Clinical outcomes of infrarenal abdominal aortic aneurysms that underwent endovascular repair in a district general hospital
Introduction
Since the first endovascular repair of an abdominal aortic aneurysm (AAA) in 1991, a less invasive method than traditional open repair has become the preferred choice for AAA repair worldwide (1,2). Minimally invasive endovascular aneurysm repair (EVAR) has lower perioperative mortality and morbidity than open surgical repair reported in randomized trials (3). Since 2010, Taiwan’s National Health Insurance has paid for EVAR, and therefore, most elective AAA repairs in Taiwan use EVAR.
Ruptured abdominal aortic aneurysms (rAAA) are catastrophic; the rAAA mortality rate may be as high as 80–85% (4). Immediate diagnosis and rapid treatment are critical. Despite advances in surgery and endovascular repair, the mortality rate for rAAA surgery is as high as 30–50% (4,5). Emergency EVAR is an alternative in patients with rAAA (5). The minimally invasive nature of this technique allows aneurysm repair in patients with a rAAA who would be at significant risk for open surgery (5).
In this study, we reviewed recent EVAR results for infrarenal AAA patients with or without a rupture in a district general hospital. The use of Perclose ProGlide® for selected cases was also analyzed. Use of EVAR could be a viable alternative in patients suffering AAA with or without a rupture.
Methods
Patient demographics
This study was evaluated and approved by the institutional review board at our hospital. A retrospective observational clinical review was conducted using data on 16 elective AAA patients and 9 consecutive ruptured AAA patients treated with EVAR from January 2010 to December 2014 in the vascular surgery department of a district general hospital in Taiwan. Patients with thoracic aneurysms and aortic dissections who received open surgery were excluded. We included all patients hospitalized for acute presentation indicating a symptomatic abdominal aortic aneurysm. These data also revealed the history of the patient’s medical contacts before and after the AAA hospitalization episode, for example, outpatient visits or hospitalization for other reasons. The device type was collected from operative reports and device entry forms. The Gore Excluder low permeability (GORE® EXCLUDER® AAA Endoprosthesis) device was used. Patients presenting with ruptured aneurysms determined using the preoperative computer tomography (CT) scan were categorized as “emergent” EVAR. All other EVAR procedures were categorized as “elective”. Perclose ProGlide® used for selected cases (6). Postoperative regular follow-up included CT scan or abdominal sonography for cases with poor renal function and regular clinical follow-up.
Statistical analysis
All statistical analyses were performed using PASW for Windows, Version 17.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are reported as the mean ± standard deviation (SD). Continuous variables were compared using a Student t-test, and discrete variables were compared using a chi-square or Fischer exact test.
Results
Preoperative and postoperative risks
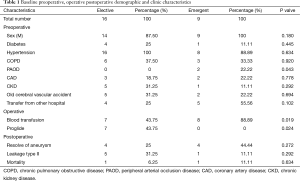
The preoperative characteristics of the two groups are listed in Tables 1 and 2. The analysis identified 25 patients, of whom 16 were in the elective category [14 men (87.50%), 76.06 (±7.59) y] and 9 were in the emergent category [9 men (100%), 73.67 (±13.03) y]; these patients had comparable baseline characteristics. Table 1 presents the concomitant diseases of the patients of elective and emergent categories: diabetes mellitus: 25% and 11.11%; hypertension: 100% and 88.89%; chronic obstructive pulmonary disease: 37.50% and 33.33%; peripheral arterial occlusion disease: 0% and 22.22%, respectively. No significant difference was found in preoperative risk.
Full table
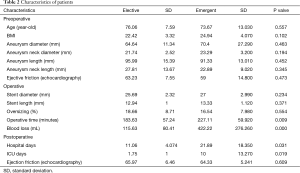
Bifurcated devices were used in 100% of patients, without the receiving aortouniiliac devices with femoral-femoral bypass. The median length of intensive care unit stay among elective EVAR cases was shorter than that for emergent EVAR cases (1.75±1 d elective vs. 10±13.37 d; P<0.019); hospital days (11.06±4.07 d elective vs. 21.89±18.36 d emergent; P<0.031); operative time (183.63±57.24 min elective vs. 227.11±59.92 min emergent; P<0.009); blood loss (115.63±80.41 mL elective vs. 422.22±276.26 mL emergent; P<0.005) as described in Table 2; When the patients have no calcification of common femoral artery, the use of Perclose ProGlide® (7 cases elective vs. 0 case emergent; P<0.024) is described in Table 1. Documented follow-ups were available for 100% of patients throughout the study period. Of the 25 patients, 9 (36%) had transferred from other hospitals without vascular service. The proportion of rAAA cases transferred from other hospitals was (5/9) 55.5% and the mortality was (1/9) 11.1%.
