A propensity matched comparison of effects between video assisted thoracoscopic single-port, two-port and three-port pulmonary resection on lung cancer
Introduction
Currently, video assisted thoracoscopic surgery (VATS) lobectomy with systematic lymph node dissection has been a widespread standard surgical procedure for early stage non-small cell lung cancer (NSCLC) in the past 20 years, with decreased postoperative morbidities, shortened hospital length of stay, and improved 5-year survival compared with open lobectomy (1,2). A multicenter study and several single center studies which used propensity matched analysis in the last 2 years demonstrated decreased postoperative morbidities and shortened hospital length of stay in VATS approach compared with open pulmonary resection approach, although comparable instead of improved 5-year survival was noted (3-8).
The mechanism of decreased rate of postoperative morbidities may lie in reduced inflammatory reaction. Liu et al. found that the level of serum C reaction protein (CRP), tumor necrosis factor α (TNF-α), interleukin 6 (IL-6) and IL-10 in the VATS group were significantly lower after VATS pulmonary operation compared with the open thoracotomy group (9). Since reduction of incision length could reduce the inflammatory responses, one would hypothesize that whether the number of VATS incisions decrease to two or one minimal incision could reduce the surgical reaction more significantly compared with standard VATS three-port pulmonary resection. Preliminary studies of VATS single-port pulmonary resection demonstrated that VATS single-port was feasible and safe, with comparable short term outcomes compared with three-port VATS pulmonary resection (10-16). However, there were few studies regarding the comparison among single-port, two-port and three-port approaches (14,15). Therefore, the aim of this study was to summarize our experiences of single-port, two-port and three-port VATS pulmonary resection, focusing on the difference of peri-operative outcomes between these approaches.
Methods
This is a prospective study which was performed in the Department of Thoracic Surgery in Cancer Hospital of Chinese Academy of Medical Sciences and Peking Union Medical College between November 2014 and January 2016. This study was approved by the institutional review board at Cancer Hospital of Chinese Academy of Medical Sciences and Peking Union Medical College, and all patients provided written informed consent before operation.
All patients who underwent VATS pulmonary resection for lung cancer between November 2014 and January 2016 were included. The inclusion criteria for VATS pulmonary resection included: clinically staged T0–2N0–1M0 patients with American Society of Anesthesiologists (ASA) score of I–II. Exclusion criteria included ASA score of III–IV and serious co-morbidities which carried higher perioperative risks, the selection of which procedure was mainly based on the experiences of surgeons. Junior surgeons who performed less than 50 VATS operations per year mainly perform three-port VATS pulmonary resection. While senior surgeons who performed more than 100 VATS operations per year attempted both three-port and single-port and two-port VATS pulmonary resections.
Patients were divided into two groups according to the number of incisions: three-port group and single-port and two-port groups. Variables studied in each patient included age, sex, co-morbidities including hypertension, coronary heart disease and chronic obstructive pulmonary disease, tumor size and position, type and duration of operation, pathological stage, histological type, number of lymph nodes retrieved, duration of chest tube, hospital length of stay, and postoperative complications. The hospital expense and cost of operation were also recorded.
Lung cancer staging were carried out according to American Joint Committee on Cancer (AJCC) 2009 cancer staging (17). Postoperative complications were defined and graded according to thoracic morbidity and mortality (TM&M) system and joint standardization of variable definitions and terminology of The Society of Thoracic Surgeons (STS) and The European Society of Thoracic Surgeons (ESTS) General Thoracic Surgery Databases (18,19).
Surgical procedures
All surgical procedures were performed under general anesthesia with double-lumen intubation. Patients were placed in the full lateral decubitus position, and the operator and thoracoscopic assistant stood at the anterior side of the patient.
We started VATS single-port pulmonary resection since November 2014 (16). Single-port VATS pulmonary resection procedures were accomplished based on the techniques reported by Gonzalez-Rivas et al. (10) and our previous experiences of VATS three-port pulmonary resection (16,20). VATS single-port pulmonary resection procedures were performed as follows. The incision, about 3 to 5 cm long, is performed at the fifth or sixth intercostal space at the middle axillary line. In most cases, the camera was placed at the posterior side of the incision, and other working instruments were placed at the anterior side. Both the operator and the thoracoscopic assistant stand at the anterior side of the patient. When the end stapler is applied, the camera’s position must be changed to accommodate the stapler. All pulmonary vessels and bronchus in the resected lobe or sub lobe were basically sectioned with the use of endoscopic staplers. Usually, the bronchus is resected at the last stage of lobectomy or sub-lobectomy. The specimen was put in the bag under the thoracoscopic assistance and was removed through the incision protector (10).
