
A comparison of the short-term outcomes of simple and complex segmentectomy via uniportal video-assisted thoracoscopic surgery
Highlight box
Key findings
• Uniportal video-assisted thoracoscopic surgery (VATS) complex segmentectomy is a safe and feasible treatment compared to uniportal VATS simple segmentectomy for patients with clinical stage 1A non-small-cell lung cancer (NSCLC).
What is known and what is new?
• Performing complex segmentectomy using uniportal VATS is a more challenging and intricate surgical procedure compared to simple segmentectomy or lobectomy.
• There were no notable differences observed between the two groups concerning patient and tumor characteristics, operative and postoperative outcomes, except for the surgical margin distances. It is likely to encounter a short resection margin in cases where complex segmentectomy is performed.
What is the implication, and what should change now?
• The location of the tumor should be thoroughly evaluated when performing uniportal VATS complex segmentectomy.
Introduction
Since 1960, lobectomy has been considered to be the standard surgical treatment for early-stage lung cancer, and it has been observed to be more effective than sublobar resection (wedge resection and segmentectomy) for patients with peripheral T1N0 non-small-cell lung cancer (NSCLC), resulting in lower rates of death and local recurrence (1,2). However, recent randomized trials, namely the JCOG0802/WJOG4607L trial and CALGB 140503 trial, have revealed that segmentectomy is a valid alternative treatment option for patients with peripheral NSCLC who have a tumor size of 2 cm or less and pathologically confirmed node-negative disease. These trials have indicated that segmentectomy offers comparable outcomes to lobectomy in terms of disease-free and overall survival, demonstrating that it can be a feasible alternative for such patients (3,4). The increased usage of low-dose chest computed tomography (CT) for screening has resulted in the detection of early-stage lung cancer with tumors smaller than 2 cm (5). Consequently, there has been a rise in the usage of segmentectomy as a treatment approach. Segmentectomy can be categorized into two types, simple and complex, based on the number of intersegmental planes that require dissection. Simple segmentectomy encompasses procedures such as superior segmentectomy, upper division segmentectomy, and lingular segmentectomy (6).
Over the past few decades, uniportal video-assisted thoracoscopic surgery (VATS) has rapidly developed worldwide (7-9). Performing complex segmentectomy via uniportal VATS is a more demanding and intricate procedure than simple segmentectomy and lobectomy and can give rise to various complications, thereby raising doubts about its advantages for the patient (10).
The objective of this study is to evaluate the safety and feasibility of uniportal VATS complex segmentectomy compared to uniportal VATS simple segmentectomy by investigating the initial surgical outcomes. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-627/rc).
Methods
Patient population
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Institutional Review Board of the Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea (No. PC23RASI0062), which did not require individual consent for this retrospective study. From May 2019 to February 2023, 476 patients with a lung cancer who underwent surgery by a single surgeon at the Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea were reviewed. After excluding 277 patients who received uniportal VATS wedge resection, lobectomy, bilobectomy, or pneumonectomy, 199 patients were included in the study. Out of these, 67 patients underwent uniportal VATS simple segmentectomy, while 132 patients underwent uniportal VATS complex segmentectomy, both with complete microscopic resection (R0). A flow chart of the study design is shown in Figure 1.