Full table
The overall 30-d mortality rate was 11.11% (1/9) in the emergent group. This patient died directly after defecation on the first day after surgery, most likely because of exsanguination. One case of mortality in elective group was caused by pneumonia with sepsis 1 year after the operation and was not an aneurysm-related mortality.
Discussion
Since the first endovascular repair of an AAA in 1991, EVAR has become the preferred choice for AAA repair worldwide because it is a less invasive method than traditional open repair (1,2). Scholarly articles report that the population most likely to show decreased incidence of AAA are those who might have benefited most from lower smoking rates and increased overall penetrance of statins (1,3,7). However, it is crucial to consider, first, that the use of endovascular repair for rAAA increased from 13% in 2002 to 73% in 2013; and second, that the demographic trend has been moving toward an increasing incidence and prevalence of cardiovascular disease in elderly men (4,8). In some reports, the mean age was 70–75 years, with over 78–90% of the patients being men (7,9-11). Although rAAAs are more common in male patients, rAAAs in female patients are accompanied by more advanced atherosclerotic processes and more severe cardiovascular disorders (9). In our report, the mean age of elective EVAR was 76.06 years, and the mean age of emergent EVAR was 73.67 years. The mean age was older than that of previous reports, and an age >80 years was a significant predictor of death for EVAR (10). The older group had larger aneurysms and more tortuous anatomy and more calcification of intima (10). EVAR has expanded access to repair because ruptures may have been prevented, particularly for oldest patients, and life expectancy may have been prolonged meaningfully (3). These patients in previous studies were older men and had higher rates of hypertension and COPD; they were more likely to undergo elective EVAR rather than emergent EVAR and were comparable with the patients in our present report (7,8,12). A history of hypertension strongly predicted survival of EVAR (8,13). Thus, control of blood pressure is still the most critical determinant of patient incidences.
Inevitably, this raises the question of whether patients should be transferred to an AAA treatment center. Our current practice indicates that many patients with a clinical diagnosis of a rupture are transferred from smaller hospitals and are increasingly managed in vascular units. A previous report showed that 59% were transferred from an outside facility and 41% were direct admissions (8). In our study, 36% (9/25) of patients were transferred from local hospitals without surgical service to our hospital. Among our patients with rAAA, 55.5% (5/9) were transferred from other hospitals and mortality was 11.1% (1/9). The transfer rate was lower than might have been expected from reports, because our hospital is a district general hospital. An earlier study indicated that patients were more likely to be offered a repair if they were transferred to a major teaching hospital than to a district general hospital (14). The mean time interval from initial patient transfer to arrival at the vascular service hospital was 1.2 h (8). This led to speculation that there were no differences of transportation distance between hospitals, so that only the fittest patients were still operable upon arrival at hospital.
According to the available literature, the survival of rAAA patients is highly correlated with mean arterial blood pressure (9,14-16). When rAAA patients arrive at the emergency department, to optimize outcomes, permission should be given if hypotension is suggested (target systolic blood pressure 70–80 mmHg) (14-16). These data do not provide definitive guidance on the optimal systolic blood pressure in patients with rAAA during the preoperative phase, but may suggest that the previously recommended threshold of 70 mmHg is too low, particularly for older patients with other cardiovascular diseases and high cardiovascular resistance (16). The lowest systolic blood pressure was strongly and independently associated with 30-d mortality (16). Hemodynamically unstable patients had a 21.7–40% chance of requiring aortic occlusion balloons during the procedures (8,15,17).