The details of VATS three-port pulmonary resection procedures were reported previously (16,20). Generally, one port for viewing was done at 7th intercostal spaces on the middle axillary line, and two ports for working on the anterior axillary line and posterior axillary line respectively, on which the intercostal spaces in detail according to the location of lesion by CT. Thoracoscopic segmentectomy began with identification and ligation of segmental vein. Subsequently, the bronchus or artery was ligated, which depended on the segment resected. The segmental pulmonary veins, arteries, and bronchi were dissected by electrocantery and stapled by endoscopic stapler separately. We used reventilation to confirm the intersegmental plane according to the inflation-deflation line and divided it by endoscopic stapler. Intra operative frozen section must be used for examination of the station 10 and station 11–12 lymph nodes and resection margins after completion of segmentectomy. If a tumor was located on the edge of the segment or the resection margin was inadequate on frozen section intraoperatively, or the station 10 or station 11–12 lymph nodes are metastatic, a multiple segmentectomy or lobectomy should be available.
We started VATS two-port pulmonary resection from January 2015. For VATS two-port, the incision at the posterior axillary line was omitted in the VATS three-port approach.
Hilar or mediastinal lymph node dissection was performed for all patients. The procedure of dissection was selected based on the guidelines and previously reported techniques for VATS lobectomy (10).
Statistical analysis
The SPSS software package 16.0 for Windows was used for statistical analysis. Data were presented as mean value ± standard deviation for continuous variables, and percentages for dichotomous variables. Continuous variables were analyzed using t-test, and categorical variables were analyzed using Fisher exact test. We first performed overall unmatched analysis for all patients. Then we made propensity score analysis according to Austin PC (21). For propensity score analysis, we first made the logistic regression model that calculated propensity scores using approach (single-port and two-port or three-port) as outcome with age, sex, tumor size, procedures, and tumor location. Excluding patients with scores lower than 0.10 (high chance of undergoing single-port and two-port VATS) and higher than 0.90 (high chance of undergoing three-port VATS). We reported the absolute difference for variables after matching rather than statistical significance testing. We then performed analysis for all matched patients. The significant level was set as a P value less than 0.05.
Results
From November 2014 and January 2016, a total of 1,553 lung cancer patients received VATS pulmonary resection. There were 716 males and 837 females. The mean age was 58.90 years (range, 25–82 years).The conversion rate was 2.7% (42/1,553) in this cohort. In the single-port group, 5 patients were converted to open thoracotomy because of pulmonary artery bleeding and 3 patients were converted to three-port because of pleural adhesion. Four patients were converted to open thoracotomy as a result of dense pleural adhesion in the two-port group. Thirty patients were converted to thoracotomy in the three-port group.
The preoperative characteristics of 1,553 patients were displayed in Table 1. Compared with patients in single-port and two-port groups, patients who underwent three-port VATS were older (57 vs. 59 years, P=0.004), had more lobectomies (68.4% vs. 78.6%, P<0.001), more upper lobar lesions (50.6% vs. 58.8%, P=0.008) and larger tumor (1.98 vs. 2.20, P=0.005).
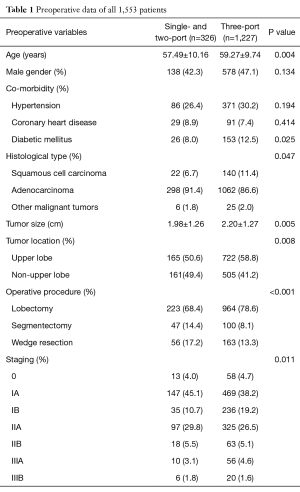
Full table
The perioperative outcomes of 1,553 patients are displayed in Table 2. Compared with single-port and two-port groups, patients in three-port group had significantly more lymph nodes retrieved. However, compared with patients underwent three-port VATS, patients in single-port and two-port groups experienced shorter postoperative length of stay (6.22 vs. 5.60 d, P=0.004), shorter duration of chest tube (4.95 vs. 4.28 d, P<0.001) and reduced volume of chest tube drainage (969 vs. 790 mL, P<0.001). However, there was no significant difference in the complication rate between two groups.