Surgical technique
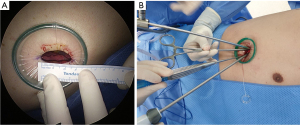
Segmentectomy is the surgical procedure of choice in our institution for patients diagnosed with peripheral NSCLC who meet specific criteria, including a tumor size of 2 cm or smaller and no evidence of lymph node involvement. The decision regarding which lung segment to remove is made by the surgeon after a meticulous review of the chest CT scan. All procedures were performed with patients in the lateral decubitus position. The surgical incision, approximately 2.5 cm in length, was made in the anterior axillary line at either the fourth or fifth intercostal space (ICS), depending on the location of the target lesion (Figure 2A). For both upper lobes, the typical working incision was made at the fourth ICS. For both lower lobes, the working incision was made at the fifth ICS. The working port was covered with a small wound protector. A 5-mm, 30° scope was positioned at the upper side of the incision by the surgical assistant. A curved suction tip, grasping instruments, Harmonic scalpel, and articulating endostaplers were inserted through the single incision (Figure 2B). Our approach aimed to achieve adequate resection margins of at least 2 cm or tumor size observed on CT scans after segmentectomy. Prior to initiating the segmentectomy, our approach involved attempting to palpate the lesions and marking them with a marking pen if they were detectable by touch using a curved suction tip. In cases where the target lesion was not palpable, we would carefully review the CT scans and proceed with palpation after segment retrieval, assuming that the lesion would be located within the retrieved segments. Target segmental pulmonary arteries and veins were clipped with either hemolock or silk tie, followed by transection of the vessels using a Harmonic scalpel. The endostaplers were utilized to divide the target segmental bronchi. In order to delineate the intersegmental plane, we employed a technique involving the systemic injection of indocyanine green (ICG) and utilized scopes with different specifications. Initially, a 5-mm, 30° scope was used, which was later switched to a 10-mm, 30° scope equipped with near-infrared fluorescence imaging capabilities. Following the injection of ICG, the intersegmental plane was divided using multiple endostaplers (Figure 3). The lung inflation technique was implemented as an alternative method for delineating the intersegmental plane, in the absence of ICG devices. When dividing the intersegmental planes, it is essential to remove the bronchial and vessel stumps of the resected segment simultaneously. Patients with tumors showing pure ground glass opacity (GGO) and part-solid GGO underwent lobe-specific lymph nodal dissection. In patients with tumors displaying part-solid GGO and solid patterns with standardized uptake values (SUVs) higher than 2.5 on FDG-positron emission tomography (PET)/CT, systematic lymph node dissection was performed. Intraoperative frozen sections were utilized to confirm the absence of N1 node metastasis. Following the segmentectomy, the detection of an air leak from the closure of the bronchus and stapler lines was assessed by inflating the lung under water. If an air leak was observed, it was addressed through the application of manual sutures, polyglycolic acid (PGA) sheets, or fibrin adhesives. All patients received an intercostal nerve block using 1 mL of bupivacaine in each space beneath the lower margin of the third through seventh ribs. Before closing the incision, a 20-French chest tube was inserted through the lower part of the incision. The working incision was closed in layers, and the skin was closed using a unidirectional absorbable barbed suture (Figure 4).


Postoperative management
Following the operation, the chest tube was connected to a digital drainage system (DDS) (Thopaz; Medela Healthcare, Baar, Switzerland) with a suction pressure of −15 cmH2O. On the first postoperative day (POD), the suction pressure was lowered to −7 cmH2O and remained at that level until the chest tube was removed. The chest tube was removed after 12 hours of no air leakage and a drainage volume of less than 200 mL per day. The patient was discharged as per their preference, either 1 day after chest tube removal, until after the final pathology report was obtained, or because they resided far from the hospital.
Statistical analysis
The medians [interquartile ranges (IQRs)] were used to express continuous variables, while numbers (percentages) were used to present categorical variables. Fisher’s exact test or Pearson’s chi-squared test was used to compare simple and complex segmentectomies for categorical variables, and the Wilcoxon rank sum test was utilized to compare continuous variables. All statistical analyses were performed using R software (RStudio version 4.2.0; R Foundation for Statistical Computing, Vienna, Austria; https://www.r-project.org/). A P value of less than 0.05 was regarded as statistically significant.
Results
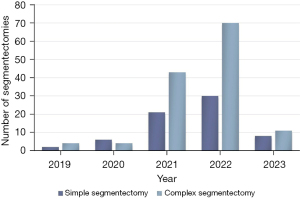
Uniportal VATS segmentectomy was performed on 199 patients, consisting of 67 simple segmentectomies and 132 complex segmentectomies (Figure 1). There were no cases where lobectomy or other extended resections were necessary due to the presence of N1 node metastasis or misidentified structures. Over the course of our study period, there was a higher number of complex segmentectomies performed compared to simple segmentectomies (Figure 5).
In uniportal VATS simple segmentectomy, S6 (superior segment) was the most frequent resected segment (16.6% of 199 patients), followed by S1+2+3 (upper division segment) in 10.6% and S4+5 (lingular segment) in 6.5%. On the other hand, in uniportal VATS complex segmentectomy, the most common resected segment was S1+2 (apico-posterior segment) in 13.1% of 199 patients, followed by S1 (apical segment) in 11.6% and S3 (anterior segment) in 10.6%. Regarding lower lobe segmentectomy, the most frequent resected segment was S8 (antero-basal segment) in 5.0% of 199 patients, followed by S10 (postero-basal segment) in 4.5%. These findings are summarized in Tables 1,2.
