
CT coronary artery calcification score as a prognostic marker in COVID-19
Highlight box
Key findings
• Coronary calcifications defined by computed tomography (CT) is associated with prognosis in patients with coronavirus disease 2019 (COVID-19). The coronary calcification score was associated with 30-day mortality [odds ratio =1.15; 95% confidence interval: 1.06–1.25; P<0.001].
What is known and what is new?
• Cardiovascular risk factors are known to be of prognostic relevance in patients with COVID-19.
• The present study provides the prognostic relevance of coronary calcifications quantified in CT images with a semiquantitative method.
What is the implication, and what should change now?
• The radiologist should report the severity of coronary calcifications in patients with COVID-19 in chest CT images to provide a prognostic imaging finding.
Introduction
The ongoing coronavirus disease 2019 (COVID-19) pandemic is still globally to this date.
The symptomatology of infected patients is highly variable. Early on in the first wave of the pandemic, it became evident that most patients only have a mild disease course. Yet, a minority of patients can rapidly suffer from severe or critical illness, leading to the admission to intensive care unit or even fatal outcome (1-4). Consequently, the frequency of fatal cases was over 10% in most European countries during the first wave of the pandemic (2). It seems plausible that correct and early prediction of an unfavorable course of COVID-19 can be crucial for patient care (2). Previously identified prognostic factors are older age than 60 years and male sex with hazard ratios of 2.6 for age of 60 years and above and 1.4 for male sex, respectively (5,6). Notably, a short time period between onset of the symptoms and admission to the hospital was also a risk factor. Important comorbidities include cardiovascular diseases comprising chronic heart failure and peripheral vascular disease are also clinical predictors of an unfavorable course (6).
Computed tomography (CT) plays an important role in the diagnostic work up for COVID-19, especially in detection of pulmonary consolidations (7-11). It is acquired without contrast media application, preferably in low-dose technique. Very early during the course of the pandemic, typical, yet unspecific imaging findings for COVID-19 were identified and rapidly reported in the literature (4). Typically described finding comprise peripheral ground-glass opacities involving both lungs (2,12). Other reported imaging signs were vascular enlargement, lower lobe and posterior predilection. In more severe cases, there were also consolidations in the affected lung lobes.
Coronary artery calcification (CA) scoring is commonly utilized to quantify the number of calcified regions of the coronary vessels. The involvement of calcified vessels harbors prognostic relevance especially in patients with coronary heart disease (13-16). Thus, there was a strong association between CA score and major cardiovascular events in asymptomatic individuals, which highlighted this imaging finding in the literature (13-16).
Moreover, CA was also shown to be a good predictor of general vessel status, which could also be of prognostic relevance in patents with COVID-19, as COVID-19 can also induce cardiac injury. Yet, there are is only few reliable data in patients with COVID-19 regarding the prognostic relevance of CA scoring. Moreover, the widely used Agatston score is calculated on cardiac-gated CT images but the more recently developed Weston score can be semiquantitatively calculated on non-gated CT images and, therefore, can be obtained by routine chest CT images, which are used to image patients with COVID-19 (16).
Therefore, the rationale of the present analysis was to investigate the possible prognostic role of CA score in patients with COVID-19. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-728/rc).
Methods
Acquisition of the patient sample
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The retrospective analysis was approved by the Ethics Committee of Otto von Guericke University Magdeburg, Magdeburg, Germany (No. 25/21). Individual consent for this retrospective analysis was waived.
All consecutive patients from the University Hospital of Otto von Guericke University Magdeburg with polymerase chain reaction (PCR)-proven COVID-19 were analyzed between March 2020 and December 2022.
As inclusion criteria were defined: sufficient CT images at the time point of the hospital admission; available clinical data regarding clinical signs, serological parameters and follow up.
Exclusion artifacts were: severe image artifacts, especially at the level of the heart.
