Interact Cardiovasc Thorac Surg 2019;29:497-502. [Crossref] [PubMed]
- de Loos ER, Daemen JHT, Coorens NA, et al. Sternal elevation by the crane technique during pectus excavatum repair: A quantitative analysis. JTCVS Tech 2021;9:167-75. [Crossref] [PubMed]
- de Loos ER, Daemen JHT, Pennings AJ, et al. Minimally invasive repair of pectus excavatum by the Nuss procedure: The learning curve. J Thorac Cardiovasc Surg 2022;163:828-837.e4. [Crossref] [PubMed]


