Delayed aortic rupture resulting from postoperative superficial sternal wound infection
Introduction
Postoperative sternal wound infection is a relatively frequent complication of cardiac surgery. Deep sternal wound infection (DSWI) commonly known as mediastinitis contributes significantly to patient morbidity and mortality, whereas superficial sternal wound infection (SSWI) leads to benign course mostly. Unfortunately, we experienced a fatal case of delayed aortic rupture resulted from postoperative SSWI.
Case presentation
A 50-year-old male presented with sudden cardiac arrest due to ventricular fibrillation. He had only a history of hypertension and was eating a meal when the arrest occurred. A successful resuscitation with electric cardioversion and cardiac massage restored patient’s mental tone and cardiac rhythm 50 minutes after the cardiac arrest. He was admitted to the intensive care unit, and an echocardiogram showed severe aortic regurgitation with coaptation failure and globally decreased left ventricular systolic function.
We performed an aortic valve replacement (AVR) with a mechanical valve through a conventional median sternotomy. The cardiopulmonary bypass time was 90 minutes, and cross-clamping time was 60 minutes. A postoperative mediastinal hemorrhage requiring transfusion occurred, and the amount within the first 24 hours was 1,560 mL. We transfused six packed red blood cells and five fresh frozen plasmas. The bleeding ceased the next day, and the chest tubes were removed 6 days after the operation. We found that the lower sternotomy wound showed dehiscence and contained bloody effusions 13 days after the operation. The sternum was stable, and there was focal wound dehiscence between the tube sites and the xyphoid process. There was some amount of hematoma without any sign of infection, so it was considered that the standing hematoma from the postoperative bleeding had resulted in wound dehiscence without any growing microorganisms. We frequently exchanged the dressing for a week and performed wound debridement and primary closure under general anesthesia. The patient was discharged a week after the wound closure; then all the stitches were removed a week later.
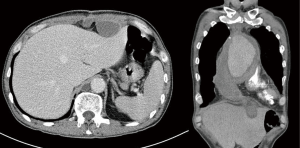
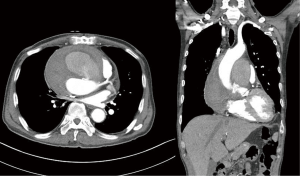
The patient had continued to complain about non-specific symptoms, including dysphagia, anorexia, generalized weakness, and febrile sense. Three months after the valve operation, he presented with severe dyspnea, which had never before been observed, and chest computed tomography revealed an ascending aortic rupture with large hematoma compressing the main pulmonary artery (Figure 1). We performed an emergent operation for bleeding control. A cardiopulmonary bypass through the femoral artery and vein was mandatory for expected massive bleeding after sternotomy. Deep hypothermic (rectal temperature <20 °C) total circulatory arrest was induced for 10 minutes, followed by an excision of the pseudoaneurysm and infusion of cardioplegia after aortic cross-clamping. The cardiopulmonary bypass time was 251 minutes, and the aortic cross-clamping time was 25 minutes. We discovered two small linear perforations (<2 mm) on the aortic wall just below the previous aortotomy site where the perforated aortic walls were very thin and fragile. We repaired the sites using multiple interrupted sutures and applied a fibrin glue-coated collagen patch and a bovine serum albumin-glutaraldehyde tissue sealant. We achieved complete bleeding control. There was no evidence of infection such as abscess formation and tissue dehiscence, but there was a fragile organized hematoma around the xyphoid process (Figure 2). The hematoma formed a cavity with thickened subcutaneous tissue. We completely debrided the hematoma including the surrounding tissue, then performed interrupted sutures. Chest tubes were placed through the newly-undermined subcutaneous tracts. All the cultures of the hematoma and debris were negative.
Postoperatively, the vital signs of the patient were stable with controlled systolic blood pressure under 120 mmHg. The patients showed confused mentality and could not obey a command. Mechanical ventilation was weaned 3 days after the operation, but the patient showed irritability and suffered from respiratory distress 22 hours after the extubation. The patient’s blood pressure could not be detected, and massive bleeding from the chest tube resulted in loss of consciousness. The patient died of hypovolemic shock despite efforts to resuscitate him.
