A 30-year-old female Behçet’s disease patient with recurrent pleural and pericardial effusion and elevated adenosine deaminase levels: case report
Introduction
Behçet’s disease is a chronic relapsing vasculitis involving multisystem in the body, characterized by endothelial dysfunction, neutrophil hyperfunction and reactive oxygen species overproduction, known to be associated with a genetic predisposition, such as carrying the HLA-B51 gene and certain microorganisms (1-5). Recurrent oral and genital ulceration with uveitis represents the clinical triad (6). Various cardiovascular, pulmonary and neurological organs can be involved as a form of vasculitis, in addition to the joints and gastrointestinal system (3).
Pulmonary manifestations in Behçet’s disease are seen in <10% of patients. Common respiratory symptoms include hemoptysis, dyspnea, pleuritic chest pain, and cough (4,7,8). The disease can involve almost all of the anatomic structures in the thorax and various-sized vessels, lung parenchyma, mediastinum, and pleura may be observed (7,8). Pulmonary artery aneurysms and hemoptysis occur most frequently in patients with Behçet’s disease, a condition that is associated with poor prognosis (4,8). Pleural effusion is an uncommon manifestation that may result mostly from the secondary findings of superior vena cava (SVC) syndrome or pulmonary infarction. A few case reports have indicated pleural effusion due to primary vasculitis of the pleura (6). Cardiovascular involvement, including coronary artery disease, pericarditis, myocarditis, endocarditis, arrhythmia and valvular dysfunction, have been reported in <10% of patients with Behçet’s disease (9-11). Pericardial involvement, a common cardiac manifestation with up to 40% cardiac involvement, may be associated with vasculitis of the pericardium or SVC thrombosis (6,10).
The main pathologic characteristic of Behçet’s disease is nonspecific vasculitis of small-to-large-sized vessels in both the systemic and pulmonary circulation, with perivascular infiltration of lymphocytes and mononuclear cells (12). Vasculitis mostly affects veins and accounts for approximately 85% of the vascular involvement (3). Endothelial cell swelling, fibrinoid necrosis and thrombus formation within the vessel lumen are common in inflammation foci (5,8).
Anti-inflammatory and immunosuppressive drugs represent the mainstay treatments for Behçet’s disease (7,8). However, the choice of treatment varies depending on the type of organ involved, the disease severity, and even the clinician who treats the patient (9,13). Corticosteroids with or without anticoagulation have been used in cases of Behçet’s disease with pulmonary involvement, but no consensus has been reached regarding the treatment of choice, particularly for patients with pleural effusion alone (7,8). When there is pericardial involvement, colchicine and immunosuppressive agents are useful, and pericardiectomy should be considered for medically unresponsive cases (14).
We report a patient with Behçet’s disease presented with recurrent pleural and pericardial effusion and elevated adenosine deaminase (ADA) levels.
Case presentation
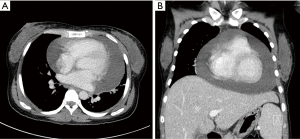
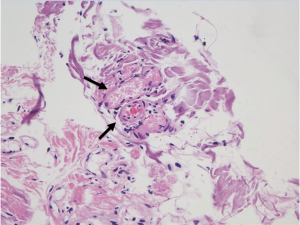
A 30-year-old Asian woman visited our clinic complaining of left pleuritic chest pain for seven days. She had associated symptoms of fever, cough, and sputum. The patient was diagnosed with Behçet’s disease two years prior and had been medicated with 15 mg of prednisolone at our rheumatology department. Sixteen months ago, she was admitted due to pericardial effusion with small pleural effusion. She had undergone pericardiocentesis, and analysis of pericardial fluid revealed a white blood cell (WBC) count of 1,000 cells/µL (lymphocytes, 37%) with an ADA level of 226.7 IU/L. We had not performed pleural drainage because of its low content. Interferon-gamma release assay (IGRA) from plasma revealed a negative result. One year previously, she had been admitted to the emergency department due to fever, dyspnea, and palpitation with unstable vital sign- blood pressure, 90/60 mmHg and heart rate, 150/min. Chest computed tomography (CT) again revealed marked pericardial effusion, suggesting cardiac tamponade (Figure 1). Next, she underwent a pericardial window operation. The analysis in the pericardial fluid was similar with the previous study. The results of acid-fast bacilli (AFB) culture and polymerase chain reaction (PCR) for mycobacterial tuberculosis (M.TB) were negative in the tissue, with histologic findings of mild endothelitis with micro-thrombi formation in the lumen (Figure 2). Because the vessel changes were non-specific and too subtle for a specific diagnosis, we suspected TB pericarditis and started standard antituberculous medication and high-dose steroid therapy (1 mg/kg, prednisolone). After 8 months, there was a marked increase in left pleural effusion on chest X-ray, and pleural drainage was complete. The effusion analysis revealed a WBC count of 360 cells/µL with a lymphocyte percentage of 54% and an ADA level of 158.5 IU/L. Microbiologic results for M.TB were all negative in the pleural fluid. The patient was maintained on the antituberculous medication for one year, which was discontinued three weeks before the current admission. She was a nonsmoker and had no familial history of connective tissue disease or pulmonary disease.
