
Total arch replacement versus hybrid operation for aortic arch aneurysm in elderly patients: a retrospective cohort analysis
Highlight box
Key findings
• In treating aortic arch aneurysms of elderly patients, the risk of re-intervention was significantly higher in the hybrid group than in total arch replacement.
What is known and what is new?
• The hybrid procedure is known as more safety option than total arch replacement in elderly aortic aneurysm patients.
• There was no definitive evidence of the superiority of hybrid procedures over total arch replacement, although the risk of re-intervention was higher in the former group.
What is the implication, and what should change now?
• The surgical strategy for aortic arch aneurysms should be selected based on the patient’s demographic and anatomical characteristics.
Introduction
Advanced age is a significant risk factor during repair of the aortic arch following an aneurysm. Milewski et al. (1) reported the hybrid arch approach has lower mortality for high-risk patients aged more than 75 years, and the relative safety of hybrid arch procedures involving aortic arch debranching and endovascular graft placement have made them increasingly popular in the elderly population (1,2). However, there is limited evidence on the efficacy of the hybrid arch procedure in comparison to total arch replacement (TAR) in elderly patients (3,4). The most critical differences between TAR and hybrid procedure are that aortic stents and aneurysmal changed aortic tissue were left in the hybrid procedure. Therefore, the primary purpose of this article is to compare short and mid-term operation results between TAR and hybrid procedure for analyzing the effects of aortic stents and remnant aneurysmal changed tissue in elderly patients (≥75 years of age) diagnosed with aortic arch aneurysms and underwent aortic arch repair in two medical centers. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-331/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of the Samsung Medical Center approved the study (No. 2021-08-045-001, August 30, 2021). Individual consent was waived due to the retrospective nature of this study. This retrospective study included 922 patients who underwent aortic arch repair at two medical centers between January 2012 and May 2021 (Figure 1). Patients <75 years of age and those with a history of acute/chronic aortic dissection, hemiarch or partial arch aortic replacement, patients with aortic arch aneurysm extending below pulmonary artery bifurcation level, or connective tissue disease were excluded. Additionally, patients who had undergone aortic arch repair via left thoracotomy were also excluded.
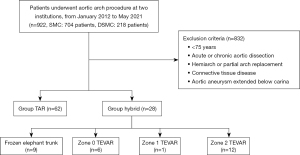
We excluded patients with aortic arch aneurysms extending below pulmonary artery bifurcation because this type of aortic aneurysm is closer to descending aortic aneurysm than aortic arch aneurysm, especially in the zone 2 thoracic endovascular aortic repair (TEVAR) cohort.
Variables and outcome
Preoperative status and intraoperative information were abstracted retrospectively from the hospital medical records each patient as described in Table 1. Patients who underwent TAR with a frozen elephant trunk were assigned to the hybrid group than the TAR group because TAR with a frozen elephant trunk reduced the extent of resected aortic tissue and left an aortic stent with aneurysmal changed aortic tissue compared with TAR without frozen elephant trunk. Other hybrid procedures included zone 0, 1, and 2 TEVAR with or without arch vessel bypass surgery.
Table 1
| Characteristics | TAR (n=62) | Hybrid (n=28) | P value |
|---|---|---|---|
| Age, years, mean ± SD | 79.5±3.6 | 77.7±3.3 | 0.03 |
| Ejection fraction, %, mean ± SD | 64.1±7.2 | 63.7±6.3 | 0.79 |
| Sex, males, n (%) | 44 (71.0) | 21 (75.0) | 0.62 |
| Neurological dysfunction, n (%) | 8 (12.9) | 4 (14.3) | >0.99 |
| Diabetes, n (%) | 12 (19.4) | 8 (28.6) | 0.31 |
| Diabetes on insulin, n (%) | 2 (3.2) | 3 (10.7) | 0.17 |
| Ischemic heart disease, n (%) | 20 (32.3) | 9 (32.1) | 0.97 |
| Other heart disease, n (%) | 4 (6.5) | 0 | 0.31 |
| COPD, n (%) | 18 (29.0) | 3 (10.7) | 0.04 |
| Other lung disease, n (%) | 5 (8.1) | 2 (7.1) | >0.99 |
| Chronic kidney disease, n (%) | 20 (32.3) | 1 (3.6) | 0.002 |
| History of malignant disease, n (%) | 15 (24.2) | 4 (14.3) | 0.41 |
| Other vascular disease, n (%) | 14 (22.6) | 7 (25.0) | 0.77 |
| History of cardiac or aortic surgery, n (%) | 5 (8.1) | 2 (7.1) | >0.99 |
| Poor mobility, n (%) | 1 (1.6) | 0 | >0.99 |
| Carotid stenosis >50%, n (%) | 12 (19.4) | 7 (25.0) | 0.54 |
| Cerebral vascular stenosis, n (%) | 16 (25.8) | 8 (28.6) | 0.75 |
| Pulmonary hypertension, n (%) | 6 (9.7) | 2 (7.1) | >0.99 |
| Emergency operation, n (%) | 12 (19.4) | 3 (10.7) | 0.38 |
| NYHA class, n (%) | 0.20 | ||
| 0 | 55 (88.7) | 25 (89.3) | |
| I | 3 (4.8) | 3 (10.7) | |
| II | 4 (6.5) | 0 |
TAR, total arch replacement; COPD, chronic obstructive pulmonary disease; NYHA class, New York heart association class.
