
Osimertinib as first-line treatment for recurrent lung cancer patients with EGFR mutation
Highlight box
Key findings
• Brain metastasis and a deteriorated performance status resulted in a poor outcome in recurrent EGFR mutated lung cancer patients who received 1st-line osimertinib treatment.
What is known and what is new?
• There is still some ongoing debate in the scientific community as osimertinib has been approved based on disease-free survival rather than overall survival.
• The treatment outcome is poor in patients with brain metastasis or with deteriorated performance status. Patients treated with osimertinib after disease recurrence have a high incidence of severe adverse events.
What is the implication, and what should change now?
• Adjuvant osimertinib is recommended unless contraindicated.
Introduction
Osimertinib has been approved as adjuvant therapy in various countries following a positive result of superior disease-free survival (DFS) in the osimertinib arm with a hazard ratio of 0.17 among patients with stage II to IIIA disease (a primary endpoint). This phase III study (ADAURA), comparing osimertinib given daily for three years with placebo after complete resection of lung cancer with EGFR mutation, exceeded an expectation and the trial was unblinded in April 2020 (1). Furthermore, the planned final analysis of overall survival (OS) has shown a better survival in osimertinib arm with a hazard ratio of 0.49, without reporting any new adverse events of special interest (2). Nevertheless, there is still an ongoing debate whether adjuvant osimertinib after surgical resection or starting osimertinib at disease recurrence is the best option.
In recent trials, including advanced non-small cell lung cancer, the study endpoints were mainly progression-free survival (PFS), or DFS for peri-operative adjuvant studies, because a meta-analysis showed that PFS could be a surrogate for OS (3). However, the meta-analysis was based on results obtained with cytotoxic drugs, not tyrosine kinase inhibitors (TKI). Although many phase III trials comparing EGFR-TKI with cytotoxic drugs failed to show an OS benefit (4-7), the FLAURA study, which compared osimertinib with 1st generation EGFR-TKI clearly showed better OS in the osimertinib arm (8). Similarly, adjuvant studies comparing 1st generation EGFR-TKI with cytotoxic chemotherapy, namely, CTONG1104 (9,10) and IMPACT (11), also failed to show benefits in terms of OS.
To answer this question, we curated a case series at our institution in which we documented patterns of recurrence and efficacy and safety of osimertinib after disease recurrence. We present this article in accordance with the STROBE and MDAR reporting checklists (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-537/rc).
Methods
Patients
Consecutive patients who received osimertinib as first-line therapy after surgery at the Department of Thoracic and Breast Surgery, Oita University Faculty of Medicine between September 2018 and January 2023 were included. Those who underwent surgery without curative intent were excluded because we did not want to include patients with macroscopic disease (i.e., partial resection of the lung for diagnostic purposes in patients with advanced lung cancer). The pathological stage was defined based on the 8th edition of the American Joint Committee on Cancer lung cancer staging system and the histological classification (12) was determined based on the 2015 World Health Organization Classification of Tumors of the Lung, Pleura, Thymus and Heart (13). The efficacy and adverse events were collected from medical records on February 20th, 2023. Adverse events were evaluated using the Common Terminology Criteria for Adverse Events (CTC-AE) version 5.0 (14).
EGFR testing
EGFR mutation was determined by either CyCleave PCR (SRL Inc., Tokyo, Japan) or a cobas EGFR mutation detection kit version 2.0 (SRL Inc.), after extracting genomic DNA from formalin-fixed paraffin-embedded tissue sections from surgically resected primary tumors.
Statistical analysis
We chose the duration of osimertinib treatment (DoT) as an endpoint for efficacy, because disease recurrence in most patients was revealed by follow-up computed tomography (CT) or magnetic resonance imaging (MRI), they had no measurable disease. DoT was calculated as an actual period of osimertinib treatment, and those patients who were still on osimertinib and those patients who had ceased osimertinib because of adverse events were censored. The follow-up schedule in our institution was usually annual brain MRI and semi-annual chest CT in the postoperative setting (15), and more frequent after patients started osimertinib treatment for disease recurrence. The probability of survival was analyzed by the Kaplan-Meier method using the date of osimertinib introduction as the starting point. The log-rank test was used to determine the significance of differences between subgroups. The site of first recurrence was determined to be local if the patients experienced intrathoracic recurrence (pleural dissemination, malignant pleural effusion, pulmonary metastasis in the ipsilateral thoracic cavity or regional lymph nodes). If any distant metastasis was observed at recurrence along with local recurrence, the site of first recurrence was defined as distant. All statistical analyses were performed using EZR version 1.55 (16).