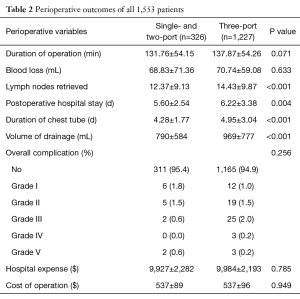
Full table
In order to eliminate the confounding effect of preoperative variables on the outcomes of lung cancer patients, we made propensity score matched analysis. The logistic regression model that calculated propensity scores using approach (single-port and two-port or three-port) as outcome with age, sex,, tumor size, procedures, and tumor location, which show good predictive capacity (c=0.62). Excluding patients with scores lower than 0.10 (high chance of undergoing single-port and two-port VATS) and higher than 0.90 (high chance of undergoing three-port VATS) resulted a subgroup of 887 patients with a predicted preoperative chance of undergoing three-port VATS. In this subgroup, 207 patients underwent single-port or two-port VATS, and 680 patients underwent three-port VATS.
The preoperative characteristics after matching were displayed in Table 3. There were no significant differences in age, gender, tumor size, location, operative procedures between two groups.
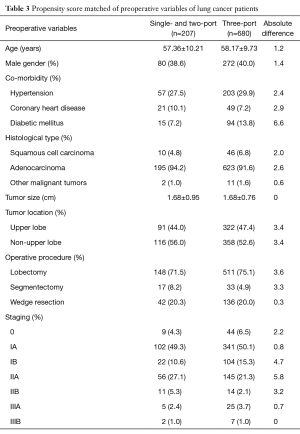
Full table
Propensity-matched analysis demonstrated that there were no significant differences in intra-operative blood loss, number of dissected lymph nodes, total hospital expense and cost of operation among three groups (Table 4). Compared with three-port group, patients who underwent single-port and two-port experienced shorter postoperative length of stay (6.24 vs. 5.61 d, P=0.033), shorter duration of chest tube (4.92 vs. 4.25 d, P=0.008), and decreased volume of drainage (926 vs. 791 d, P=0.003). Again, there was no significant difference in the morbidity rate between these two groups.
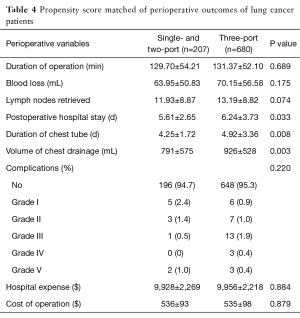
Full table
Discussion
In our study, we found that there were no significant differences in the short term outcomes between VATS single-port, two-port and three-port groups in the surgical treatment of lung cancer in terms of the complications rate. However, compared with three-port VATS pulmonary resection, single-port and two-port were associated with shorter postoperative length of stay, shorter duration of chest tube, and decreased volume of drainage.
The safety and feasibility of VATS single-port surgical treatment for lung cancer have been well elaborated in a number of studies with a complication rate of 4–14% (10-15). Gonzalez-Rivas et al. described the first series of single-port thoracoscopic lobectomy in 2013 (10). In that study, the conversion rate of single-port VATS lobectomy was 4.9% and the complication rate was 14.4%. They concluded that single-port thoracoscopic anatomic resection is a feasible and safe procedure with good perioperative results. In our previous study of 58 cases of VATS single-pot pulmonary resection, the conversion rate and the complication rate was 3.4% and 10.3% respectively (16). Recently, Chung et al. demonstrated that uniportal VATS lobectomy achieved comparable perioperative results compared with conventional VATS lobectomy, with no differences in postoperative complications, postoperative 30-day mortality or reoperation rate, operative time, number of removed lymph nodes, chest tube duration or length of postoperative hospital stay between the uniportal VATS group and conventional VATS group (22).
In China, VATS two-port pulmonary resection was first reported in 2010 (23). In that study, Chu et al. performed 21 cases of single utility VATS lobectomy and no severe complications occurred. The following study also affirmed the safety of VATS two-port pulmonary resection (24). Wang et al. reported that uniportal VATS lobectomy and segmentectomy achieved comparable perioperative results compared with multi incision VATS including two-port lobectomy and segmentectomy (14). However, no studies were reported on the comparison between two-port and three-port VATS pulmonary resection.