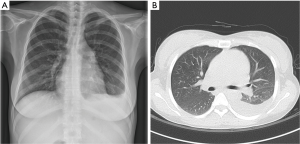
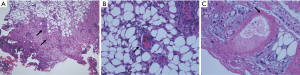
On physical examination, her body temperature was 38.1 ℃; blood pressure was 100/60 mmHg, heart rate was 125 beats/min, respiratory rate was 18 cycles/min, and O2 saturation was 98% by oximetry in the atmosphere. Breathing sounds were diminished at left lower lung fields without rale or wheezing. The laboratory findings showed a WBC count of 2,680/mm3, a hemoglobin value of 9.9 g/dL, and a platelet count of 170,000/mm3. The C-reactive protein level was 0.38 mg/dL, and the AST/ALT level was 58/39 U/L. Electrolyte and creatinine levels were normal. Chest X-ray showed left pleural effusion (Figure 3A). Chest CT showed left pleural effusion and mild cardiomegaly, but there was no other significant lesion such as lung parenchymal infiltration (Figure 3B). Percutaneous catheter drainage was performed, and pleural fluid analysis revealed a protein level of 4.66 g/dL (serum 6.8 g/dL), a glucose level of 85 mg/dL, an albumin level of 2.81 g/dL (serum 3.4 g/dL), and an LDH level of 676 U/L (serum 772 U/L). Her WBC count was 880/µL and differential count showed a lymphocyte percentage of 60% with ADA level, 146.5 IU/L. Bronchoscopic findings were no endobronchial lesion with AFB staining and TB PCR-negative. Anti-nuclear antibody in serum was positive (titer 1:100), and anti-neutrophil cytoplasmic antibody was negative. IGRA was negative in the plasma, and the serum ADA level was 236.2 IU/L. The results of all of the pleural and pericardial effusion analyses are shown in Table 1. To obtain a definite diagnosis of recurrent pleural effusion, video-assisted thoracoscopic pleural biopsy was performed. Microscopic examination of the pleural specimen showed inflammatory cell infiltration and fibrosis in pleural tissue and endothelitis in small rather than large vessels, with some thrombus formation (Figure 4A-C). We confirmed the diagnosis as pleuropericardial involvement of Behçet’s disease and maintained steroid therapy in the out-patient department.
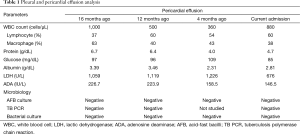
Full table
Discussion
In the endemic area, a high ADA level with lympho-dominant exudate is considered to be the most clear indication for the diagnosis of TB pleurisy and pericarditis (15,16). In our case, the patient was assumed to have TB pericarditis and pleurisy due to lympho-dominant exudate with a high ADA level on effusion analysis. Although she had a negative result of IGRA, the negative predictive value of the test of peripheral blood is known to be relatively low in the diagnosis of TB pleurisy (17). Regarding the relationship between ADA and Behçet’s disease, several studies have shown that plasma ADA levels are increased in patients with Behçet’s disease, and are also associated with disease activity (13,18). As the T-cell immune response is considered to play an important role in the pathogenesis of the disease, ADA, a non-specific marker of T-cell activation, might be elevated, particularly during the disease’s active stage. In our patient, the serum ADA level was high at 236.2 IU/L, assuming that the underlying Behçet’s disease was still active.
In the current case, histologic findings in the pleura showed vasculitis of the small vessels with thrombus formations in vessel lumens, consistent with the involvement of Behçet’s disease. Furthermore, retrospective review revealed that the vascular changes at the pericardium, such as endothelitis with micro-thrombi formation, suggested the pericardial involvement of Behçet’s disease. There were no granulomatous lesions or other findings indicating other conditions such as tuberculosis. Pleural effusion usually occurs secondary to pulmonary infarction or an infectious condition in Behçet’s disease (12). There have been few case reports in which the effusion was attributed to vasculitis of the pleura (19). Moreover, to the best of our knowledge, it is extremely rare that vasculitis involves both the pericardium and pleura simultaneously in patients with Behçet’s disease, per our case.