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board at Oita University Faculty of Medicine (IRB No. 698), and informed consent was obtained from each patient.
Results
Patients’ characteristics
During the period, 20 patients were identified to receive first-line osimertinib treatment after disease recurrence [male, n=6; median age, 75 years (range, 55–85 years)] (Table 1). The EGFR mutation type was L858R in 11 patients, exon 19 deletion (Del19) in 8 patients, and L861Q (uncommon mutation) in 1 patient. The performance status (PS) was 0 or 1 in all but two patients, who had central nervous system (CNS) metastasis and were therefore PS 3. The first site of postoperative recurrence was locoregional in 5 patients and distant in 15 patients, including 7 patients with CNS metastasis.
Table 1
| Factors | Categories | Value |
|---|---|---|
| Age at recurrence, years | 75 [55–85] | |
| Sex | Male/female | 6/14 |
| PS at recurrence | 0/1/2/3 | 15/3/0/2 |
| Smoking | Never/ever | 14/6 |
| EGFR mutation | L858R/Del19/L861Q | 11/8/1 |
| Clinical stage | I/II/III | 12/6/2 |
| pStage†,‡ | I/II/III/IVA | 11/3/4/2 |
| Post operative adjuvant | None/UFT/VP | 13/5/2 |
| First site of recurrence | Locoregional/distant | 5/15 |
| Brain metastasis (first site) | Positive§/negative | 7/13 |
| RFS, months | 33.1 [0–141.1] |
†, for stage I, IA2/IA3/IB =3/3/5; ‡, two patients had pleural dissemination found intra-operatively, and therefore pStage IVA; §, two patients had leptomeningeal metastasis. Data are presented as median [range] or number. PS, performance status; pStage, pathological stage; UFT, tegafur and uracil; VP, vinorelbine and cisplatin; RFS, recurrence-free survival.
Duration of osimertinib treatment
As of February 2023, 10 patients were still on osimertinib, including 3 with CNS metastasis, and the median DoT was not reached (Figure 1A). Patients who had brain metastasis as the first site of recurrence experienced poorer outcomes (DoT not reached vs. 23.7 months, P=0.04, Figure 1B). PS was also related to DoT, although the number of patients with poor PS was small (DoT not reached in PS 0, 2.5 months in PS 1–3, P=0.0005, Figure 1C). Three patients with symptomatic brain metastasis (including two with leptomeningeal metastasis) initially responded to osimertinib, but died of disease progression after 23.7, 11.8, and 3.9 months of treatment, respectively. There were no significant differences in DoT according to age, sex, smoking, EGFR mutation type (Figure 1D), adjuvant therapy, clinical Stage, pathological Stage, first site of recurrence, or recurrence-free survival.

Adverse events, reasons for treatment discontinuation and mechanism of resistance
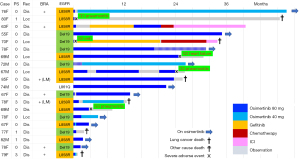
The treatment courses of individual patients are shown in Figure 2. Although five patients were unable to continue osimertinib due to serious adverse effects (pneumonitis, n=3; drug eruption, n=1; and heart failure, n=1), there was no treatment-related mortality. Among them, one patient switched to gefitinib after experiencing severe drug eruption (Stevens-Johnson syndrome, the 5th patient from the top, Figure 2). Another patient (the third patient from the top, Figure 2) switched to gefitinib because of financial issues, and ended up using osimertinib after disease progression during gefitinib treatment. The reason for osimertinib discontinuation was disease progression in other patients. The mechanism of resistance to osimertinib treatment was unknown, except for one patient (the third patient from the top, Figure 2), who had small cell transformation diagnosed from malignant pleural effusion and went on to receive carboplatin, etoposide and atezolizumab. At the time of writing this report, the patient remains on maintenance atezolizumab without evidence of disease progression.
Discussion
Osimertinib was developed for EGFR T790M, a major cause of acquired resistance to first- and second-generation EGFR-TKIs (17). Because osimertinib also demonstrates high specificity to activating EGFR mutations, it shows a very favorable toxicity profile (18). Therefore, it can also be delivered to patients with a deteriorated PS, elderly patients, and patients with co-morbidities. However, the PFS is shorter in patients with a poor PS, when they are treated with osimertinib (19-21).