Two previous reports demonstrated the safety of deferring AAA repair until the diameter reaches 5.0 cm (3,10). There was no statistically significant difference between the diameters of AAA cases and rAAA cases, but with rAAA, the mean aneurysm diameter was 6 cm or shorter at the time of the rupture (12,16,18). A rupture is nearly always fatal without aneurysm repair. In our elective group, the mean aneurysm diameter was 6.46 cm and in our emergent group, the mean aneurysm diameter was 7.04 cm. The mean aneurysm diameter for AAA was shorter than the mean for rAAA, but this was not statistically significant. Table 2 shows that compared with the emergent group, the elective group had significantly (P<0.005) more favorable results for median length of intensive care unit stay, hospital days, operative time, and blood loss. When compared to open repair, EVAR also had shorter procedure times, less blood loss, fewer intensive care unit days, and shorter lengths of stay (10). Any blood loss exceeding 2,000 mL is considered an independent factor increasing the risk of perioperative death caused by hemorrhagic shock and its sequelae (9). Using Perclose ProGlide® for selective cases reduced blood loss and operative time. Results from a contemporary EVAR registry in our hospital demonstrated favorable perioperative outcomes and excellent clinical efficacy. The median length of stay was 11 d in the EVAR group, which was the same as that in our study (9,19). The mean of procedures was 163 min, which was less than 183.63 min for our study (9).
In view of the still poor results of open surgery, some authors believe that endovascular interventions will likely become the gold standard for the treatment of ruptured aortas (11). However, we believe that patient selection plays such a crucial role that one cannot compare both techniques properly. Anatomical suitability is crucial for endovascular intervention, and it is determined by CT according to guidelines for elective EVAR. Particular studies have reported perioperative mortalities of 1.2–12%, a 3% late aneurysm-related mortality, and a discouraging 66% overall survival at 5 y (1,3,19). In all cases, but especially in traditional open surgery, rAAA is associated with high mortality and significant comorbidity. In addition to age, comorbid conditions can be applied to predict the operative risks for EVAR and open surgery with greater precision for all age groups. This can help select those who may be at reasonable risk for EVAR, even if they are at high risk for open repair (3). The perioperative survival advantage with endovascular repair was sustained for several years, and an aneurysm rupture after repair was uncommon (2). In this report, we used data from a district general hospital and described the clinical outcomes of these patients. In our case, there was only one case, which was an aneurysm-related mortality. These results confirm that EVAR technology has been safely transferred to a district general hospital by our integrated health care system. Coincident with the introduction of EVAR, we observed large population-level declines in short-term AAA-related mortality among elderly patients (3). A less invasive approach to AAA repair may prove to be a more favorable option for rAAA, especially for patients of advanced age with significant comorbidities (12). Our results suggest that endovascular repair continues to improve and is now an acceptable alternative to open repair.
We recommend EVAR as the management of choice for rAAA and for related ailments, in anatomically suitable patients where the local facilities and expertise exist. Using Perclose ProGlide® for selected cases such as no calcification of common femoral artery could reduce blood loss and operative time. These results highlight the need for increased awareness about the condition and suggest ways to improve care trajectories to reduce delay to surgery, thereby minimizing rupture mortality. However, postoperative endoleaks and the need for reintervention continue to pose challenging problems for patients after EVAR. Our results suggest that endovascular repair continues to improve and is now an acceptable alternative to open repair, even when judged in terms of long-term survival.
This study has a number of limitations. First, the retrospective nature may introduce a bias to this analysis. Second, this series included only one district general hospital. We recognize some weaknesses in this study: patients were offered EVAR if anatomically suitable, and therefore, by definition, EVAR patients had more favorable anatomy than those undergoing open repair, thereby introducing a selection bias.
Acknowledgements
We also wish to thank all colleagues in the Department of Medical Research to assist in this research.
Funding: This study cannot be completed without the research fundings from Tungs’ Taichung MetroHarbor Hospital Comprehensive Medical Corp. (research grants No: IRB-TTMHH-104C0006).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional review board at our hospital.
