
Enhanced efficacy of a novel aspirator in uniportal video-assisted thoracoscopic mediastinal lymph node dissection: a non-randomized prospective clinical trial
Highlight box
Key findings
• This new aspirator with forceps used in video-assisted thoracoscopic surgery (VATS) can effectively shorten the time of mediastinal lymph node dissection and improve the efficiency of thoracoscopic surgery, without increasing lymph node dissection-related adverse events.
What is known and what is new?
• Aspirator is an important instrument in VATS. Traditional aspirators lack the ability to pull and lift tissue and cannot achieve optimal exposure, which limits the accuracy and safety of the operation.
• We invented a new aspirator for VATS, in which the clamping function of the front plier-like structure was added. The new aspirator can pull and clamp.
What is the implication, and what should change now?
• The clamping force needs to be adjusted to avoid tissue fracture when clamping tissue. The transmission device is located in the pipeline structure, which is not convenient for postoperative cleaning and disinfection.
Introduction
Lung cancer is one of the leading causes of mortality in the world (1). Surgery is regarded as the first treatment choice for patients with non-small cell lung cancer (NSCLC), which is 85% of all lung cancer patients (2). Since its first report in the 1990s (3), video-assisted thoracoscopic surgery (VATS) has become the standard surgical procedure for early-stage NSCLC in recent years. Mediastinal lymph node dissection is an important part of VATS, according to the National Comprehensive Cancer Network and the recently updated European Society for Medical Oncology guidelines (4,5). It is thought to improve survival rates in patients with early-stage NSCLC patients (6).
Since the main incision of VATS is often less than 3 cm, successful VATS depends on well-designed surgical instruments. Surgical aspirators play a crucial role in this process. In addition to the aspirating functions, the aspirator is also responsible for exposing the surgical field of vision. Traditional aspirators can push and press tissue in surgery, but they lack the ability to pull and lift tissue, which is essential in many procedures, especially the process of lymph node dissection. Additional forceps may help when pulling or lifting is needed, but more instrumentation means more interference during the operation. Therefore, multifunctional instruments are critical in VATS.
Therefore, we designed a new surgical aspirator that combines the function of traditional surgical aspirators and thoracoscopic forceps. In this study, we aimed to validate the efficacy and safety of this new surgical aspirator in the process of lymph node dissection in VATS that may be beneficial to most NSCLC patients. We present this article in accordance with the TREND reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1152/rc).
Methods
Study design
The study was a prospective non-randomized intervention clinical study. Patients scheduled for surgical resection of early-stage NSCLC in the Zhejiang Cancer Hospital from May 2021 were planned to be enrolled in the study. Enrolled patients were allocated according to the parity of the hospital number: odd hospital number (with last digit 1, 3, 5, 7, 9) to the traditional aspirator group (control) and even hospital number (with last digit 0, 2, 4, 6, 8) to the new aspirator group (intervention).
The inclusion criteria of this study were as follows: (I) age was ≥18 and ≤85 years; (II) diagnosed with NSCLC by preoperative biopsy or intraoperative cytopathology; (III) diagnosed as invasive lung cancer and has the surgical indication of systematic mediastinal lymph node dissection; (IV) the function of organs such as heart and lung can support pulmonary resection. Exclusion criteria were as follows: (I) age was <18 or >85 years; (II) had surgical contraindications such as heart failure or use of anticoagulant drugs in one week; (III) had already undergone previous ipsilateral thoracic surgery; (IV) mediastinal lymph node dissection was not needed; (V) preoperative images suggested possible calcified lymph nodes, which may cause difficulties in dissection; (VI) other situations VATS mediastinal lymph node dissection could not proceed, such as having converted to open surgery.
Two experienced thoracic surgeons were recruited to test the new aspirator independently. They both performed uniportal VATS. After full practice using the new aspirator on about 30 patients, the two surgeons started to perform mediastinal lymph node dissection with a traditional aspirator or new aspirator. All the operations were uniportal VATS, and the incision located between posterior axillary line and midaxillary line, fourth intercostal. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics committee of Zhejiang Cancer Hospital (approval date 2021-03-08, approval code IRB-2021-3). Informed consent was obtained from all patients.