Conclusions
Clinicians should consider that Behçet’s disease may manifest as pleural or pericardial effusion with lympho-dominant exudate and high ADA level, which mimics TB pleurisy or pericarditis. Pathologic confirmation could be helpful for the definite diagnosis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Erkiliç K, Evereklioglu C, Cekmen M, et al. Adenosine deaminase enzyme activity is increased and negatively correlates with catalase, superoxide dismutase and glutathione peroxidase in patients with Behçet's disease: original contributions/clinical and laboratory investigations. Mediators Inflamm 2003;12:107-16. [Crossref] [PubMed]
- Calis M, Ates F, Yazici C, et al. Adenosine deaminase enzyme levels, their relation with disease activity, and the effect of colchicine on adenosine deaminase levels in patients with Behçet's disease. Rheumatol Int 2005;25:452-6. [Crossref] [PubMed]
- Ceylan N, Bayraktaroglu S, Erturk SM, et al. Pulmonary and vascular manifestations of Behcet disease: imaging findings. AJR Am J Roentgenol 2010;194:W158-64. [Crossref] [PubMed]
- Chae EJ, Do KH, Seo JB, et al. Radiologic and clinical findings of Behçet disease: comprehensive review of multisystemic involvement. Radiographics 2008;28:e31. [Crossref] [PubMed]
- Verity DH, Wallace GR, Vaughan RW, et al. Behçet's disease: from Hippocrates to the third millennium. Br J Ophthalmol 2003;87:1175-83. [Crossref] [PubMed]
- Hiller N, Lieberman S, Chajek-Shaul T, et al. Thoracic manifestations of Behçet disease at CT. Radiographics 2004;24:801-8. [Crossref] [PubMed]
- Erkan F, Cavdar T. Pulmonary vasculitis in Behçet's disease. Am Rev Respir Dis 1992;146:232-9. [Crossref] [PubMed]
- Erkan F, Gül A, Tasali E. Pulmonary manifestations of Behçet's disease. Thorax 2001;56:572-8. [Crossref] [PubMed]
- Ambrose NL, Haskard DO. Differential diagnosis and management of Behçet syndrome. Nat Rev Rheumatol 2013;9:79-89. [Crossref] [PubMed]
- Geri G, Wechsler B. Spectrum of cardiac lesions in Behçet disease: a series of 52 patients and review of the literature. Medicine (Baltimore) 2012;91:25-34. [Crossref] [PubMed]
- Mirone L, Altomonte L, Ferlisi EM, et al. Behçet's disease and cardiac arrhythmia. Clin Rheumatol 1997;16:99-100. [Crossref] [PubMed]
- Tunaci A, Berkmen YM, Gökmen E. Thoracic involvement in Behçet's disease: pathologic, clinical, and imaging features. AJR Am J Roentgenol 1995;164:51-6. [Crossref] [PubMed]
- Yazici H, Yurdakul S, Hamuryudan V. Behçet disease. Curr Opin Rheumatol 2001;13:18-22. [Crossref] [PubMed]
- Sezen Y, Buyukhatipoglu H, Kucukdurmaz Z, et al. Cardiovascular involvement in Behçet's disease. Clin Rheumatol 2010;29:7-12. [Crossref] [PubMed]
- Porcel JM. Tuberculous pleural effusion. Lung 2009;187:263-70. [Crossref] [PubMed]
- Mayosi BM, Burgess LJ, Doubell AF. Tuberculous pericarditis. Circulation 2005;112:3608-16. [Crossref] [PubMed]
- Ates G, Yildiz T, Ortakoylu MG, et al. Adapted T cell interferon-gamma release assay for the diagnosis of pleural tuberculosis. Respiration 2011;82:351-7. [Crossref] [PubMed]
- Mesquida M, Molins B, Llorenç V, et al. Proinflammatory cytokines and C-reactive protein in uveitis associated with Behçet's disease. Mediators Inflamm 2014;2014:396204.
- Oz N, Sarper A, Erdoğan A, et al. Video-assisted thoracic surgery for the management of pleural and pericardial effusion in Behçet's syndrome. Tex Heart Inst J 2000;27:304-6. [PubMed]