In the current study, we compared the perioperative outcomes between conventional three-port versus single-port and two-port VATS pulmonary resection. The complication rate was 4.6% and 5.1% in non-three-port (single-port and two-port) group and three-port respectively. There was no significant difference in complication rate between these two groups, which was consistent with the results of previous studies. Wang et al. reported that complication rate of uniportal VATS lobectomy and segmentectomy was 10%, which was similar to 13.66% in multi incision VATS group (14). Shen et al. conducted a propensity-matched study which demonstrated comparable perioperative outcomes the morbidity was 4.0% and 7.0% in single-port and multi-port group, respectively (15). Therefore, both single-port and two-port VATS pulmonary resection is safe and confers similar complication rate compared with conventional three-port VATS pulmonary resection.
In our study, significant difference in the number of removed lymph-nodes in un-matched analysis may be the result of imbalance of operative procedures in different incision group. After propensity score matching, the rate of operative procedures in different incision group was similar, and there are no significant differences between single- and two-port and three-port groups. Other study also reported the similar findings (15). Shen et al. reported mean number of lymph nodes was 21 in single-port VATS lobectomy group, which was similar to 20 in multi-port VATS lobectomy group. Combined literature and findings of our study, we concluded that single-port and two-port VATS pulmonary resection was safe without comprising oncologic effects compared with conventional three-port VATS pulmonary resection.
Besides, in the current study, we found that the volume of chest tube drainage was less in VATS single-port and two-port groups compared with VATS three-port group. The mechanism of this phenomenon was not clear. Relatively more cases of lobectomy in VATS three-port group than VATS single-port and two-port groups in unmatched patients may account for the results. However, after matching, single-port and two-port VATS were also associated with decreased volume of drainage compared with three-port group. The volume of drainage was 790 and 969 mL in single-port and two-port group and three-port group respectively, which was more than reported (25). In our center, the chest tube used in thoracic surgery was 28 F in general. And we removed the chest tube when the drainage was lower than 100 mL/d. Therefore, the volume and duration of chest tube may be more than others.
Our study found that single-port and two-port VATS were associated with shorter postoperative length of stay and shorter duration of chest tube compared with three-port group. This may be explained by decreased volume of drainage in single-port and two-port VATS group. Shen also found similar results, with length of stay in single-port group and multi-port group was 4.7 and 5.3 d, respectively.
There are two limitations in our study. Firstly, the number of patients who underwent VATS single-port and two-port pulmonary resection was relatively small. However, after matched for confounding factors including age, gender, tumor size, tumor location and operative procedure, the results of comparison between three VATS approaches for lung cancer were reliable. Secondly, the results were from one medical center, which limit the generalization of the conclusion. Multicenter or randomized controlled trials are needed to confirm the role of VATS single-port and two-port pulmonary resection in the surgical treatment of lung cancer.
In conclusion, the short term outcomes between VATS single-port, two-port and three-port groups in the surgical treatment of lung cancer were comparable. VATS single-port and two-port pulmonary resection were associated with decreased volume of drainage, shorter length of stay and shorter duration of chest tube.
Acknowledgements
Funding: Collaborative Innovation Center for Cancer Medicine Fund (ZLYXXTCX-201509) and Beijing Hope Run Special Fund (LC2015L21).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the institutional review board at Cancer Hospital of Chinese Academy of Medical Sciences and Peking Union Medical College, and all patients provided written informed consent before operation.
References
- Chen FF, Zhang D, Wang YL, et al. Video-assisted thoracoscopic surgery lobectomy versus open lobectomy in patients with clinical stage I non-small cell lung cancer: a meta-analysis. Eur J Surg Oncol 2013;39:957-63. [Crossref] [PubMed]