Table 1
| Simple segmentectomy | N (%) |
|---|---|
| S6 | 33 (16.6) |
| S1+2+3 (upper division) | 21 (10.6) |
| S4+5 (lingular) | 13 (6.5) |
VATS, video-assisted thoracoscopic surgery.
Table 2
| Complex segmentectomy | N (%) |
|---|---|
| S1 | 23 (11.6) |
| S2 | 14 (7.0) |
| S3 | 21 (10.6) |
| S5 | 1 (0.5) |
| S8 | 10 (5.0) |
| S9 | 1 (0.5) |
| S10 | 9 (4.5) |
| S1+2 | 26 (13.1) |
| S2+3 | 1 (0.5) |
| S2b+3a | 1 (0.5) |
| S7+8 | 8 (4.0) |
| S8+9 | 2 (1.0) |
| S9+10 | 4 (2.0) |
| S2+4+5 | 1 (0.5) |
| S3+4+5 | 1 (0.5) |
| S7+8+9 | 3 (1.5) |
| S3+6+7+8+9 | 1 (0.5) |
| S7+8+9+10 | 5 (2.5) |
VATS, video-assisted thoracoscopic surgery.
The demographic and baseline characteristics of the patients, as well as the tumor characteristics, are described in Table 3. The study included 67 patients (19 men and 48 women) who underwent uniportal VATS simple segmentectomy, with a median age of 52 (IQR, 44–65) years. Meanwhile, 132 patients (44 men and 88 women) underwent uniportal VATS complex segmentectomy, with a median age of 54 (IQR, 45–62) years. Of the uniportal VATS simple segmentectomy group, 16 patients (23.9%) had a current or former smoking history, while 33 patients (25.0%) in the uniportal VATS complex segmentectomy group had a current or former smoking history. There were no significant differences between the two groups regarding age, sex, smoking history, and history of malignant tumors. The study found that in the uniportal VATS simple segmentectomy group, 66 patients (98.5%) had adenocarcinoma, and only 1 patient (1.5%) had squamous cell carcinoma. All 132 patients who underwent uniportal VATS complex segmentectomy had adenocarcinoma. The most frequent subtype of adenocarcinoma was invasive adenocarcinoma (IAC), with 40 patients (60.6%) in the uniportal VATS simple segmentectomy group and 73 patients (55.3%) in the uniportal VATS complex segmentectomy group. There were no significant differences between the two groups in terms of the tumor’s histology, size on CT, subtypes, and adenocarcinoma grade.
Table 3
| Variables | Simple segmentectomy (n=67) | Complex segmentectomy (n=132) | P value |
|---|---|---|---|
| Age (years) | 52 [44–65] | 54 [45–62] | 0.788 |
| Sex | 0.581 | ||
| Male | 19 (28.4) | 44 (33.3) | |
| Female | 48 (71.6) | 88 (66.7) | |
| Smoking history | >0.99 | ||
| Current/former | 16 (23.9) | 33 (25.0) | |
| Never | 51 (76.1) | 99 (75.0) | |
| History of malignant tumors | 0.862 | ||
| Lung cancer | 1 (1.5) | 2 (1.5) | |
| Other malignancies | 10 (14.9) | 23 (17.4) | |
| Histology | 0.337 | ||
| Adenocarcinoma | 66 (98.5) | 132 (100.0) | |
| Squamous cell carcinoma | 1 (1.5) | 0 (0.0) | |
| Tumor size on CT (mm) | 11 [9–15] | 11 [8–13] | 0.386 |
| Subtype | 0.777 | ||
| AIS | 11 (16.7) | 25 (18.9) | |
| MIA | 15 (22.7) | 34 (25.8) | |
| IAC | 40 (60.6) | 73 (55.3) | |
| Adenocarcinoma grade | 0.12 | ||
| 0 | 26 (39.4) | 59 (44.7) | |
| 1 (well-differentiated) | 9 (13.6) | 25 (18.9) | |
| 2 (moderately differentiated) | 26 (39.4) | 46 (34.8) | |
| 3 (poorly differentiated) | 5 (7.6) | 2 (1.5) |
Values are presented as n (%) or median [IQR]. CT, computed tomography; AIS, adenocarcinoma in situ; MIA, minimally invasive adenocarcinoma; IAC, invasive adenocarcinoma; IQR, interquartile range.