Overall, 241 patients (85 female patients, 35.3%) were included into the present study. The median age was 64 years, ranging from 18 to 93 years. The primary end point of the study was the impact of CA on 30-day mortality after diagnosis of COVID-19.
Imaging technique
CT was performed at the time point of the hospital admission for every case without any form of previous treatment.
CT imaging was acquired during clinical routine on a multidetector CT scanner (Siemens Somatom Definition AS+; Siemens Healthcare, Erlangen, Germany). At the beginning of the pandemic, the CT scanner was solely used for patients suspected or confirmed of COVID-19. The CT protocol the following technical parameters: slice thickness 1 mm with 5 mm reconstructions, tube voltage 120 kV, automatic tube current modulation, pitch factor 1.2, and collimation 0.6 mm. Figure 1 provides representative cases of the investigated cohort for illustration purposes.

CA scoring
Weston scoring was performed by an experienced radiologist with 7 years of experience in cardiovascular radiology. The four coronary arteries comprising of the left main, the left anterior descending, left circumflex and right coronary artery were each scored for the amount of calcification of the vessel. For this purpose, a 4-point scale was used ranging from 0= no calcification to 3= extensive calcifications indicated by blooming artefacts. The exact score was described in detail previously (17). The score can therefore range from 0 to 12.
Statistical analysis
SPSS (IBM SPSS Statistics for Windows. version 225.0: IBM corporation, Armonk, NY, USA) and GraphPad Prism 5 (GraphPad Software, La Jolla, CA, USA) were utilized for the statistics. The figures were created with GraphPad Prism 5 Collected data were first evaluated by means of descriptive statistics). Spearman’s correlation coefficient (r) was performed to elucidate the associations between the CA score and the clinical parameters. Group differences were calculated with Mann-Whitney test and Fisher exact test, when suitable. Uni- and multivariable logistic regression analyses were conducted to identify the associations between CA scoring with 30-day mortality. Receiver operating characteristics (ROC) analysis was performed to elucidate the diagnostic accuracy. The threshold of a P value below <0.05 was used to demonstrate statistical significance.
Results
Clinical signs and scores
Overall, 61 patients (25.3%) of the patient sample died within the 30-day period. Table 1 provides an overview between survivors and non-survivors.
Table 1
| Parameter | Survivors (n=180) | Non-survivors (n=61) | P value |
|---|---|---|---|
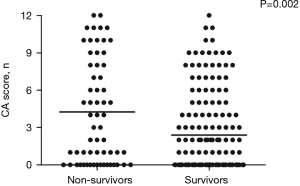
| CA score | 2.3±3.0 | 4.2±4.1 | 0.002 |
| Age (years) | 62.8±15.7 | 65.9±14.2 | 0.2 |
| Gender (female) | 62 | 23 | 0.77* |
| Need for intubation | 60 | 55 | <0.0001* |
| Intubation duration (hour) | 182.4±344.2 | 376.0±311.9 | <0.0001 |
| Need for ICU admission | 88 | 54 | 0.01* |
Data are presented as mean ± standard deviation or number. *, Fisher’s exact test. CA, coronary artery calcification; ICU, intensive care unit.
In survivors, the mean CA score was 2.3±3.0 and in non-survivors, it was 4.2±4.1, P=0.002 (Figure 2). CA score correlated with age (r=0.55, P<0.0001, Figure 3).
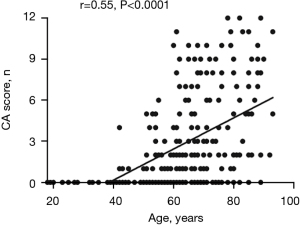
Furthermore, there was a weak inverse correlation between CA score and duration of intubation (r=−0.14, P=0.03).
Overall, 94 patients (41.1%) had no presence of calcifications (CA score of 0). In this group, 17 patients died (18.1%). In the group with calcification in the coronary vessels (n=147, 58.9%), 43 patients died (29.3%). There was no difference regarding 30-day mortality between these groups (P=0.13).