CNS metastasis is a common event in lung cancer patients with EGFR mutation (22). Patients should be carefully examined for CNS metastasis with brain MRI, as it frequently leads to a decline in PS, analogous to the impact of bone metastasis. Although osimertinib is effective for patients with CNS metastasis, the PFS is shorter in those patients (23).
It has been reported that the odds ratio of brain recurrence becomes the highest at 15 months after surgery (24). Furthermore, an analysis using proportional hazards competing risks and multistate models with data from the International Adjuvant Lung Cancer Trial revealed that platinum doublet could not reduce the risk of CNS metastasis (25). In the adjuvant setting, gefitinib or erlotinib could not effectively inhibit CNS recurrence (9,11), but osimertinib could (1). The difference between the drugs, especially in patients without CNS metastasis, is not clear. In patients with CNS metastasis, the CNS fluid penetration rates were similar between drugs with gefitinib being 1.13% to 1.30% (26,27) and osimertinib being 0.79% to 1.47% (28,29). It has been reported that the concentration of osimertinib in the CNS fluid is higher in comparison to other TKIs when they are delivered orally (30).
As for adverse events, the incidence of interstitial pneumonitis is the greatest concern in advanced lung cancer treated with osimertinib (all-grade, 3.9%; grade ≥3, 2.1%, FLAURA trial) (31), especially among the Japanese subset (all-grade, 12.3%; grade ≥3, 1.5%) (32). In this study, 3 patients developed grade 3 pneumonitis (15%); this incidence is higher in comparison to clinical trials, as is also reported in other real-world studies (33). However, no grade ≥3 pneumonitis was observed in the ADAURA study (1). This could be explained by the fact that the incidence of drug-related pneumonitis is related to smoking status and poor PS before treatment (34). In fact, in the ADAURA trial, 71.5% of the patients were never smokers and 64% had PS 0 (1), while in the FLAURA trial, 64% were never smokers and 41% had PS 0 (31). Even when the discontinuation of osimertinib is required due to grade 1–2 pneumonitis (33,35), the careful re-administration of osimertinib when the patient experiences recurrence is feasible (36,37). There are also studies showing that the re-administration of TKIs after disease recurrence is safe and effective (38,39).
Although most patients receive benefit from adjuvant osimertinib, there may still be a group who does not require adjuvant treatment. Circulating tumor DNA might be helpful in patient selection and treatment monitoring (40). We had eight patients who experienced recurrence even though their pathological stages were IA–IB. Several studies reported the risk factors for recurrence in patients with completely resected stage I lung cancer (41), and the ADAURA2 study is ongoing for high-risk stage I patients (42). Concomitant molecular alteration is also important in predicting the response to adjuvant EGFR-TKI. NKX2-1 gain, CDK4 gain, TP53 mutation, and MYC gain have been reported to predict significantly better survival in patients who receive adjuvant EGFR-TKI (43). We reported that NOTCH1 and CTNNB1 mutations exist as an early event, and remain after acquired resistance (44). For these events, there might be a strategy to enhance EGFR-TKI treatment by combining treatment, such as NOTCH inhibitors (45,46) or Cyclin-dependent kinase 4/6 inhibitors (47).
Conclusions
In conclusion, our data showed a favorable overall response to osimertinib in patients with postoperative recurrence, but patients with brain metastasis or with poor PS showed a poor prognosis. While starting osimertinib at recurrence effectively rescues most patients, recurrence with poor PS and brain metastasis is associated with abysmal outcomes; since the drug is well tolerated, starting treatment in the adjuvant setting is sensible.
Acknowledgments
The authors would like to thank Dr. Brian Quinn, Editor-in-Chief, Japan Medical Communication, Fukuoka, Japan for his critical comments on the manuscript.