References
- Chang RW, Goodney P, Tucker LY, et al. Ten-year results of endovascular abdominal aortic aneurysm repair from a large multicenter registry. J Vasc Surg 2013;58:324-32. [Crossref] [PubMed]
- Lederle FA, Freischlag JA, Kyriakides TC, et al. Long-term comparison of endovascular and open repair of abdominal aortic aneurysm. N Engl J Med 2012;367:1988-97. [Crossref] [PubMed]
- Schermerhorn ML, Bensley RP, Giles KA, et al. Changes in abdominal aortic aneurysm rupture and short-term mortality, 1995-2008: a retrospective observational study. Ann Surg 2012;256:651-8. [Crossref] [PubMed]
- Brattheim BJ, Eikemo TA, Altreuther M, et al. Regional disparities in incidence, handling and outcomes of patients with symptomatic and ruptured abdominal aortic aneurysms in Norway. Eur J Vasc Endovasc Surg 2012;44:267-72. [Crossref] [PubMed]
- Raats JW, Flu HC, Ho GH, et al. Long-term outcome of ruptured abdominal aortic aneurysm: impact of treatment and age. Clin Interv Aging 2014;9:1721-32. [Crossref] [PubMed]
- Furlough CL, Desai SS, Azizzadeh A. Adjunctive technique for the use of ProGlide vascular closure device to improve hemostasis. J Vasc Surg 2014;60:1693-4. [Crossref] [PubMed]
- Sensi L, Tedesco D, Mimmi S, et al. Hospitalization rates and post-operative mortality for abdominal aortic aneurysm in Italy over the period 2000-2011. PLoS One 2013;8:e83855. [Crossref] [PubMed]
- Mehta M, Byrne J, Darling RC 3rd, et al. Endovascular repair of ruptured infrarenal abdominal aortic aneurysm is associated with lower 30-day mortality and better 5-year survival rates than open surgical repair. J Vasc Surg 2013;57:368-75. [Crossref] [PubMed]
- Gierek D, Cyzowski T, Kaczmarska A, et al. Perioperative prognostic factors in patients with ruptured abdominal aortic aneurysms treated in the intensive care unit. Anaesthesiol Intensive Ther 2013;45:25-9. [Crossref] [PubMed]
- Propper BW, Abularrage CJ. Long-term safety and efficacy of endovascular abdominal aortic aneurysm repair. Vasc Health Risk Manag 2013;9:135-41. [PubMed]
- Gŭllŭ AÜ, Burnaz T, Okten E, et al. Emergent endovascular repair of ruptured abdominal and thoracic aortic aneurysms in a single center: midterm outcomes. Chirurgia (Bucur) 2014;109:753-7. [PubMed]
- Lo RC, Lu B, Fokkema MT, et al. Relative importance of aneurysm diameter and body size for predicting abdominal aortic aneurysm rupture in men and women. J Vasc Surg 2014;59:1209-16. [Crossref] [PubMed]
- Brooke BS, Meguid RA, Makary MA, et al. Improving surgical outcomes through adoption of evidence-based process measures: intervention specific or associated with overall hospital quality? Surgery 2010;147:481-90. [Crossref] [PubMed]
- Hinchliffe RJ, Ribbons T, Ulug P, et al. Transfer of patients with ruptured abdominal aortic aneurysm from general hospitals to specialist vascular centres: results of a Delphi consensus study. Emerg Med J 2013;30:483-6. [Crossref] [PubMed]
- Mehta M, Paty PS, Byrne J, et al. The impact of hemodynamic status on outcomes of endovascular abdominal aortic aneurysm repair for rupture. J Vasc Surg 2013;57:1255-60. [Crossref] [PubMed]
- IMPROVE trial investigators, Powell JT, Hinchliffe RJ, et al. Observations from the IMPROVE trial concerning the clinical care of patients with ruptured abdominal aortic aneurysm. Br J Surg 2014;101:216-24; discussion 224. [Crossref] [PubMed]
- Berland TL, Veith FJ, Cayne NS, et al. Technique of supraceliac balloon control of the aorta during endovascular repair of ruptured abdominal aortic aneurysms. J Vasc Surg 2013;57:272-5. [Crossref] [PubMed]
- Lo RC, Bensley RP, Hamdan AD, et al. Gender differences in abdominal aortic aneurysm presentation, repair, and mortality in the Vascular Study Group of New England. J Vasc Surg 2013;57:1261-8,1268.e1-5.
- Noorani A, Page A, Walsh SR, et al. Mid-term outcomes following emergency endovascular aortic aneurysm repair for ruptured abdominal aortic aneurysms. Eur J Vasc Endovasc Surg 2012;43:382-5. [Crossref] [PubMed]