- Cai YX, Fu XN, Xu QZ, et al. Thoracoscopic lobectomy versus open lobectomy in stage I non-small cell lung cancer: a meta-analysis. PLoS One 2013;8:e82366. [Crossref] [PubMed]
- Nwogu CE, D'Cunha J, Pang H, et al. VATS lobectomy has better perioperative outcomes than open lobectomy: CALGB 31001, an ancillary analysis of CALGB 140202 (Alliance). Ann Thorac Surg 2015;99:399-405. [Crossref] [PubMed]
- Stephens N, Rice D, Correa A, et al. Thoracoscopic lobectomy is associated with improved short-term and equivalent oncological outcomes compared with open lobectomy for clinical stage I non-small-cell lung cancer: a propensity-matched analysis of 963 cases. Eur J Cardiothorac Surg 2014;46:607-13. [Crossref] [PubMed]
- Paul S, Isaacs AJ, Treasure T, et al. Long term survival with thoracoscopic versus open lobectomy: propensity matched comparative analysis using SEER-Medicare database. BMJ 2014;349:g5575. [Crossref] [PubMed]
- Berry MF, D'Amico TA, Onaitis MW, et al. Thoracoscopic approach to lobectomy for lung cancer does not compromise oncologic efficacy. Ann Thorac Surg 2014;98:197-202. [Crossref] [PubMed]
- Murakawa T, Ichinose J, Hino H, et al. Long-term outcomes of open and video-assisted thoracoscopic lung lobectomy for the treatment of early stage non-small cell lung cancer are similar: a propensity-matched study. World J Surg 2015;39:1084-91. [Crossref] [PubMed]
- Falcoz PE, Puyraveau M, Thomas PA, et al. Video-assisted thoracoscopic surgery versus open lobectomy for primary non-small-cell lung cancer: a propensity-matched analysis of outcome from the European Society of Thoracic Surgeon database. Eur J Cardiothorac Surg 2016;49:602-9. [Crossref] [PubMed]
- Liu Y, Zhao H, Liu J, et al. Influence of thoracoscopic surgery on inflammatory reaction of the body for early peripheral lung cancer patients. Zhongguo Fei Ai Za Zhi 2014;17:730-3. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Ismail M, Helmig M, Swierzy M, et al. Uniportal VATS: the first German experience. J Thorac Dis 2014;6:S650-5. [PubMed]
- Hsu PK, Lin WC, Chang YC, et al. Multiinstitutional analysis of single-port video-assisted thoracoscopic anatomical resection for primary lung cancer. Ann Thorac Surg 2015;99:1739-44. [Crossref] [PubMed]
- Ng CS, Kim HK, Wong RH, et al. Single-port video-assisted thoracoscopic major lung resections: experience with 150 consecutive cases. Thorac Cardiovasc Surg 2016;64:348-53. [Crossref] [PubMed]
- Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [Crossref] [PubMed]
- Shen Y, Wang H, Feng M, et al. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: a propensity-matched study. Eur J Cardiothorac Surg 2016;49:i48-53. [PubMed]
- Mu JW, Gao SG, Xue Q, et al. A Matched Comparison Study of Uniportal Versus Triportal Thoracoscopic Lobectomy and Sublobectomy for Early-stage Nonsmall Cell Lung Cancer. Chin Med J (Engl) 2015;128:2731-5. [Crossref] [PubMed]
- Edge SB, Byrd DR, Compton CC, et al. AJCC Cancer Staging Handbook. 7thed. New York: Springer-Verlag, 2010:299-323.
- Fernandez FG, Falcoz PE, Kozower BD, et al. The Society of Thoracic Surgeons and the European Society of Thoracic Surgeons general thoracic surgery databases: joint standardization of variable definitions and terminology. Ann Thorac Surg 2015;99:368-76. [Crossref] [PubMed]
- Seely AJ, Ivanovic J, Threader J, et al. Systematic classification of morbidity and mortality after thoracic surgery. Ann Thorac Surg 2010;90:936-42. [Crossref] [PubMed]
- Mu JW, Chen GY, Sun KL, et al. Application of video-assisted thoracic surgery in the standard operation for thoracic tumors. Cancer Biol Med 2013;10:28-35. [PubMed]
- Austin PC. Propensity-score matching in the cardiovascular surgery literature from 2004 to 2006: a systematic review and suggestions for improvement. J Thorac Cardiovasc Surg 2007;134:1128-35. [Crossref] [PubMed]
- Chung JH, Choi YS, Cho JH, et al. Uniportal video-assisted thoracoscopic lobectomy: an alternative to conventional thoracoscopic lobectomy in lung cancer surgery? Interact Cardiovasc Thorac Surg 2015;20:813-9. [Crossref] [PubMed]
- Chu X, Xue Z, Zhang L, et al. Primary report of lobectomy with single utility port complete video-assisted thoracoscopic surgery. Zhongguo Fei Ai Za Zhi 2010;13:19-21. [PubMed]
- Xu C, Ma H, Ni B, et al. Analysis of single-operation-hole thoracoscopic lobectomy in 113 clinical cases. Zhongguo Fei Ai Za Zhi 2014;17:424-7. [PubMed]
- Xie HY, Xu K, Tang JX, et al. A prospective randomized, controlled trial deems a drainage of 300 ml/day safe before removal of the last chest drain after video-assisted thoracoscopic surgery lobectomy. Interact Cardiovasc Thorac Surg 2015;21:200-5. [Crossref] [PubMed]