The primary outcome measures were all-cause mortality and incidence of post-surgical re-intervention in a previously repaired arch segment. Permanent and temporary neurological deficits were defined as new deficits that were either present or had undergone complete resolution at the time of discharge, respectively. Medical records and the hospital database were used to collect patient demographics and baseline and follow-up clinical (such as vital status) data, while mortality data was collected from the National Registry of Births and Deaths using the patients’ unique personal identification numbers. The mean duration of follow-up was 27.0±28.8 months.
Surgical indications
Open surgical repair was the first treatment of choice for patients diagnosed with aortic arch aneurysms in both medical centers, with the hybrid arch procedure being considered for high-risk elderly patients (≥75 years of age) with multiple comorbidities only. The multidisciplinary team developed the final treatment plan based on the anatomical characteristics of the aorta [such as the proximal and distal landing zone, site of side clamping or aortic cross-clamping (ACC) in the ascending aorta, and degree of calcification/presence of thrombus in the aortic lumen], carotid artery, and cerebral arteries.
Surgical technique for total arch replacement
All patients underwent median sternotomy and cardiopulmonary bypass (CPB), established using bicaval drainage and arterial return through the ascending aorta or axillary artery. The position of the arterial cannulation was determined using computed tomography and epiaortic ultrasound examination to minimize the risk of cerebral embolism. The patients’ body temperature was lowered until a rectal temperature of 24–28 ℃ was achieved, and the adequacy of the cardiopulmonary bypass perfusion was monitored using two arterial lines (right radial and femoral arteries), cerebral oximetry, and urine output. After opening the ascending aorta and aortic arch, balloon-tipped selective cerebral perfusion (SCP) cannulas were inserted into the three supra-aortic vessels and TAR was performed using a 4-branched graft. Following distal anastomosis, antegrade systemic circulation was resumed through a side branch of the graft, and the three arch vessels were then reconstructed individually using the branch of the arch graft extending from the left subclavian artery (LSA) to the brachiocephalic artery (BCA). Proximal anastomosis was performed above the sinotubular junction, and the ACC clamp was then removed and the patient’s body temperature was brought back to normal.
Surgical technique for hybrid procedure
In the hybrid procedure, the types of TEVAR were selected by the level of the proximal end of the aneurysm. Therefore, the most critical selection criteria for TEVAR type was sufficient landing zone, ranging from 15–25 mm proximally and 20–30 mm distally. In addition, and in a specific situation, the angle of patients’ aorta or combined thromboembolism risk was also considered. We generally select the diameter of the stent graft to be about 120% of the aortic aneurysm diameter. After TEVAR, additional ballooning or stent graft insertion is performed if there is an endoleak in post-TEVAR angiography.
TAR with frozen elephant trunk
The cannulation and CPB strategy used were similar to that of TAR reported above. Following ascending aorta and aortic arch resection, balloon-tipped SCP cannulas were inserted into the three supra-aortic vessels and the aortic arch was prepared for distal sutured anastomosis. The stent graft was then inserted into the proximal descending aorta in an antegrade direction and deployed such that it covered the dilated vessel. Distal anastomosis was carried out using a 4-branched expanded polytetrafluoroethylene graft, and the remaining procedures were completed in a manner similar to TAR mentioned above.