Funding: This work was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE and MDAR reporting checklists. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-537/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-537/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-537/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-537/coif). AO has received speakers bureaus from AstraZeneca (Cambridge, UK), Chugai Pharmaceutical (Tokyo, Japan), MSD Japan (Tokyo, Japan), Bristol Myers Squibb (Tokyo, Japan), and Ono Pharmaceutical (Tokyo, Japan), and on the Advisory Board for AstraZeneca (Cambridge, UK). AO reports grant from the Japan Society for the Promotion of Science (No. JP 21K08889). KS has received grants from AstraZeneca (Cambridge, UK), Chugai Pharmaceutical (Tokyo, Japan), MSD Japan (Tokyo, Japan), Bristol Myers Squibb (Tokyo, Japan), and Ono Pharmaceutical (Tokyo, Japan), speaker and consultant honoraria from AstraZeneca (Cambridge, UK), Chugai Pharmaceutical (Tokyo, Japan), MSD Japan (Tokyo, Japan), Bristol Myers Squibb (Tokyo, Japan), and Ono Pharmaceutical (Tokyo, Japan), and on the Advisory Board for AstraZeneca (Cambridge, UK) and Chugai Pharmaceutical (Tokyo, Japan). KS reports grant from Japan Society for the Promotion of Science (No. JP 20K09168). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board at Oita University Faculty of Medicine (IRB No. 698), and informed consent was obtained from each patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wu YL, Tsuboi M, He J, et al. Osimertinib in Resected EGFR-Mutated Non-Small-Cell Lung Cancer. N Engl J Med 2020;383:1711-23. [Crossref] [PubMed]
- Tsuboi M, Herbst RS, John T, et al. Overall Survival with Osimertinib in Resected EGFR-Mutated NSCLC. N Engl J Med 2023;389:137-47. [Crossref] [PubMed]
- Mauguen A, Pignon JP, Burdett S, et al. Surrogate endpoints for overall survival in chemotherapy and radiotherapy trials in operable and locally advanced lung cancer: a re-analysis of meta-analyses of individual patients' data. Lancet Oncol 2013;14:619-26. [Crossref] [PubMed]
- Inoue A, Kobayashi K, Maemondo M, et al. Updated overall survival results from a randomized phase III trial comparing gefitinib with carboplatin-paclitaxel for chemo-naïve non-small cell lung cancer with sensitive EGFR gene mutations (NEJ002). Ann Oncol 2013;24:54-9. [Crossref] [PubMed]
- Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 2010;362:2380-8. [Crossref] [PubMed]
- Mitsudomi T, Morita S, Yatabe Y, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol 2010;11:121-8. [Crossref] [PubMed]
- Yoshioka H, Shimokawa M, Seto T, et al. Final overall survival results of WJTOG3405, a randomized phase III trial comparing gefitinib versus cisplatin with docetaxel as the first-line treatment for patients with stage IIIB/IV or postoperative recurrent EGFR mutation-positive non-small-cell lung cancer. Ann Oncol 2019;30:1978-84. [Crossref] [PubMed]
- Ramalingam SS, Vansteenkiste J, Planchard D, et al. Overall Survival with Osimertinib in Untreated, EGFR-Mutated Advanced NSCLC. N Engl J Med 2020;382:41-50. [Crossref] [PubMed]
- Zhong WZ, Wang Q, Mao WM, et al. Gefitinib versus vinorelbine plus cisplatin as adjuvant treatment for stage II-IIIA (N1-N2) EGFR-mutant NSCLC (ADJUVANT/CTONG1104): a randomised, open-label, phase 3 study. Lancet Oncol 2018;19:139-48. [Crossref] [PubMed]
- Zhong WZ, Wang Q, Mao WM, et al. Gefitinib Versus Vinorelbine Plus Cisplatin as Adjuvant Treatment for Stage II-IIIA (N1-N2) EGFR-Mutant NSCLC: Final Overall Survival Analysis of CTONG1104 Phase III Trial. J Clin Oncol 2021;39:713-22. [Crossref] [PubMed]
- Tada H, Mitsudomi T, Misumi T, et al. Randomized Phase III Study of Gefitinib Versus Cisplatin Plus Vinorelbine for Patients With Resected Stage II-IIIA Non-Small-Cell Lung Cancer With EGFR Mutation (IMPACT). J Clin Oncol 2022;40:231-41. [Crossref] [PubMed]