Table 4 presents the results of operative outcomes for both simple and complex segmentectomy via uniportal VATS. The median anesthesia and operation times for simple segmentectomy were 140 (IQR, 118–170) and 105 (IQR, 87–130) min, respectively, while those for complex segmentectomy were 135 (IQR, 120–165) and 105 (IQR, 93–126) min, respectively. Both groups had similar median estimate blood loss of 50 (IQR, 50–50) mL. However, a significant difference was observed between the two groups in terms of surgical margin distance (P=0.0175), with the simple segmentectomy group having a median distance of 22 (IQR, 17–32) mm and the complex segmentectomy group having a median distance of 20 (IQR, 15–26) mm. In the simple segmentectomy group, one case (specifically, upper division segmentectomy) necessitated conversion to thoracotomy due to bleeding resulting from a tear between the left main pulmonary artery and the apicoposterior segmental branch. There were no significant differences between the two groups in terms of anesthesia time, operation time, estimated blood loss, use of ICG, conversion to thoracotomy, and presence of pleural adhesion.
Table 4
| Variables | Simple segmentectomy (n=67) | Complex segmentectomy (n=132) | P value |
|---|---|---|---|
| Anesthesia time (min) | 140 [118–170] | 135 [120–165] | 0.814 |
| Operation time (min) | 105 [87–130] | 105 [93–126] | 0.792 |
| Estimated blood loss (mL) | 50 [50–50] | 50 [50–50] | 0.972 |
| Invasive size of tumor (mm) | 7 [2–11.5] | 6 [2–9] | 0.126 |
| Surgical margin distance (mm) | 22 [17–32] | 20 [15–26] | 0.0175 |
| Use of ICG | 63 (94.0) | 131 (99.2) | 0.2177 |
| Conversion to thoracotomy | 1 (1.5) | 0 (0.0) | 0.337 |
| Pleural adhesion | 0.533 | ||
| None | 60 (89.5) | 122 (92.4) | |
| Partial | 5 (7.5) | 9 (6.8) | |
| Whole | 2 (3.0) | 1 (0.8) |
Values are presented as n (%) or median [IQR]. ICG, indocyanine green; IQR, interquartile range.
Table 5 displays the postoperative outcomes of the uniportal VATS simple and complex segmentectomy. The median duration of chest tube drainage was 1 (IQR, 1–2) days in both groups. However, there was a significant difference in duration of postoperative hospital stay between the two groups (P=0.0116), with the simple segmentectomy group having a median stay of 7 (IQR, 4.5–8) days and the complex segmentectomy group having a median stay of 6 (IQR, 4–7) days. There were seven complications after uniportal VATS segmentectomy, which included prolonged air leak, chylothorax, pneumothorax, pneumonia, and transient ischemic attack (TIA). However, there were no significant differences in the duration of chest tube drainage and incidence of complications between the two groups.
Table 5
| Variables | Simple segmentectomy (n=67) | Complex segmentectomy (n=132) | P value |
|---|---|---|---|
| Duration of chest tube drainage (days) | 1 [1–2] | 1 [1–2] | 0.0748 |
| Duration of postoperative hospital stay (days) | 7 [4.5–8] | 6 [4–7] | 0.0116 |
| Complications | 3 (4.5) | 4 (3.0) | 0.69 |
| Prolonged air leak | 1 (1.5) | 1 (0.8) | >0.99 |
| Chylothorax | 1 (1.5) | 0 (0.0) | 0.337 |
| Pneumothorax | 1 (1.5) | 1 (0.8) | >0.99 |
| Pneumonia | 0 (0.0) | 1 (0.8) | >0.99 |
| TIA | 0 (0.0) | 1 (0.8) | >0.99 |
Values are presented as n (%) or median [IQR]. TIA, transient ischemic attack; IQR, interquartile range.