Zone 0 thoracic endovascular repair
Following median sternotomy and side clamping of the ascending aorta, end-to-side anastomosis was carried out between the ascending aorta and the ePTFE graft. A bypass from the ascending aorta to the BCA, left common carotid artery (LCCA), and LSA was created, and a thoracic endovascular repair (TEVAR) stent graft was deployed through the femoral artery such that it covered the BCA, LCCA, and LSA.
Zone 1 TEVAR
A bypass from the right common carotid artery to the LCCA and LSA was created using a ringed Gore-Tex graft (8 mm), and the proximal sites of the LCCA and LSA were ligated. The TEVAR stent graft was deployed through the femoral artery such that it covered the LCCA and LSA.
Zone 2 TEVAR
In 7 patients, a bypass was created from the LCCA to the LSA using a ringed Gore-Tex graft (8 mm) and the TEVAR stent graft was deployed through the femoral artery such that it covered the LSA. In the remaining 5 patients, no LSA bypass was created and the TEVAR stent graft was deployed through the femoral artery such that it covered the LSA.
Statistical analysis
Normally distributed variables were reported as mean (range) values and compared using the independent t-test, while non-parametric continuous variables were reported as median (interquartile range) values and compared using the Mann-Whitney U test. Categorical variables were reported as numbers (percentages) and compared using the Pearson’s chi-square test. Cox proportional hazards regression was used to estimate the hazard ratio (HR) for risk factors for late mortality, and variables with a P<0.2 in the initial analysis were included in the multivariate regression model (5). The Kaplan-Meier method was used to construct survival and free-from-re-intervention curves, and these were compared using log-rank tests. All statistical analyses were performed using the SPSS software, version 20 (SPSS Inc., Chicago, IL, USA), and P<0.05 were considered statistically significant.
Results
The study sample included 62 and 28 patients in the TAR and hybrid groups and the mean follow-up duration was 27.0±28.8 and 38.8±35.4 months (P=0.10) in each group. The mean age of the patients was significantly higher in the former group compared to the latter (79.5±3.6 vs. 77.7±3.3 years, P=0.04, Table 1). Chronic lung and kidney diseases [glomerular filtration rate <60 mL/min/1.73 m2] were more frequently observed in the TAR group compared to the hybrid group (chronic lung disease: 29.0% vs. 10.7%, P=0.04; chronic kidney disease: 32.3% vs. 3.6%, P=0.002). No significant differences in any of the other risk factors were observed between the groups.
Twenty patients in the TAR group underwent concomitant procedures (Table 2). In the hybrid group (Table 3), 9 patients underwent frozen elephant trunk TAR, 6 patients underwent zone 0 TEVAR, 1 patient underwent zone 1 TEVAR, and 12 patients underwent zone 2 TEVAR (of which, 5 did not undergo LCCA to LSA bypass surgery). The length of the inserted stent graft was 158.6±24.7 mm.
Table 2
| Details of operation | Values (n=62) |
|---|---|
| Concomitant procedure | |
| Coronary artery bypass grafting | 11 (17.4) |
| Mitral valve replacement | 2 (3.2) |
| Aortic valve replacement | 2 (3.2) |
| Tricuspid valve annuloplasty | 1 (1.6) |
| Pulmonary valve replacement | 1 (1.6) |
| Aortic root replacement | 2 (3.2) |
| Aortic root remodeling | 1 (1.6) |
| Surgical duration, min | 364±76 |
| Cardiopulmonary bypass duration, min | 184±43 |
| Cross-clamping duration, min | 129±34 |
| Selective cerebral perfusion duration, min | 79±21 |
Data are shown as mean ± SD or n (%). TAR, total arch replacement.
Table 3
| Details of operation | Hybrid procedure (n=28) |
|---|---|
| Frozen elephant trunk, n (%) | 9 (32.1) |
| Zone 0, n (%) | 6 (21.4), total debranching bypass with TEVAR |
| Zone 1, n (%) | 1 (3.6), RCCA to LCCA and LSA |
| Zone 2, n (%) | 12 (42.9), LCCA to LSA (n=7), no bypass (n=5) |
TEVAR, thoracic endovascular repair; RCCA, right common carotid artery; LCCA, left common carotid artery; LSA, left subclavian artery.
