Urgent pulmonary lobectomy for blunt chest trauma: report of three cases without mortality
Introduction
In the European Union, trauma is the most frequent cause of death in the population between 15 and 45 years (1). It is estimated that about 25% of traumatic deaths are secondary to thoracic injuries (2) and blunt chest trauma is associated with a higher mortality rate than penetrating chest injuries (3-5).
Generally patients with severe chest injuries are treated with supportive measures and only a minority of these patients need urgent thoracotomy (5-8). According to the “damage control” strategy, pneumonorrhaphy and tractotomy are treatments of choice (9-11); pulmonary resections, including wedge resection, lobectomy and pnemonectomy, are necessary in selected cases (6,8,12). Currently, the survival of patients that underwent major lung resections performed for thoracic trauma is very low and the mortality rate associated with lobectomy reaches 60% (4,5).
We report three cases of urgent thoracotomies with inferior lung lobectomies for blunt chest trauma without mortality and with postoperative complete restoration of respiratory function.
Methods
Over a 2-year period [2013–2014], 210 patients with chest trauma were hospitalized at Manzoni Hospital-Lecco: 158 (75.2%) in the Department of Surgery and 52 (24.8%) in the Intensive Care Unit. Mean age was 42.3 years (range: 3–84); 176 (83.8%) patients were males and 34 (16.2%) females. Mechanism of injury was blunt in 204 (97.1%) patients while penetrating in 6 (2.9%). In 42 (20%) cases, there were concomitant extrathoracic lesions. In 48 (22.8%) patients was necessary a ventilatory support and 37 (17.6%) patients were treated with thoracostomy tube. Nineteen (9%) patients needed urgent thoracotomy: 4 (1.9%) cases for penetrating injury and 15 (7.1%) cases for blunt trauma. In the blunt group 5 pneumonorrhaphies, 5 wedge resections, 3 lobectomies, and 2 rib fixings with concomitant hematoma evacuation were performed; in the penetrating group 2 myocardial wound repairs and 2 tractotomy were performed. Three (1.4%) patients treated with urgent thoracotomy required concomitant laparotomy for intra-abdominal injuries. The mortality rate was 1.4% (3 patients): 2 (0.9%) patients with penetrating myocardial wounds and 1 (0.5%) patient with associated abdominal trauma. We describe the clinical course of 3 female patients treated with anatomical pulmonary lobectomies. All patients gave written consent for the publication of personal data.
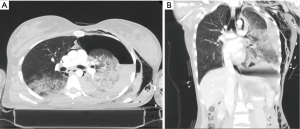
Patient 1
A 28-year-old woman was admitted to Emergency Department for severe car crash. Chest X-rays and thoraco-abdominal computed tomography (CT) scan showed multiple left ribs fractures, left hemo-pneumothorax and multiple lung contusion areas (Figure 1). A spleen laceration of grade 2 according to American Association for the Surgery of Trauma (AAST) and left humeral fracture were also found. The Injury Severity Score (ISS) was 29. Patient underwent chest tube insertion with blood (1,500 mL) and air output. Severe haemoptysis followed by a fast onset of hemorrhagic shock and cardiac arrest required emergent anterolateral thoracotomy with a single-lumen endotracheal tube. Left inferior bronchial disruption needed inferior lung lobectomy and thoracoplasty for repair multiple rib fractures. Operative time was 160 minutes. Splenic laceration was non-operatively managed. Endotracheal tube was removed 30 days after surgery. After 43 days the patient was shifted from Intensive Care Unit to Surgery Department and discharged from the hospital on the 58th post-operative day.
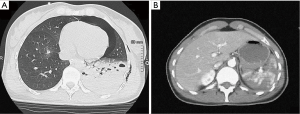
Patient 2
A 35-year-old woman was admitted for a thoraco-abdominal trauma after a motor cycle crash. Thoraco-abdominal CT scan revealed an AAST grade 4 spleen laceration with hemoperitoneum and left hemo-pneumothorax associated with left lung hematoma (ISS =26) (Figure 2). Patient underwent emergent splenectomy and left chest tube insertion with blood (800 mL) and air output. Four hours after surgery the patient developed a hypovolemic shock. A following CT scan revealed an expanding left lung hematoma with hemothorax requiring urgent posterolateral thoracotomy with double lumen intubation; a left lung inferior lobectomy was performed. Operative time was 168 minutes. Postoperative course was uneventful; endotracheal tube was removed in 2nd postoperative day. The patient was discharged on 13th post-operative day.