Discussion
Our early surgical outcomes with the uniportal VATS complex segmentectomy have been promising, demonstrating its safety and feasibility when compared to uniportal VATS simple segmentectomy. Apart from the duration of the postoperative stay and surgical margin distances, there were no significant differences between the two groups in terms of patient and tumor characteristics, operative outcomes, and postoperative outcomes.
There is substantial literature supporting the effectiveness of anatomic segmentectomy compared to lobectomy for patients with small, peripheral NSCLC in terms of oncologic outcomes, despite the lack of randomized trials (6,11,12). In a multicenter propensity score-matched analysis conducted by Handa and colleagues, it was reported that long-term outcomes for patients undergoing complex segmentectomy were comparable to those undergoing lobectomy, with a 5-year cancer-specific survival (CSS) rate of 96% and 5-year recurrence-free interval (RFI) rate of 95.5% for complex segmentectomy, compared to a 5-year CSS rate of 97.8 and 5-year RFI rate of 95.9% for lobectomy (12). In 2022, the first phase 3 randomized trial, JCOG0802/WJOG4607L, was published and showed that segmentectomy is both non-inferior and superior to lobectomy regarding overall survival for patients diagnosed with small-sized peripheral NSCLC (3). Another phase 3 randomized trial, CALGB 140503, was published in 2023 and demonstrated that sublobar resection is not inferior to lobectomy in terms of disease-free survival for selected patients with peripheral NSCLC with a tumor size of 2 cm or less and pathologically confirmed node-negative disease in the hilar and mediastinal lymph nodes. Furthermore, both sublobar resection and lobectomy showed similar overall survival (4). The efficacy of anatomic segmentectomy over lobectomy for patients diagnosed with small, peripheral NSCLC has been established through two randomized trials. Our policy for conducting uniportal VATS segmentectomy is suitable, as we have selectively chosen patients with clinical stage 1A NSCLC and confirmed absence of lymph node involvement in the hilar and mediastinal regions through frozen section analysis.
Segmentectomy can be subdivided into two types, simple and complex, based on the number of intersegmental planes that require dissection (6). The question at hand is whether complex segmentectomy is a safe and feasible alternative to simple segmentectomy. Complex segmentectomy of the lower lobes is considered more challenging due to the deep location of vascular structures and bronchi within the lung parenchyma, as well as the prevalence of anatomical variations that increase the risk of misidentifying these structures during surgery (10). To ensure comprehensive analysis, five cases of basal segmentectomy were included within the complex segmentectomy group, instead of excluding them or creating a separate category. This approach allows for a more inclusive evaluation of complex segmentectomy procedures in our study. In addition to the higher risk of postoperative complications during complex segmentectomy, many surgeons are discouraged from performing complex segmentectomy due to concerns about increased risk of cancer recurrence and failure to achieve complete cancer control (6,10). Within our study, 43 out of 199 patients (21.6%) underwent complex segmentectomy of the lower lobe. None of these patients required conversion to lobectomy or other extended resections due to misidentification of segmental vascular structures and bronchi during the procedure.
The study we conducted showed that the patient and tumor characteristics in the simple segmentectomy group and complex segmentectomy group were comparable. There were no notable differences in age, sex, smoking history, history of malignant tumors, tumor’s histology, size on CT, subtypes, and adenocarcinoma grade. Simple segmentectomy had a median anesthesia time of 140 min and median operation time of 105 min. In comparison, surgical times for complex segmentectomy were also deemed acceptable, with a median anesthesia time of 135 min and median operation time of 105 min. In their study, Okubo and colleagues found that the operative time (113 min) for complex segmentectomy was similar to that of simple segmentectomy and that the perioperative results for complex segmentectomy were acceptable and comparable to those of simple segmentectomy. According to their findings, the complex segmentectomy group had closer surgical margins of 22 (IQR, 14–30) mm in comparison to the simple segmentectomy group, which had margins of 25 (IQR, 17–35) mm. As a result, they advised surgeons to be careful and ensure adequate surgical margins (13). We performed complex segmentectomy involving two or more segment resections in 53 out of 199 patients (26.6%) to ensure sufficient surgical margin distances. However, our study found that the median surgical margin distance for complex segmentectomy [20 (IQR, 15–26) mm] was shorter than that of simple segmentectomy [22 (IQR, 17–32) mm]. These results suggest that, similar to Okubo et al., surgeons should pay close attention to ensuring adequate surgical margins during complex segmentectomy (13). While our institution currently lacks three-dimensional reconstructed CT images, incorporating them during complex segmentectomy could be beneficial in achieving longer surgical margins by aiding in preoperative decision-making regarding the specific segments to be resected (14).