Aspirator design
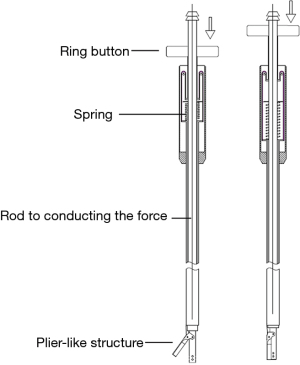
On the basis of a traditional surgical aspirator, the clamping function of the front plier-like structure is added. Besides, our new tool adds an annular button (with spring for returning) located on the handheld end, and a rod to conducting the force. Under normal conditions, the button is in the initial position, and the pliers remain closed. When surgeon presses the button, the force transmits to the pliers through the rod, driving the pliers open, and the aspirator is ready to clamp tissue. After the button is released, the pliers return to the closed state, and the tissue is tightly clamped. The structure (including button, spring, rod and pliers) is shown in Figure 1. The new aspirator can replace the need for forceps and facilitate the surgical procedures, especially for mediastinal lymph node dissection (Figures 2,3). Videos 1,2 show typical scenes in which the new aspirator plays significant role. The new aspirator passed experimental surgery on pig before clinical trial.


Statistical analysis
The basic information such as sex, age, location of the lobe tumor was recorded before surgery. The time spent for lymph node dissection was defined as the time taken from incision of mediastinal pleura to lymph node clearance and cessation of bleeding. After operation, the pathological type of tumor and number of harvested lymph nodes were recorded, as well as adverse events related to lymph node dissection during or after the operation, such as injury of main blood vessels or bronchus and chylothorax. Injury of main blood vessels or bronchus was defined as injury that needs sewing during operation. Chylothrax was defined as chylous fluid found in postoperative thoracic drainage. Postoperative complications not related to mediastinal lymph node dissection were excluded, such as pneumothorax and postoperative bleeding which is not at the lymph node dissection site.
The data analysis was performed using SPSS v23.0 (SPSS Inc., Chicago, IL, USA). A two-sided P value less than 0.05 was regarded as a statistically significant difference. Baseline comparability was first checked, and an independent-samples t-test was applied to analyze the differences in sex, age, pathological type and adverse events related to lymph node dissection. If baseline data were not comparable, multiple regression was used. An independent-samples t-test was applied to analyze the differences in surgery time.
Results
In total, 581 patients who need or may need to receive mediastinal lymph node dissection entered our screening range; 77 of them failed the procedure of screening. The reason included the result of cryopathology not suggesting mediastinal lymph node dissection (such as benign or carcinoma in situ), conversion to open surgery before mediastinal lymph node dissection, fluctuation of patient’s condition during surgery and a compromise resection being performed, etc.
A total of 504 patients went through the procedure of screening and were selected. The age of the enrolled patients ranged from 34 to 83 (average 64.10, median 65) years. The tumor was located on the right for 256 patients and on the left for 248 patients. The baseline data are shown in Table 1. Uniportal VATS mediastinal lymph node dissection was performed.
Table 1
| Characteristics | Traditional aspirator | New aspirator | P |
|---|---|---|---|
| Sex | 0.878 | ||
| Male | 133 | 118 | |
| Female | 117 | 136 | |
| Age (year), median [range] | 64.26 [37–83] | 63.53 [34–82] | 0.372 |
| Pathological pattern | 0.704 | ||
| Adenocarcinoma | 136 | 147 | |
| Squamous cell carcinomas | 105 | 95 | |
| Others | 9 | 12 | |
| Tumor location | 0.501 | ||
| Right superior lobe | 36 | 54 | |
| Right middle lobe | 11 | 17 | |
| Right inferior lobe | 76 | 62 | |
| Left superior lobe | 56 | 58 | |
| Left inferior lobe | 71 | 63 | |
| Number of harvested lymph nodes | |||
| No. 2/4R | 5.70 | 5.97 | 0.578 |
| No. 7R | 3.83 | 3.72 | 0.393 |
| No. 7L | 3.64 | 3.78 | 0.311 |
When dealing with No. 2/4R lymph nodes, surgeons spent 544.71±120.80 (range, 332–917, median 541) seconds with the traditional aspirator and 507.54±100.00 (range, 348–702, median 520) seconds with the new aspirator. An independent-samples t-test showed that P=0.008, which indicated a statistically significant difference between the two groups. The traditional aspiration group had an average surgery time of 507.11±104.61 (range, 310–785, median 510) seconds for No. 7R lymph nodes and 608.47±128.50 (range, 397–919, median 606) seconds for No. 7L lymph nodes, while those in the new aspiration group were 465.09±94.94 (range, 271–744, median 476) seconds (P=0.001) and 549.39±102.11 (range, 368–782, median 538) seconds (P<0.001), respectively. The data are shown in Table 2. The new aspirator effectively shortened mediastinal lymph node dissection time.
Table 2
| Lymph nodes | Traditional aspirator, mean ± SD (s) | New aspirator, mean ± SD (s) | P |
|---|---|---|---|
| No. 2/4R | 544.71±120.80 | 507.54±100.00 | 0.008 |
| No. 7R | 507.11±104.61 | 465.09±94.94 | 0.001 |
| No. 7L | 608.47±128.50 | 549.39±102.11 | <0.001 |
SD, standard deviation; s, seconds.