Post-operative results
The length of intensive care unit (ICU) stay was not significantly different in both groups (Table 4), but excluding waiting period between first and second operation in hybrid group, the length of ICU stay was significantly shorter in hybrid group (2.6±3.0 vs. 5.9±9.2, P=0.03). The in-hospital mortality rate was 3.3% (3 out of 90 patients) overall, and no significant differences were observed between the two groups (TAR: 1.6%, hybrid: 7.1%, P=0.22, Table 4). One patient in the TAR group died on post-operative day (POD) 13 due to post-surgical cerebral infarction, while 2 patients in the hybrid group died from sepsis with empyema after zone 0 TEVAR and cerebral infarction after zone 1 TEVAR on PODs 19 and 7, respectively.
Table 4
| Outcomes | TAR (n=62) | Hybrid (n=28) | P value |
|---|---|---|---|
| Length of ICU stay, days, mean ± SD | 5.9±9.2 | 5.1±7.6 | 0.72 |
| Length of hospitalization, days, mean ± SD | 25.0±32.5 | 17.2±19.6 | 0.24 |
| Mortality on hospitalization, n (%) | 1 (1.6)* | 2 (7.1)** | 0.22 |
| Tracheostomy, n (%) | 6 (9.7) | 3 (10.7) | >0.99 |
| Complications, n (%) | |||
| Cerebral infarction | 6 (9.7) | 2 (7.1) | >0.99 |
| SDH, SAH | 2 (3.2) | 1 (3.6) | >0.99 |
| Pneumonia | 6 (9.7) | 2 (7.1) | >0.99 |
| Temporary SCI | 1 (1.6) | 1 (3.6) | 0.52 |
| Permanent SCI | 0 (0.0) | 1 (3.6)*** | 0.31 |
| Bowel ischemia | 1 (1.6) | 1 (3.6) | 0.52 |
| AKI on hemodialysis | 1 (1.6) | 0 (0.0) | >0.99 |
| Dysphagia | 2 (3.2) | 3 (10.7) | 0.17 |
| Mediastinitis | 1 (1.6) | 0 (0.0) | >0.99 |
*, cerebral infarction; **, empyema sepsis, cerebral infarction; ***, permanent paraplegia. TAR, total arch replacement; ICU, intensive care unit; SD, standard deviation; SDH, subdural hemorrhage; SAH, subarachnoid hemorrhage; SCI, spinal cord injury; AKI, acute kidney injury.
No significant differences in the incidence of post-operative complications were observed between the two groups. In the TAR group, cerebral infarctions and peri-operative cerebral (subdural or subarachnoid) hemorrhages were observed in 6 (9.7%) and 2 (3.2%) patients, respectively, while the corresponding numbers in the hybrid group were 2 (7.1%) and 1 (3.6%) patient, respectively. One patient (3.6%) in the hybrid group exhibited permanent spinal cord injury and paraplegia after frozen elephant trunk TAR.
Mid-term follow up results
Mid-term survival rate analysis using Kaplan-Meier curves showed no significant differences between the two groups (P=0.31, Figure 2). In the TAR group, the freedom from all-cause mortality rates 1, 3, and 5 years after treatment were 82%, 71%, and 71%, respectively, while the corresponding values in the hybrid group were 80%, 68%, and 52%, respectively.

Late aortic re-intervention occurred in 6 patients, of which 1 (1.6%) was in the TAR group and 5 (17.9%) were in the hybrid group. The freedom-from-re-intervention analysis showed significantly better outcomes in the TAR group compared to the hybrid group (P=0.04, Figure 3), with the freedom from re-intervention rates 1, 3, and 5 years after treatment being 100%, 93%, and 93%, respectively, in the TAR group and 90%, 80%, and 80%, respectively, in the hybrid group. One patient exhibited a distal anastomosis leak with pseudoaneurysm formation, concealed by pleural adhesion, 28 months after TAR and underwent re-intervention using a TEVAR graft. The patient was discharged from the hospital without occurrence of any complications. In the hybrid group, 5 patients underwent re-intervention for type IB endoleak (3 patients; durations: 3 days, 30 months, and 75 months after surgery), type II endoleak (1 patient, duration: 26 months after surgery), and aortoesophageal fistula (1 patient, duration: 3 months after surgery), and the median duration until re-intervention was 26 months (interquartile range: 3–30) after surgery. Patients with type Ib endoleaks received additional TEVAR grafts at the leakage site, while those with type II leaks were treated using coil embolization in the collateral arteries for the progression of aneurysmal dilatation. The patient with an aortoesophageal fistula received a TEVAR graft at the affected site, but died from sepsis 25 days after re-intervention. The multivariate Cox regression analysis showed that CKD was an independent positive predictor of post-operative mortality (HR: 2.957, P=0.02) during the follow-up period (Table 5).