However, CA score was associated with 30-day mortality [odds ratio (OR) =1.15; 95% confidence interval (CI): 1.06–1.25; P<0.001; Table 2]. This remained statistically significant in multivariable regression analysis adjusted for age and sex with CA score influencing 30-day mortality (OR =1.28; 95% CI: 1.08–1.4, P=0.002; Table 2).
Table 2
| Parameter | Univariable | Multivariable | |||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | ||
| CA score | 1.15 | 1.06–1.25 | <0.001 | 1.28 | 1.08–1.4 | 0.002 | |
| Age | 1.01 | 0.99–1.03 | 0.17 | 1.009 | 0.98–1.04 | 0.58 | |
| Gender | 1.1 | 0.61–2.0 | 0.70 | 1.2 | 0.55–2.61 | 0.63 | |
| Need for intubation | 18.0 | 7.3–44.2 | <0.001 | 62.1 | 7.1–541.3 | <0.001 | |
| Intubation duration (h) | 1.001 | 1.0–1.002 | 0.01 | 1.0 | 0.99–1.01 | 0.49 | |
| Need for ICU admission | 8.0 | 3.4–18.6 | <0.001 | 0.48 | 0.05–4.0 | 0.48 | |
OR, odds ratio; CI, confidence interval; CA, coronary artery calcification; ICU, intensive care unit.
CA score was not associated with ICU admission with an OR of 0.96 (95% CI: 0.89–1.03, P=0.31) and with need for intubation with an OR of 0.98 (95% CI: 0.91–1.05, P=0.38).
ROC analysis
The diagnostic accuracy for CA scoring to predict 30-day mortality was elucidated by ROC analysis. The AUC was 0.62 (95% CI: 0.54–0.71). Employing a threshold value for the CA of 3, a sensitivity of 0.49 with a specificity of 0.74 was achieved.
Discussion
Risk stratification is crucial for patients with COVID-19 in clinical care. Several clinical parameters and different scores were investigated and employed to predict an unfavorable course and mortality in patients with COVID-19 (2,5,6).
During the first months of the pandemic, it was shown that cardiovascular disorders, especially coronary heart disease are risk factors for an unfavorable course of COVID-19 (18).
The present analysis can corroborate these predominantly clinical anamnestic based studies with the significant association between coronary calcification quantified on CT image as an imaging biomarker of coronary heart disease. However, it should be acknowledged that there are also patients with coronary heart disease with no calcified plaques, which are not detected by the current analysis.
That is why the diagnostic gold standard of coronary stenosis is the contrast enhanced cardiac-gated CT imaging.
However, an important aspect of the present study is that the sole presence of calcified plaques identified on CT image can be predictive for an unfavorable outcome in patients with COVID-19. Moreover, it has been shown that plaque quantification is more sensitive to predict unfavorable outcome than only the sole presence of calcification in a stratified manner (19,20). This can be underlined by the present results.
A previous meta-analysis could already demonstrate the clinical importance of coronary artery calcifications in patients with COVID-19 (21). In this analysis, the data of 5 studies comprising 3,500 patients were investigated and reported an OR of 2.68 (95% CI: 1.78–4.04) (21). Noteworthy, the included patients were of the first wave of the pandemic with a different severity course and outcomes compared to the recent days and the presented results in this study.
Another recent meta-analysis reported an OR of 2.19 (95% CI: 1.36–3.52) for the effect of detectable coronary calcifications on mortality based upon 2,875 patients (22).
The importance of CA scoring was also demonstrated in other diseases.
Until recently, only cardiac-gated CT studies were solely used and investigated for quantification of CA. Due to advances in technology including larger numbers of detectors and faster gantry speeds in current CT scanners, even non-gated studies can provide either semiquantitative scores as the investigated Weston score and even quantitative CA, similar to the established Agatston scoring (17). This was demonstrated by high correlations with cardiac CT gated CT images and was also associated with relevant cardiovascular disease outcomes (17). This is the rationale, why the analysis used in the present study can be assumed as reliable. Notably, this allows to use the low dose CTs performed for the detection of infectious foci in patients with COVID-19 to provide a prognostic imaging marker as a by-product.