In the traditional aspirator group, 3 patients experienced adverse events related to lymph node dissection during the operation (contralateral bronchial injury during dissecting subcarinal lymph node, superior vena cava bleeding and azygos vein arch bleeding) while there were no adverse events in the new aspirator group. Postoperative chylothorax was found in 7 patients in the traditional aspirator group and 8 patients in the new aspirator group (P=0.818). One patient in the new aspirator group underwent reoperation for chylothorax, as conservative treatment was futile. The safety-related results are shown in Table 3, and there were no other accidental tissue injury or postoperative adverse events related to mediastinal lymph node dissection.
Table 3
| Case number | Aspirator | Sex | Age (year) | Tumor location | Adverse events | |
|---|---|---|---|---|---|---|
| During operation | Post operation | |||||
| 1 | New | Female | 73 | Left inferior lobe | Chylothorax | |
| 2 | New | Female | 69 | Left inferior lobe | Chylothorax | |
| 3 | New | Male | 59 | Left inferior lobe | Chylothorax | |
| 4 | New | Male | 65 | Left superior lobe | Chylothorax | |
| 5 | New | Female | 77 | Right inferior lobe | Chylothorax | |
| 6 | New | Female | 75 | Right superior lobe | Chylothorax—reoperation | |
| 7 | New | Male | 55 | Right inferior lobe | Chylothorax | |
| 8 | New | Male | 57 | Right superior lobe | Chylothorax | |
| 9 | Traditional | Male | 69 | Left superior lobe | Contralateral bronchial injury | |
| 10 | Traditional | Male | 47 | Left inferior lobe | Chylothorax | |
| 11 | Traditional | Male | 77 | Right superior lobe | Chylothorax | |
| 12 | Traditional | Male | 53 | Right inferior lobe | Chylothorax | |
| 13 | Traditional | Male | 59 | Right superior lobe | Chylothorax | |
| 14 | Traditional | Female | 73 | Right middle lobe | Chylothorax | |
| 15 | Traditional | Female | 76 | Right inferior lobe | Chylothorax | |
| 16 | Traditional | Female | 56 | Left superior lobe | Chylothorax | |
| 17 | Traditional | Female | 73 | Right inferior lobe | Bleeding of superior vena cava | |
| 18 | Traditional | Female | 65 | Right superior lobe | Bleeding of azygos vein arch | |
Discussion
VATS has become the standard operation for the treatment of patients with early NSCLC (7). Surgical aspirators play an important role in the process of thoracoscopic surgery. In addition to the suction function, the aspirator can be used to expose the surgical field, such as providing tissue tension when cutting with energy devices. The traditional aspirator can only push and press the tissue during the operation but cannot pull and lift the tissue, which is often required during the operation. A common scenario in VATS is shown in Figure 4. Because the traditional aspirator could not help to expose lymph nodes adequately, we had to suspend the operation and use forceps instead. However, if there is external lymph node bleeding, the view will be covered by blood and still cannot be fully exposed without an aspirator. Therefore, switching between traditional aspirators and forceps will prolong the operation time and cause greater surgical trauma to patients, and a new surgical aspirator with the functions of both traditional aspirators and forceps is of great significance.

In this study, the new aspirator showed a significant advantage over the traditional aspirator in mediastinal lymph node dissection. For No. 2/4R, No. 7R and No. 7L lymph nodes, use of the new aspirator could significantly reduce time and facilitate the operation. The function of grasping shows its effect in exposing the surgical field of mediastinal lymph node dissection, which lived up the original intention of the design. According to our experience, the new aspirator could move the lymph nodes to almost every direction and expose its every side to dissociate, when it was relatively difficult for traditional aspirator to expose the bottom and dorsal side (relative to camera perspective) of lymph nodes. The advantage in exposure saves time.
The occurrence of postoperative lymph node-related complications, such as chylothorax, has not significantly increased. In particular, there were no adverse events related to mediastinal lymph node dissection during the operation, such as bronchial and main blood vessel injury, in the new aspirator group, which showed that the new aspirator showed good safety and had great potential in VATS. In the traditional group, three adverse events happened. The first case happened in the process of dissecting No. 7L, as bleeding of lymph nodes obstructed the exposure of contralateral bronchial, which was injured by ultrasound dissector. In the second case, the 4R lymph node was calcifying, and showed tight adhesion with the wall of the superior vena cava; the bleeding happened when the surgeon tried to dissociate with hook. The third case is similar—the 4R lymph node adhered tight with the wall of azygos vein arch, which is injured when the surgeon tried blunt dissection. These three adverse events were adventive and regarded unrelated to the aspirator.