Discussion
The percentage of incidence of mediastinal wound infection in patients undergoing median sternotomy and open-heart surgery can be up to 3–5% (1-3). Furthermore, 20–30% of these patients develop DSWI with associated morbidity and mortality (4). Parissis et al. reviewed 3,896 cardiac surgery patients prospectively and reported that the overall mortality of the DSWI group was 15.4% (5). On the other hand, the SSWI could be treated with appropriate antibiotics, local drainage, and debridement of the wound. The mortality of SSWI has been reported to be 0.5–4.4% (1,5).
While risk analyses and outcomes of mediastinal wound infection have been studied in great frequency, no group has rendered a report studying the causes of mortality resulting from mediastinal wound infection. DSWI has a definition and diagnostic guidelines and is classified according to El Oakley and Wright (6). Furthermore, many medical and surgical treatments or prophylaxes have been investigated systematically in DSWI patients (7,8). Based on past experiences, the causes of mortality in patients with DSWI were able to be postulated to be vital organ infection with septic shock and multi-organ failure. However, no postulation about the causality between SSWI after cardiac surgery and patient mortality has been made up to this point in time.
We have assumed the cause of the aortic rupture in our case. The aortic walls of the patient, especially sinotubular junction and sinus portion, were slightly thinned at initial operation. Since the aortotomy was completely repaired using two Teflon felts without bleeding, we did not add any procedures on the aortic root. But, the postoperative bleeding could occur from the aortotomy site or the thinned aortic root which was stretched and over-tensioned resulting from the aortotomy repair. Additionally, this case study hypothesizes that a small amount of the hematoma around the xyphoid process resulted in lower sternotomy wound dehiscence, which caused a secondary latent infection. There was no evidence of gross wound infection and microorganisms, but the patient suffered from some clinical signs of infection such as general weakness, febrile sense, and indigestion. The latent infection brought about an aortitis, which led to thinning and perforation of the aortic wall. It is very possible that SSWI itself has the potential to cause mortality, and therefore every care should be taken to minimize such a possibility.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: This study was approved by the institutional review board and ethics committee.
References
- Ridderstolpe L, Gill H, Granfeldt H, et al. Superficial and deep sternal wound complications: incidence, risk factors and mortality. Eur J Cardiothorac Surg 2001;20:1168-75. [Crossref] [PubMed]
- Olsen MA, Lock-Buckley P, Hopkins D, et al. The risk factors for deep and superficial chest surgical-site infections after coronary artery bypass graft surgery are different. J Thorac Cardiovasc Surg 2002;124:136-45. [Crossref] [PubMed]
- Ariyaratnam P, Bland M, Loubani M. Risk factors and mortality associated with deep sternal wound infections following coronary bypass surgery with or without concomitant procedures in a UK population: a basis for a new risk model? Interact Cardiovasc Thorac Surg 2010;11:543-6. [Crossref] [PubMed]
- Parisian Mediastinitis Study Group. Risk factors for deep sternal wound infection after sternotomy: a prospective, multicenter study. J Thorac Cardiovasc Surg 1996;111:1200-7. [Crossref] [PubMed]
- Parissis H, Al-Alao B, Soo A, et al. Risk analysis and outcome of mediastinal wound and deep mediastinal wound infections with specific emphasis to omental transposition. J Cardiothorac Surg 2011;6:111. [Crossref] [PubMed]
- El Oakley RM, Wright JE. Postoperative mediastinitis: classification and management. Ann Thorac Surg 1996;61:1030-6. [Crossref] [PubMed]
- Floros P, Sawhney R, Vrtik M, et al. Risk factors and management approach for deep sternal wound infection after cardiac surgery at a tertiary medical centre. Heart Lung Circ 2011;20:712-7. [Crossref] [PubMed]
- Lehot JJ. Cefazolin prophylaxis during cardiac operations. Ann Thorac Surg 2004;77:755-6; author reply 756. [Crossref] [PubMed]