The possible prognostic benefit of CA scoring beyond the anamnestic presence of cardiovascular diseases was demonstrated in several analyses (22-26).
One strength of the present CA scoring is that is semiquantitatively and easily performed in clinical routine. Compared to the standard Agatston score, there is no need for cardiac gated CT, which is not routinely performed for thoracic CT in patients with COVID-19.
Presumably, the inclusion of CA scoring into the proposed risk scores should be further investigated in multivariable analyses. In the current state, the severe overlap between the patient groups cannot justify the benefit in clinical routine.
Notably, even if CA score can be considered as a prognostic imaging marker, it could not change the management of the patient. To this date, a patient with high calcification status of the coronary arteries could not be treated differently compared to a patient with no calcifications.
The present analysis is not free from limitations. First, it is a retrospective study with possible known inherent bias. However, the reader was blinded to the clinical outcome to reduce possible bias. Second, the patient sample is relatively small caused by the single center design. Noteworthy, there might be selection bias, which can have an influence of the present results, as patients without the need for hospital admission were not included into the present analysis. Notably, the present patient sample has a relatively high mortality rate compared to other reported patient samples. Therefore, the identified associations might not transferrable to patient samples with a lower mortality rate. Third, the CA scoring was performed on non-cardiac gated CT. The gold standard is the Agatston score calculated on cardiac gated CT. However, the Weston score, which was used in the present study is highly correlated with this established score and is considered almost as reliable as the Agatston score (17). Moreover, the reading was performed by one radiologist without a test for interreader variability. However, it was shown in previous analyses that the Weston score has low interreader variability, which reduces this limitation of the present work (17). Forth, the patient history for known coronary heart disease and metabolic diseases was not available for all patients. Therefore, we could not address for this factor in the multivariable analysis. It remains elusive, whether CA scoring adds prognostic relevance beyond the anamnestic presence of CA scoring in patients with COVID-19.
Conclusions
CA score derived from native CT images was associated with 30-day mortality in patients with COVID-19. However, the identified overlap between the patient groups might be too large for translation into clinical routine. Therefore, CA scoring should be further investigated as a potential imaging marker in patients with COVID-19.
Acknowledgments
Funding: This research was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-728/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-728/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-728/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-728/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chopra V, Flanders SA, Vaughn V, et al. Variation in COVID-19 characteristics, treatment and outcomes in Michigan: an observational study in 32 hospitals. BMJ Open 2021;11:e044921. [Crossref] [PubMed]
- Besutti G, Ottone M, Fasano T, et al. The value of computed tomography in assessing the risk of death in COVID-19 patients presenting to the emergency room. Eur Radiol 2021;31:9164-75. [Crossref] [PubMed]
- Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020;323:1061-9. Erratum in: JAMA 2021;325:1113. [Crossref] [PubMed]
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497-506. [Crossref] [PubMed]