- Goldstraw P, Chansky K, Crowley J, et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2016;11:39-51. [Crossref] [PubMed]
- Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J Thorac Oncol 2015;10:1243-60. [Crossref] [PubMed]
- Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0 [Internet]. Bethesda: US Department of Health and Human Services, National Institutes of Health, National Cancer Institute; c2023 [cited 2023 Mar 12]. Available online: https://www.cancer.gov
- Ettinger DS, Wood DE, Aisner DL, et al. Non-Small Cell Lung Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2022;20:497-530. [Crossref] [PubMed]
- Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant 2013;48:452-8. [Crossref] [PubMed]
- Cross DA, Ashton SE, Ghiorghiu S, et al. AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated resistance to EGFR inhibitors in lung cancer. Cancer Discov 2014;4:1046-61. [Crossref] [PubMed]
- Finlay MR, Anderton M, Ashton S, et al. Discovery of a potent and selective EGFR inhibitor (AZD9291) of both sensitizing and T790M resistance mutations that spares the wild type form of the receptor. J Med Chem 2014;57:8249-67. [Crossref] [PubMed]
- Igawa S, Fukui T, Kasajima M, et al. First-line osimertinib for poor performance status patients with EGFR mutation-positive non-small cell lung cancer: A prospective observational study. Invest New Drugs 2022;40:430-7. [Crossref] [PubMed]
- Takamizawa S, Okuma Y, Kato Y, et al. First-line osimertinib in EGFR mutation-positive non-small cell lung cancer patients with poor performance status. Future Oncol 2022;18:291-300. [Crossref] [PubMed]
- Teranishi S, Sugimoto C, Nagaoka S, et al. Retrospective analysis of independent predictors of progression-free survival in patients with EGFR mutation-positive advanced non-small cell lung cancer receiving first-line osimertinib. Thorac Cancer 2022;13:2741-50. [Crossref] [PubMed]
- Suda K, Mitsudomi T, Shintani Y, et al. Clinical Impacts of EGFR Mutation Status: Analysis of 5780 Surgically Resected Lung Cancer Cases. Ann Thorac Surg 2021;111:269-76. [Crossref] [PubMed]
- Xie L, Nagpal S, Wakelee HA, et al. Osimertinib for EGFR-Mutant Lung Cancer with Brain Metastases: Results from a Single-Center Retrospective Study. Oncologist 2019;24:836-43. [Crossref] [PubMed]
- Xu ST, Xi JJ, Zhong WZ, et al. The Unique Spatial-Temporal Treatment Failure Patterns of Adjuvant Gefitinib Therapy: A Post Hoc Analysis of the ADJUVANT Trial (CTONG 1104). J Thorac Oncol 2019;14:503-12. [Crossref] [PubMed]
- Rotolo F, Dunant A, Le Chevalier T, et al. Adjuvant cisplatin-based chemotherapy in nonsmall-cell lung cancer: new insights into the effect on failure type via a multistate approach. Ann Oncol 2014;25:2162-6. [Crossref] [PubMed]
- Togashi Y, Masago K, Masuda S, et al. Cerebrospinal fluid concentration of gefitinib and erlotinib in patients with non-small cell lung cancer. Cancer Chemother Pharmacol 2012;70:399-405. [Crossref] [PubMed]
- Zhao J, Chen M, Zhong W, et al. Cerebrospinal fluid concentrations of gefitinib in patients with lung adenocarcinoma. Clin Lung Cancer 2013;14:188-93. [Crossref] [PubMed]
- Jenkins S, Yang JC, Ramalingam SS, et al. Plasma ctDNA Analysis for Detection of the EGFR T790M Mutation in Patients with Advanced Non-Small Cell Lung Cancer. J Thorac Oncol 2017;12:1061-70. [Crossref] [PubMed]
- Yamaguchi H, Wakuda K, Fukuda M, et al. A Phase II Study of Osimertinib for Radiotherapy-Naive Central Nervous System Metastasis From NSCLC: Results for the T790M Cohort of the OCEAN Study (LOGIK1603/WJOG9116L). J Thorac Oncol 2021;16:2121-32. [Crossref] [PubMed]