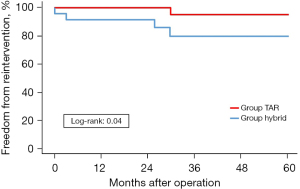
Table 5
| Variable | Univariate | Multivariate | |||
|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | ||
| Hybrid group | 0.987 (0.438–2.214) | 0.97 | |||
| Age | 1.120 (1.013–1.239) | 0.03 | 1.073 (0.950–1.211) | 0.25 | |
| Ejection fraction | 1.003 (0.989–1.017) | 0.70 | |||
| Sex (male) | 0.977 (0.410–2.233) | 0.96 | |||
| Neurological dysfunction | 2.424 (0.569–10.327) | 0.23 | |||
| Diabetes | 1.227 (0.491–3.064) | 0.66 | |||
| Diabetes on insulin | 1.326 (0.307–5.725) | 0.71 | |||
| Ischemic heart disease | 2.009 (0.906–4.454) | 0.08 | 1.134 (0.419–3.070) | 0.81 | |
| Other heart disease | 1.077 (0.449–2.582) | 0.87 | |||
| COPD | 1.666 (0.718–3.865) | 0.24 | |||
| Other lung disease | 1.201 (0.521–2.770) | 0.67 | |||
| Chronic kidney disease | 3.207 (1.420–7.244) | 0.005 | 2.957 (1.162–7.525) | 0.02 | |
| History of malignant disease | 1.321 (0.555–3.144) | 0.53 | |||
| Other vascular disease | 1.357 (0.903–2.038) | 0.14 | 0.728 (0.244–2.179) | 0.57 | |
| History of cardiac or thoracic aorta surgery | 2.056 (0.106–1.244) | 0.15 | 1.691 (0.437–6.546) | 0.45 | |
| Poor mobility | 7.996 (1.023–62.490) | 0.05 | 4.905 (0.427–56.313) | 0.20 | |
| Carotid stenosis (>50%) | 2.366 (1.049–5.338) | 0.04 | 2.424 (0.902–6.514) | 0.08 | |
| Cerebral vascular stenosis | 0.895 (0.387–2.074) | 0.80 | |||
| Pulmonary hypertension | 1.308 (0.711–2.405) | 0.39 | |||
| Emergency operation | 1.913 (0.801–4.568) | 0.14 | 1.474 (0.504–4.310) | 0.48 | |
| NYHA class | 0.835 (0.377–1.851) | 0.66 | |||
HR, hazard ratio; CI, confidence interval; COPD, chronic obstructive pulmonary disease; NYHA class, New York heart association class.
Discussion
Advanced age is an independent predictor of early post-operative complications in patients undergoing conventional TAR (6,7). Although previous studies have suggested that hybrid arch procedures are relatively safer in elderly patients (1,2,8-10), they have been unable to demonstrate significant differences in mortality between the two procedures. In the results of the current study, the clinical outcomes of the hybrid procedure in elderly patients are not better than the outcomes of TAR, but the re-intervention rates were higher in the former group and usually occurred within three years after surgery.
Murashita et al. (2) found that hybrid procedures were safer than TAR when treating aortic arch aneurysms in high-risk patients, and emphasized that early outcomes such as mortality and morbidity were similar between the two procedures despite patients in the hybrid group being at higher risk. In the current study, patients in the hybrid group recovered more rapidly after the operation and started post-operative rehabilitation faster than patients in TAR. However, no significant differences in in-hospital mortality rates were observed upon comparing the two procedures (TAR: 1.6%, hybrid: 7.1%, P=0.22, Table 4), although there was significantly more COPD and CKD in the TAR group. This was in agreement with previous evidence suggesting that post-operative mortality did not significantly differ between the TAR and hybrid groups, with early mortality rates being 4–10% for aortic arch operations with selective cerebral perfusion and 2–6% for hybrid procedures using stent grafts (11-16). The current study also found that old age was not a surgical risk factor (Table 5), and this was in agreement with previous evidence (17-19). The main difference between the hybrid and TAR procedures lies in the incidence of remnant aortic aneurysms which can create pressure by pressing on the surrounding tissues such as the esophagus and trachea and increase the risk of re-intervention. Significantly fewer patients in the TAR group required aortic re-intervention compared to the hybrid group (P=0.04). Yoshitake et al. (18) recently compared aortic arch repair using the endovascular technique, TAR, and staged surgery and found that the mid-term survival was similar between the hybrid procedure and TAR. However, TEVAR grafts were associated with an increased risk of re-intervention, the majority of which occurred within 3 years after surgery. The findings of the current study were in agreement with previous evidence suggesting that the majority of re-interventions occurred within 3 years of hybrid surgery, with the approximate freedom from re-intervention rate being 80–95% (20-23). The life-expectancy in South Korea in 2020 was 83.5 years (24). For this reason, reintervention after the hybrid procedure could occur in elderly patients within their life expectancy, and we must not ignore the risk of reintervention after the hybrid procedure in elderly patients.