Our study revealed that both simple and complex segmentectomy had short median duration of chest tube drainage [1 (IQR, 1–2) days] and comparable incidence of complications. Interestingly, the duration of the postoperative hospital stay in our complex segmentectomy group was longer [6 (IQR, 4–7) days] than that reported by Okubo et al. [3 (IQR, 3–4) days] but similar to the results reported by Handa et al. [7 (IQR, 6–9) days] (6,13). The duration of postoperative hospital stay also exhibited a statistically significant difference between the two groups. However, we consider this finding to have limited practical significance due to several factors. Firstly, patients’ preferences to prolong their hospital stay, along with the absence of constraints on hospitalization periods within Korea’s medical insurance system, influenced the results. Furthermore, there was no statistically significant difference observed in the duration of chest tube drainage between the complex and simple segmentectomy groups, further diminishing the meaningfulness of comparing postoperative stay duration.
Our study has some limitations. Firstly, the sample size was small, as the surgeries were performed by a single surgeon in a single center. Secondly, the study was nonrandomized and retrospective in nature, which may have introduced bias in our results. Finally, we do not have long-term data, and we have yet to report on disease-free survival and recurrence-free survival.
Conclusions
Based on our study, we concluded that uniportal VATS complex segmentectomy is a viable and safe alternative for patients with clinical stage 1A NSCLC, with early surgical outcomes similar to uniportal VATS simple segmentectomy. We found no significant differences in patient and tumor characteristics, operative outcomes, and postoperative outcomes between the two groups, except for the surgical margin distances. It is vital to acknowledge that a short resection margin is probable in complex segmentectomy cases. Thus, when conducting uniportal VATS complex segmentectomy, careful evaluation of the tumor location is essential.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-627/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-627/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-627/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-627/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Institutional Review Board of the Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea (No. PC23RASI0062), which did not require individual consent for this retrospective study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 622-3. [Crossref] [PubMed]
- CAHAN WG. Radical lobectomy. J Thorac Cardiovasc Surg 1960;39:555-72.
- Saji H, Okada M, Tsuboi M, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet 2022;399:1607-17. [Crossref] [PubMed]
- Altorki N, Wang X, Kozono D, et al. Lobar or Sublobar Resection for Peripheral Stage IA Non-Small-Cell Lung Cancer. N Engl J Med 2023;388:489-98. [Crossref] [PubMed]
- National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [Crossref] [PubMed]
- Handa Y, Tsutani Y, Mimae T, et al. Complex segmentectomy in the treatment of stage IA non-small-cell lung cancer. Eur J Cardiothorac Surg 2020;57:114-21. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Hernandez-Arenas LA, Purmessur RD, Gonzalez-Rivas D. Uniportal video-assisted thoracoscopic segmentectomy. J Thorac Dis 2018;10:S1205-14. [Crossref] [PubMed]
- Karenovics W, Gonzalez M. How to decrease technical obstacles to difficult video-assisted thoracoscopic surgery segmentectomy? J Thorac Dis 2019;11:53-6. [Crossref] [PubMed]
- Schuchert MJ, Pettiford BL, Keeley S, et al. Anatomic segmentectomy in the treatment of stage I non-small cell lung cancer. Ann Thorac Surg 2007;84:926-32; discussion 932-3. [Crossref] [PubMed]
- Handa Y, Tsutani Y, Mimae T, et al. Oncologic Outcomes of Complex Segmentectomy: A Multicenter Propensity Score-Matched Analysis. Ann Thorac Surg 2021;111:1044-51. [Crossref] [PubMed]
- Okubo Y, Yoshida Y, Yotsukura M, et al. Complex segmentectomy is not a complex procedure relative to simple segmentectomy. Eur J Cardiothorac Surg 2021;61:100-7. [Crossref] [PubMed]
- Wang X, Wang Q, Zhang X, et al. Application of three-dimensional (3D) reconstruction in the treatment of video-assisted thoracoscopic complex segmentectomy of the lower lung lobe: A retrospective study. Front Surg 2022;9:968199. [Crossref] [PubMed]