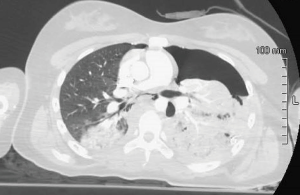
Patient 3
A 14-year-old woman attempted suicide falling from a height of six meters. Total body CT scan demonstrated left hemo-pneumothorax caused by several lung lacerations and right lung contusions (Figure 3). Moreover the patient had AAST grade 2 splenic laceration, two uncomplicated lumbar transverse process fractures and bilateral feet fractures (ISS =43). A chest tube was inserted and 1,000 mL of blood were drained. Hypovolemic shock required prompt surgical intervention. A posterolateral thoracotomy was performed after the placement of a double lumen tube. An inferior lobectomy for a deep lung laceration involving hilum and a pneumonorrhaphy for superior lobe laceration were carried out. Operative time was 165 minutes. Splenic laceration and lumbar spine fractures were non-operatively managed, while feet fractures required delayed several surgical operations. Patient maintained endotracheal intubation for 13 days. She was discharged from Intensive Care Unit on 16th postoperative day and from the hospital on 68th postoperative day.
No post-operative complications were observed. Spirometry performed four months after surgery demonstrated no functional deficit with complete recovery of respiratory function in each patient.
Discussion
The majority of patients with blunt chest trauma are managed non-operatively by supportive measures and tube thoracostomy; thoracotomy is required in only 7–10% of cases (5-8).
The “damage control” strategy has been applied also to lung injuries: simple and rapid surgical treatments not involving pulmonary tissue resection have been developed for reducing operative times and decreasing blood loss in patients with metabolic damage (9-13). Consequently, pneumonorrhaphy and tractotomy are the surgical techniques preferred in chest trauma (7,9). Pulmonary resections are needed in 17% of patients that underwent urgent thoracotomy for blunt chest trauma and range from wedge resection to pneumonectomy (5). In case of extensive injuries involving major hilar vessels or bronchi, an anatomic pulmonary resection is necessary (6,8).
In our series 3 anatomic lobectomies were performed for massive hemothorax with bronchial disruption and consequent cardio-circulatory arrest (case 1), quickly expanding pulmonary hematoma with hypovolemic shock (case 2), and massive hemothorax due to a deep parenchymal laceration involving lung hilum (case 3).
Overall mortality rate after major pulmonary resections for trauma is very high and increases with the presence of multivisceral injuries, the severity of hypovolemic shock and the extent of lung resection (4,5,7,12). In multicenter series, the mortality associated with lobectomy ranges from 35% to 43% and in case of pneumonectomy varies from 50% to 62% (4,5). The low survival rate associated with major lung resections may be partly explained by the frequent association with extrathoracic multivisceral injuries (5). However the multivariate analysis of two large multicenter series demonstrated that the extent of lung resection is an independent predictive factor for intrahospital mortality in patients with thoracic trauma (4,5).
Early diagnosis and consequent specific interventions are fundamental issues in traumatic injury of the lung (14). CT scan plays a key role in the management of chest trauma and it has a considerable impact on the following therapeutic decisions (14). The introduction in the clinical practice of multidetector CT allows rapid and complete definition of all lesions in polytrauma patients (15). Multidetector CT scan can be performed right after the primary survey without any complications and it can be repeated subsequently if the patient’s conditions are worsening (14,15).
The delay of the surgical treatment is one of the most important factors influencing negatively the outcome of these patients (3,8). Hypovolemic shock, massive hemothorax with chest tube output greater than 1,500 mL and not controlled airway leak are the standard indications for urgent thoracotomy in blunt chest trauma (3,6-8). For reducing mortality, some authors suggest to perform urgent thoracotomy when the output of thoracostomy tube reaches 1,000 mL (8). In patients with massive hemothorax for blunt chest trauma, the surgical hemostasis must to be achieved quickly: pneumonorrhaphies and wedge resections are preferred but if more conservative interventions do not control hemorrhage, anatomical lobectomy must be performed without delay (6,8). The duration of surgery seems to influence the outcome of patients with lung injuries (16). In a series the mean operative time of conservative treatments (tractotomy) was 2.3 hours, while the mean operative time of anatomic resections (lobectomies and pneumonectomies) was 4.7 hours (7): the disparity of mortality between conservative and non-conservative lung resections for traumatic lesions may be related to the difference in the length of surgery.
In our series the operative time was shorter (2.7 hours) compared to that present in the literature: lobectomies were carried out by two expert thoracic surgeons (GV, MC) of our surgical team that routinely perform elective pulmonary surgery.