In the current study, the incidence of post-operative neurological complications did not significantly differ between the two groups, and this was in agreement with Cao et al. (25) who also reported similar mortality and post-operative neurological outcomes between the hybrid and conventional TAR groups. Their systematic review of the clinical outcomes of hybrid arch procedures concluded that hybrid repair of the aortic arch was associated with negligible risk of peri-operative mortality and neurological morbidity, although the authors emphasized the lack of longitudinal evidence preventing ascertainment of the durability of the procedure.
Limitations
This study had several limitations. Firstly, the sample size was too small to conclude about a higher reintervention rate risk in the hybrid group. For this reason, further investigation using a larger cohort and longer follow-up is necessary. Secondly, patient characteristics and surgical procedures in both groups were not controlled. Thirdly, the indication of hybrid procedure was not controlled because this was a multicenter cohort study, and the indication of hybrid procedure differed in each hospital and operator. And in selecting patients for hybrid procedures besides age and comorbidities, anatomical characteristics of the aorta were also critical factors for selecting patients for hybrid procedures. More chronic kidney disease patients were in the TAR group for these reasons. Finally, only some patients were followed-up in the current study, suggesting potential inaccuracies in the long-term follow-up data.
Conclusions
The treatment outcomes of the hybrid procedure did not significantly differ from those of TAR, although the re-intervention rates were higher in the former group and usually occurred within 3 years after surgery. Therefore, the risk of re-intervention should be taken into consideration when treating elderly patients, and selection of the surgical strategy for aortic arch aneurysms should be based on the patient’s demographic and anatomical characteristics.
Acknowledgments
Funding: Financial support was provided by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-331/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-331/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-331/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-331/coif). YHC receives financial support provided by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Korean government (the Ministry of Health & Welfare) (No. HI22C1784 to YHC). The other authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Milewski RK, Szeto WY, Pochettino A, et al. Have hybrid procedures replaced open aortic arch reconstruction in high-risk patients? A comparative study of elective open arch debranching with endovascular stent graft placement and conventional elective open total and distal aortic arch reconstruction. J Thorac Cardiovasc Surg 2010;140:590-7. [Crossref] [PubMed]
- Murashita T, Matsuda H, Domae K, et al. Less invasive surgical treatment for aortic arch aneurysms in high-risk patients: a comparative study of hybrid thoracic endovascular aortic repair and conventional total arch replacement. J Thorac Cardiovasc Surg 2012;143:1007-13. [Crossref] [PubMed]
- Preventza O, Tan CW, Orozco-Sevilla V, et al. Zone zero hybrid arch exclusion versus open total arch replacement. Ann Cardiothorac Surg 2018;7:372-9. [Crossref] [PubMed]
- Settepani F, Cappai A, Basciu A, et al. Outcome of open total arch replacement in the modern era. J Vasc Surg 2016;63:537-45. [Crossref] [PubMed]
- Greenland S, Mickey RM. Re: "The impact of confounder selection criteria on effect estimation. Am J Epidemiol 1989;130:1066. [Crossref] [PubMed]
- Kazui T, Washiyama N, Muhammad BA, et al. Total arch replacement using aortic arch branched grafts with the aid of antegrade selective cerebral perfusion. Ann Thorac Surg 2000;70:3-8; discussion 8-9. [Crossref] [PubMed]