- Liu B, Spokes P, He W, et al. High risk groups for severe COVID-19 in a whole of population cohort in Australia. BMC Infect Dis 2021;21:685. [Crossref] [PubMed]
- Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect 2020;81:e16-25. [Crossref] [PubMed]
- Azevedo RB, Botelho BG, Hollanda JVG, et al. Covid-19 and the cardiovascular system: a comprehensive review. J Hum Hypertens 2021;35:4-11. [Crossref] [PubMed]
- Kwee TC, Kwee RM. Chest CT in COVID-19: What the Radiologist Needs to Know. Radiographics 2020;40:1848-65. [Crossref] [PubMed]
- Salehi S, Abedi A, Balakrishnan S, et al. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol 2020;215:87-93. [Crossref] [PubMed]
- Li K, Wu J, Wu F, et al. The Clinical and Chest CT Features Associated With Severe and Critical COVID-19 Pneumonia. Invest Radiol 2020;55:327-31. [Crossref] [PubMed]
- Harrison EA, Wu JW. Vaccine confidence in the time of COVID-19. Eur J Epidemiol 2020;35:325-30. [Crossref] [PubMed]
- Pan F, Yang L, Liang B, et al. Chest CT Patterns from Diagnosis to 1 Year of Follow-up in Patients with COVID-19. Radiology 2022;302:709-19. [Crossref] [PubMed]
- Tramontano L, Punzo B, Clemente A, et al. Prognostic Value of Coronary Calcium Score in Asymptomatic Individuals: A Systematic Review. J Clin Med 2022;11:5842. [Crossref] [PubMed]
- Agha AM, Pacor J, Grandhi GR, et al. The Prognostic Value of CAC Zero Among Individuals Presenting With Chest Pain: A Meta-Analysis. JACC Cardiovasc Imaging 2022;15:1745-57. [Crossref] [PubMed]
- Maniar Y, Blumenthal RS, Alfaddagh A. The role of coronary artery calcium in allocating pharmacotherapy for primary prevention of cardiovascular disease: The ABCs of CAC. Clin Cardiol 2022;45:1107-13. [Crossref] [PubMed]
- Hecht HS, Cronin P, Blaha MJ, et al. 2016 SCCT/STR guidelines for coronary artery calcium scoring of noncontrast noncardiac chest CT scans: A report of the Society of Cardiovascular Computed Tomography and Society of Thoracic Radiology. J Cardiovasc Comput Tomogr 2017;11:74-84. [Crossref] [PubMed]
- Kirsch J, Buitrago I, Mohammed TL, et al. Detection of coronary calcium during standard chest computed tomography correlates with multi-detector computed tomography coronary artery calcium score. Int J Cardiovasc Imaging 2012;28:1249-56. [Crossref] [PubMed]
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054-62. [Crossref] [PubMed]
- Giannini F, Toselli M, Palmisano A, et al. Coronary and total thoracic calcium scores predict mortality and provides pathophysiologic insights in COVID-19 patients. J Cardiovasc Comput Tomogr 2021;15:421-30. [Crossref] [PubMed]
- Scoccia A, Gallone G, Cereda A, et al. Impact of clinical and subclinical coronary artery disease as assessed by coronary artery calcium in COVID-19. Atherosclerosis 2021;328:136-43. [Crossref] [PubMed]
- Meyer HJ, Wienke A, Surov A, Extrapulmonary CT. Findings Predict In-Hospital Mortality in COVID-19. A Systematic Review and Meta-Analysis. Acad Radiol 2022;29:17-30.
- Cereda A, Allievi L, Palmisano A, et al. Systematic review and meta-analysis on coronary calcifications in COVID-19. Emerg Radiol 2022;29:631-43. [Crossref] [PubMed]
- Hollenberg EJ, Lin F, Blaha MJ, et al. Relationship Between Coronary Artery Calcium and Atherosclerosis Progression Among Patients With Suspected Coronary Artery Disease. JACC Cardiovasc Imaging 2022;15:1063-74. [Crossref] [PubMed]
- Vakil P, Wen Z, Lima AS, et al. Predictive Value of Coronary Artery Calcium in Patients Receiving Computed Tomography Pulmonary Angiography for Suspected Pulmonary Embolism in the Emergency Department. J Thorac Imaging 2022;37:279-84. [Crossref] [PubMed]
- Jacobs PC, Gondrie MJ, Mali WP, et al. Unrequested information from routine diagnostic chest CT predicts future cardiovascular events. Eur Radiol 2011;21:1577-85. [Crossref] [PubMed]
- Lehker A, Mukherjee D. Coronary Calcium Risk Score and Cardiovascular Risk. Curr Vasc Pharmacol 2021;19:280-4. [Crossref] [PubMed]