In chest trauma anterolateral thoracotomy in the supine position is the more frequently used approach because it permits a fast access to the contralateral hemithorax with a clamshell incision (11,12). Posterolateral thoracotomy is employed in stable patients with injuries localized to one hemithorax: this incision permits a wide exposure of the hilum and the inferior lobe (6,8,12). In unstable patients it is preferable to intubate with a single-lumen endotracheal tube while in relatively stable patient a double lumen intubation allows selective pulmonary exclusion (6,8,12).
We used posterolateral incision with a double lumen intubation in relatively stable patients (patient 2 and patient 3) with preoperative CT negative for contralateral thoracic injuries: the wide surgical field allowed us to perform a rapid assessment of traumatic injuries and a timely operative hemostasis.
The present series is too small to draw any definitive conclusions. Major lung resections are performed rarely in chest trauma but are associated with a high mortality directly related to the extent of resection and extra-thoracic injuries. A fast diagnosis and timely intervention are the keys to success in trauma patients. No major morbidity, including complete functional respiratory recovery, reflects the young age of our patients and intensive postoperative rehabilitation. The absence of mortality in this series may be related to prompt diagnosis, short operative time, and absence of associated severe neurological or abdominal injuries.
Acknowledgements
We thank Dr. Gerardo Cioffi, native speaker, for reviewing the English language.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Heatlh Statistics. Atlas on mortality in the European Union; Chapter 5 – part 1: Mortality by age. Luxemburg: Office of Official Publications of the European Communities, 2003.
- Khandhar SJ, Johnson SB, Calhoon JH. Overview of thoracic trauma in the United States. Thorac Surg Clin 2007;17:1-9. [Crossref] [PubMed]
- Karmy-Jones R, Jurkovich GJ, Nathens AB, et al. Timing of urgent thoracotomy for hemorrhage after trauma: a multicenter study. Arch Surg 2001;136:513-8. [Crossref] [PubMed]
- Martin MJ, McDonald JM, Mullenix PS, et al. Operative management and outcomes of traumatic lung resection. J Am Coll Surg 2006;203:336-44. [Crossref] [PubMed]
- Karmy-Jones R, Jurkovich GJ, Shatz DV, et al. Management of traumatic lung injury: a Western Trauma Association Multicenter review. J Trauma 2001;51:1049-53. [Crossref] [PubMed]
- Stewart KC, Urschel JD, Nakai SS, et al. Pulmonary resection for lung trauma. Ann Thorac Surg 1997;63:1587-8. [Crossref] [PubMed]
- Cothren C, Moore EE, Biffl WL, et al. Lung-sparing techniques are associated with improved outcome compared with anatomic resection for severe lung injuries. J Trauma 2002;53:483-7. [Crossref] [PubMed]
- Nishiumi N, Inokuchi S, Oiwa K, et al. Diagnosis and treatment of deep pulmonary laceration with intrathoracic hemorrhage from blunt trauma. Ann Thorac Surg 2010;89:232-8. [Crossref] [PubMed]
- Velmahos GC, Baker C, Demetriades D, et al. Lung-sparing surgery after penetrating trauma using tractotomy, partial lobectomy, and pneumonorrhaphy. Arch Surg 1999;134:186-9. [Crossref] [PubMed]
- Rotondo MF, Bard MR. Damage control surgery for thoracic injuries. Injury 2004;35:649-54. [Crossref] [PubMed]
- Wall MJ, Soltero E. Damage control for thoracic injuries. Surg Clin North Am 1997;77:863-78. [Crossref] [PubMed]
- Huh J, Wall MJ, Estrera AL, et al. Surgical management of traumatic pulmonary injury. Am J Surg 2003;186:620-4. [Crossref] [PubMed]
- Wall MJ, Hirshberg A, Mattox KL. Pulmonary tractotomy with selective vascular ligation for penetrating injuries to the lung. Am J Surg 1994;168:665-9. [Crossref] [PubMed]
- Trupka A, Waydhas C, Hallfeldt KK, et al. Value of thoracic computed tomography in the first assessment of severely injured patients with blunt chest trauma: results of a prospective study. J Trauma 1997;43:405-11; discussion 411-2. [Crossref] [PubMed]
- Peters S, Nicolas V, Heyer CM. Multidetector computed tomography-spectrum of blunt chest wall and lung injuries in polytraumatized patients. Clin Radiol 2010;65:333-8. [Crossref] [PubMed]
- Gasparri M, Karmy-Jones R, Kralovich KA, et al. Pulmonary tractotomy versus lung resection: viable options in penetrating lung injury. J Trauma 2001;51:1092-5; discussion 1096-7. [Crossref] [PubMed]