- Czerny M, Fleck T, Zimpfer D, et al. Risk factors of mortality and permanent neurologic injury in patients undergoing ascending aortic and arch repair. J Thorac Cardiovasc Surg 2003;126:1296-301. [Crossref] [PubMed]
- Pecoraro F, Lachat M, Hofmann M, et al. Mid-term results of zone 0 thoracic endovascular aneurysm repair after ascending aorta wrapping and supra-aortic debranching in high-risk patients. Interact Cardiovasc Thorac Surg 2017;24:882-9. [Crossref] [PubMed]
- Ferrero E, Ferri M, Viazzo A, et al. Is total debranching a safe procedure for extensive aortic-arch disease? A single experience of 27 cases. Eur J Cardiothorac Surg 2012;41:177-82. [Crossref] [PubMed]
- Minatoya K, Ogino H, Matsuda H, et al. Is conventional aortic arch surgery justifiable in octogenarians? J Thorac Cardiovasc Surg 2010;139:641-5. [Crossref] [PubMed]
- Kazui T, Yamashita K, Washiyama N, et al. Aortic arch replacement using selective cerebral perfusion. Ann Thorac Surg 2007;83:S796-8; discussion S824-31. [Crossref] [PubMed]
- Di Eusanio M, Schepens MA, Morshuis WJ, et al. Antegrade selective cerebral perfusion during operations on the thoracic aorta: factors influencing survival and neurologic outcome in 413 patients. J Thorac Cardiovasc Surg 2002;124:1080-6. [Crossref] [PubMed]
- Ogino H, Sasaki H, Minatoya K, et al. Evolving arch surgery using integrated antegrade selective cerebral perfusion: impact of axillary artery perfusion. J Thorac Cardiovasc Surg 2008;136:641-8; discussion 948-9. [Crossref] [PubMed]
- Svensson LG, Rushing GD, Valenzuela ES, et al. Modifications, classification, and outcomes of elephant-trunk procedures. Ann Thorac Surg 2013;96:548-58. [Crossref] [PubMed]
- Preventza O, Garcia A, Cooley DA, et al. Total aortic arch replacement: A comparative study of zone 0 hybrid arch exclusion versus traditional open repair. J Thorac Cardiovasc Surg 2015;150:1591-8; discussion 1598-600. [Crossref] [PubMed]
- Kulik A, Castner CF, Kouchoukos NT. Outcomes after total aortic arch replacement with right axillary artery cannulation and a presewn multibranched graft. Ann Thorac Surg 2011;92:889-97. [Crossref] [PubMed]
- Hiraoka A, Chikazawa G, Totsugawa T, et al. Open total aortic arch reconstruction for patients with advanced age in the era of endovascular repair. J Thorac Cardiovasc Surg 2014;148:77-82. [Crossref] [PubMed]
- Yoshitake A, Okamoto K, Yamazaki M, et al. Comparison of aortic arch repair using the endovascular technique, total arch replacement and staged surgery†. Eur J Cardiothorac Surg 2017;51:1142-8. [Crossref] [PubMed]
- Seike Y, Matsuda H, Fukuda T, et al. Total arch replacement versus debranching thoracic endovascular aortic repair for aortic arch aneurysm: what indicates a high-risk patient for arch repair in octogenarians? Gen Thorac Cardiovasc Surg 2018;66:263-9. [Crossref] [PubMed]
- Shiraya S, Nakamura Y, Harada S, et al. Debranching thoracic endovascular aortic repair for distal aortic arch aneurysm in elderly patients aged over 75 years old. J Cardiothorac Surg 2020;15:13. [Crossref] [PubMed]
- Son SA, Jung H, Cho JY. Long-term outcomes of intervention between open repair and endovascular aortic repair for descending aortic pathologies: a propensity-matched analysis. BMC Surg 2020;20:266. [Crossref] [PubMed]
- Adams JD, Angle JF, Matsumoto AH, et al. Endovascular repair of the thoracic aorta in the post-FDA approval era. J Thorac Cardiovasc Surg 2009;137:117-23. [Crossref] [PubMed]
- Iba Y, Minatoya K, Matsuda H, et al. How should aortic arch aneurysms be treated in the endovascular aortic repair era? A risk-adjusted comparison between open and hybrid arch repair using propensity score-matching analysis. Eur J Cardiothorac Surg 2014;46:32-9. [Crossref] [PubMed]
- Statistics Korea. The life-expectancy in South Korea. Statistics Korea, Seoul. Available online: https://www.index.go.kr/unify/idx-info.do?idxCd=8016. Accessed 10 November 2022.
- Cao P, De Rango P, Czerny M, et al. Systematic review of clinical outcomes in hybrid procedures for aortic arch dissections and other arch diseases. J Thorac Cardiovasc Surg 2012;144:1286-300, 1300.e1-2.