In this study, the operation time of left upper mediastinal lymph node dissection, such as No. 4L, No. 5 and No. 6, was not compared between the two groups. That was with reasons. In our preliminary study, we found the variance of time spent in dissection of No. 4L is large, which may be because the actual size, number (some patients have only one or even no No. 4L lymph node, when others may have three or more) and location (difficult to expose when near arterial ligament; easier for exposure when closer to the bulge) of No. 4L differ, and these factors have great influence for its procedure time. Meanwhile, we found the new aspirator can show some advantage in the operation time of No. 5 and No. 6, but not significant. We regarded the result as the exposure of No. 5 and No. 6 is relatively easy, and the time of dissection is short (compared to that of No. 2/4R, No. 7R and No. 7L), and the convenience of new aspirator cannot fully play its role. By contrast, the size and location of No. 2/4R, No. 7R and No. 7L are relatively fixed, and the operation time for their dissection has enough space for descending. In the formal phase of study, the results meet our expectations.
The learning process of the new aspirator is short for experienced thoracic surgeons. For the first five VATS operations, the control of the equipment appears to be rusty. When the number of VATS operations comes to ten, the control becomes proficient. Experienced thoracic surgeons are able to master the new aspirator in twenty VATS operations. Taking the efficacy of new aspirator to VATS operations into account, the learning process is worthy, and the learning curve enables the new device to have prospect of popularization.
In this study, the energy devices used by the two surgeons were not limited. Therefore, they could have the space to produce a full effect of both new and traditional aspirators. In the actual process, both surgeons used ultrasound dissector in most part of dissection, and hook also played a role in the process, mainly to cut the visceral pleura open and stop bleeding. The efficacy of new aspirator when cooperating with other energy devices, such as bipolar electrocoagulation, is waiting to be disclosed.
As a new invention, the aspirator has some defects that need to be improved. The clamping force needs to be adjusted to avoid tissue fracture when clamping tissue. Meanwhile, the transmission device is located in the pipeline structure, which is not convenient for postoperative cleaning and disinfection. The elasticity of the spring is also worthy of discussion, as low elasticity equals difficulty to press, and excessive elasticity may induce releasing the clamp inadvertently.
Conclusions
This is the first report of a new suction device combining the functions of both traditional surgical aspirators and forceps, which may effectively shorten the time of mediastinal lymph node dissection and improve the efficiency of thoracoscopic surgery without increasing lymph node-related adverse events. More assessors are needed to provide a consensus statement before it becomes a standard of practice for lymph node dissection.
Acknowledgments
The authors appreciate the great support from Dr. Marcello Migliore (King Faisal Specialist Hospital and Research Center, Saudi Arabia), Dr. Calvin S. H. Ng (Prince of Wales Hospital, China), Dr. Gregor J. Kocher (Bern University Hospital, Switzerland), Dr. Patrick Zardo (Hannover Medical School, Germany), Dr. Narasimman Sathiamurthy (Kuala Lumpur Hospital, Malaysia) and Dr. Teruaki Mizobuchi (Chibaken Saiseikai Narashino Hospital, Japan) in improving the quality of this paper.
Funding: The study was supported by
Footnote
Reporting Checklist: The authors have completed the TREND reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1152/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1152/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1152/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1152/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics committee of Zhejiang Cancer Hospital (approval date 2021-03-08, approval code IRB-2021-3). Informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. CA Cancer J Clin 2020;70:313. [Crossref] [PubMed]
- Sher T, Dy GK, Adjei AA. Small cell lung cancer. Mayo Clin Proc 2008;83:355-67. [Crossref] [PubMed]
- Kirby TJ, Rice TW. Thoracoscopic lobectomy. Ann Thorac Surg 1993;56:784-6. [Crossref] [PubMed]
- Remon J, Soria JC, Peters S, et al. Early and locally advanced non-small-cell lung cancer: an update of the ESMO Clinical Practice Guidelines focusing on diagnosis, staging, systemic and local therapy. Ann Oncol 2021;32:1637-42. [Crossref] [PubMed]
- Ettinger DS, Wood DE, Aisner DL, et al. Non-Small Cell Lung Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2022;20:497-530. [Crossref] [PubMed]
- Cao J, Xu J, He Z, et al. Prognostic impact of lymphadenectomy on outcomes of sublobar resection for stage IA non-small cell lung cancer ≤2 cm. J Thorac Cardiovasc Surg 2018;156:796-805.e4. [Crossref] [PubMed]
- Scarci M, Gonzalez-Rivas D, Schmidt J, et al. Management of Intraoperative Difficulties During Uniportal Video-Assisted Thoracoscopic Surgery. Thorac Surg Clin 2017;27:339-46. [Crossref] [PubMed]