- Ballard P, Yates JW, Yang Z, et al. Preclinical Comparison of Osimertinib with Other EGFR-TKIs in EGFR-Mutant NSCLC Brain Metastases Models, and Early Evidence of Clinical Brain Metastases Activity. Clin Cancer Res 2016;22:5130-40. [Crossref] [PubMed]
- Soria JC, Ohe Y, Vansteenkiste J, et al. Osimertinib in Untreated EGFR-Mutated Advanced Non-Small-Cell Lung Cancer. N Engl J Med 2018;378:113-25. [Crossref] [PubMed]
- Ohe Y, Imamura F, Nogami N, et al. Osimertinib versus standard-of-care EGFR-TKI as first-line treatment for EGFRm advanced NSCLC: FLAURA Japanese subset. Jpn J Clin Oncol 2019;49:29-36. [Crossref] [PubMed]
- Sakata Y, Sakata S, Oya Y, et al. Osimertinib as first-line treatment for advanced epidermal growth factor receptor mutation-positive non-small-cell lung cancer in a real-world setting (OSI-FACT). Eur J Cancer 2021;159:144-53. [Crossref] [PubMed]
- Ohmori T, Yamaoka T, Ando K, et al. Molecular and Clinical Features of EGFR-TKI-Associated Lung Injury. Int J Mol Sci 2021;22:792. [Crossref] [PubMed]
- Sato Y, Sumikawa H, Shibaki R, et al. Drug-Related Pneumonitis Induced by Osimertinib as First-Line Treatment for Epidermal Growth Factor Receptor Mutation-Positive Non-Small Cell Lung Cancer: A Real-World Setting. Chest 2022;162:1188-98. [Crossref] [PubMed]
- Imaji M, Fujimoto D, Sato Y, et al. Safety and efficacy of osimertinib rechallenge or continuation after pneumonitis: A multicentre retrospective cohort study. Eur J Cancer 2023;179:15-24. [Crossref] [PubMed]
- Kodama H, Wakuda K, Yabe M, et al. Retrospective analysis of osimertinib re-challenge after osimertinib-induced interstitial lung disease in patients with EGFR-mutant non-small cell lung carcinoma. Invest New Drugs 2021;39:571-7. [Crossref] [PubMed]
- Cumbo C, Anelli L, Specchia G, et al. Monitoring of Minimal Residual Disease (MRD) in Chronic Myeloid Leukemia: Recent Advances. Cancer Manag Res 2020;12:3175-89. [Crossref] [PubMed]
- Zhong WZ, Chen KN, Chen C, et al. Erlotinib Versus Gemcitabine Plus Cisplatin as Neoadjuvant Treatment of Stage IIIA-N2 EGFR-Mutant Non-Small-Cell Lung Cancer (EMERGING-CTONG 1103): A Randomized Phase II Study. J Clin Oncol 2019;37:2235-45. [Crossref] [PubMed]
- Abbosh C, Frankell AM, Harrison T, et al. Tracking early lung cancer metastatic dissemination in TRACERx using ctDNA. Nature 2023;616:553-62. [Crossref] [PubMed]
- Tsutani Y, Imai K, Ito H, et al. Adjuvant Chemotherapy for High-risk Pathologic Stage I Non-Small Cell Lung Cancer. Ann Thorac Surg 2022;113:1608-16. [Crossref] [PubMed]
- Tsutani Y, Goldman JW, Dacic S, et al. Adjuvant Osimertinib vs. Placebo in Completely Resected Stage IA2-IA3 EGFR-Mutated NSCLC: ADAURA2. Clin Lung Cancer 2023;24:376-80. [Crossref] [PubMed]
- Liu SY, Bao H, Wang Q, et al. Genomic signatures define three subtypes of EGFR-mutant stage II-III non-small-cell lung cancer with distinct adjuvant therapy outcomes. Nat Commun 2021;12:6450. [Crossref] [PubMed]
- Osoegawa A, Yamaguchi M, Nakamura T, et al. High Incidence of C797S Mutation in Patients With Long Treatment History of EGFR Tyrosine Kinase Inhibitors Including Osimertinib. JTO Clin Res Rep 2021;2:100191. [Crossref] [PubMed]
- Bousquet Mur E, Bernardo S, Papon L, et al. Notch inhibition overcomes resistance to tyrosine kinase inhibitors in EGFR-driven lung adenocarcinoma. J Clin Invest 2020;130:612-24. [Crossref] [PubMed]
- Takahashi H, Sakakibara-Konishi J, Furuta M, et al. Notch pathway regulates osimertinib drug-tolerant persistence in EGFR-mutated non-small-cell lung cancer. Cancer Sci 2023;114:1635-50. [Crossref] [PubMed]
- Osoegawa A, Takumi Y, Hashimoto T, et al. Cyclin-dependent kinase (CDK) 4/6 inhibition in non-small cell lung cancer with epidermal growth factor receptor (EGFR) mutations. Invest New Drugs 2023;41:183-92. [Crossref] [PubMed]


