
Video-assisted thoracic surgery drainage is feasible and safe for acute necrotizing mediastinitis: a retrospective cohort study
Highlight box
Key findings
• Video-assisted thoracic surgery (VATS) and thoracotomy showed comparable postoperative outcomes, including in blood transfusion, duration of postoperative drainage, length of antibiotic medication, admission to intensive care unit (ICU), length of ICU stay, and postoperative hospital stay, reoperation rate, and mortality.
What is known and what is new?
• Thoracotomy is the traditional approach for treating acute necrotizing mediastinitis (ANM), but VATS is being increasingly used in patients with this condition. However, which approach is more effective remains controversial.
• Our research showed that VATS and open approach had comparable outcomes for the treatment of ANM.
What is the implication, and what should change now?
• This study demonstrated that VATS is a feasible option for the treatment of patients with ANM.
Introduction
Acute necrotizing mediastinitis (ANM), also known as mediastinal abscess, is a severe infection of the mediastinal loose connective tissue. Descending necrotizing mediastinitis (DNM), originating from the oropharynx and neck, is the most common type of ANM. However, ANM can be caused by infections from sites other than the oral cavity and neck, such as the esophagus, lungs, and sternum. The mortality rate among patients with ANM remains high (1-3) due to delayed diagnosis and inadequate drainage of the abscess (3-10). Surgical drainage, comprising the cervical and thoracic approach, is the most important component of treatment for these patients. The choice between cervical and thoracic operation depends on the level of abscess invasion. If the abscess involves the inferior mediastinum, the thoracic approach is usually recommended for surgical drainage (1,11,12), and thoracotomy is the most commonly used approach for treating ANM involving the inferior mediastinum. However, with the development of video-assisted thoracic surgery (VATS), numerous diseases are now being treated with VATS. There was one study which compared thoracotomy and VATS for treating patients with DNM (13), but there is no accepted consensus concerning which approach is preferred. We thus collected the data of patients with ANM treated with surgery over a 9-year period at our center and compared the outcomes of VATS-treated patients with those of thoracotomy-treated patients. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-845/rc).
Methods
Patients
The study was approved by the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University (approval No. 2021-1420) and was conducted in accordance with the Declaration of Helsinki (as revised in 2013) (14). All the data of patients were provided anonymously, and informed consent was waived due to the retrospective nature of the study.
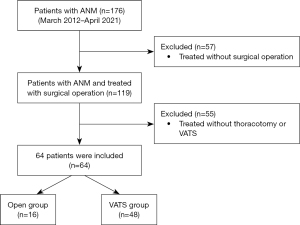
We retrospectively reviewed the medical records of patients treated in West China Hospital between March 2012 and April 2021. The data were obtained from the West China Hospital big data platform (WCH-BDP) (15). Our study included all patients (I) diagnosed with ANM and (II) treated with VATS or open thoracotomy, and excluded those (I) treated without surgery or (II) treated with the cervical approach or other surgical procedures. The selection flow diagram for the study population is shown in Figure 1.
Clinical procedures
Patients were diagnosed with ANM based on the following criteria: (I) relevant clinical history, such as a history of cervical, odontogenic, or thoracic infection, or of esophageal perforation due to a foreign body; (II) clinical manifestations of severe infection, such as fever, pharyngalgia, chest pain, or symptoms of septic shock; and (III) formation of a mediastinal abscess on a cervicothoracic computed tomography (CT) scan. Broad-spectrum antibiotics were administered once the mediastinal abscess was diagnosed, and the antibiotic administration was adjusted based on treatment outcomes and bacterial susceptibility testing. Thoracic surgical indications were summarized as follows: (I) patients with severe infection; (II) formation of an encapsulated abscess; and (III) an abscess involving the inferior mediastinum or combined with acute empyema. Because surgery for ANM is considered to be an emergency operation, the decision between thoracotomy and VATS was based on the individual preferences of the thoracic surgeons on duty.
In preparation for surgery, the patients were placed in a lateral decubitus position, with double-lumen endotracheal intubation being used with general anesthesia. For those patients with previous tracheal intubation or tracheotomy, a blocker was used for single-lung ventilation. Open thoracotomy was carried out in the fourth or fifth intercostal spaces. The VATS approach included a 1-cm incision for the thoracoscope in the seventh intercostal space on the midaxillary line, a 3-cm utility incision on the anterior axillary line in the third or fourth intercostal space, and a 2-cm assistant incision in the ninth intercostal space (between the posterior axillary line and scapular line). Subsequently, both thoracotomy and VATS involved excision of infected tissues and pleura, adequate flushing with normal saline or povidone-iodine after opening of the abscess cavity. Usually, two 28-French (Fr) silicone drainage tubes were placed after surgery, one in the abscess cavity and the other in the chest. The abscess was collected and sent for bacterial and fungal culture during the operation. After the operation, enhanced cervicothoracic CT was performed to assess the presence of newly formed abscesses if the patients had recurrent fever with increased white blood cell count or signs of deteriorative infective shock. Once an abscess was again detected with CT, a reoperation was scheduled via a multidisciplinary discussion.
Data collection
The study collected patients’ general information, including age, sex, smoking history, alcohol consumption, comorbidity, etiology, and abscess involvement. Comorbidity data included hypertension, coronary heart disease, diabetes, cerebrovascular disease, and autoimmune disease. Data on perioperative variables, including use of cervical approach, operation side, sputum, and secretion culture, and treatment outcomes, including blood transfusion, duration of postoperative drainage, length of antibiotic medication, admission to the intensive care unit (ICU), length of ICU stay, length of hospital stay, reoperation rate, postoperative complications, and hospital mortality were collected. Mortality was defined as death during the hospital stay.
Statistical analyses
Patients were divided into two groups based on whether they had undergone VATS (VATS group) or open thoracotomy (Open group). Normally distributed continuous variables are expressed as the mean ± standard deviation and were compared with the Student t-test. Abnormally distributed continuous variables are expressed as the median and range and were compared with the Wilcoxon signed-rank test. Differences between categorical variables were evaluated using the chi-squared test. All statistical analyses were conducted using SPSS version 22.0 (IBM Corp., Armonk, NY, USA).
Results
Our study ultimately included 64 patients, comprising 42 males (65.6%) and 22 females (34.4%). In the study population, the distribution of infection origin was as follows: from the neck in 26 patients (40.6%), from perforation due to a esophageal foreign body in 16 patients (25.0%), odontogenic infection in 15 patients (23.4%), thoracic infections in 3 patients (4.7%), and other sources of infections in 4 patients (6.3%). The most frequent symptoms reported were fever (57.8%), cervical swelling (35.9%), cervical pain (35.9%), pharyngalgia (34.4%), and dysphagia (32.8%) (Figure 2). The superior mediastinum was the most frequently affected area (85.9%), followed by the posterior mediastinum (78.1%). There were 16 patients in the Open group and 48 in the VATS group. Additionally, 37 patients (57.8%) underwent simultaneous cervical drainage. There were more patients with esophageal perforation in the Open group (50.0% vs. 16.7%; P=0.02) than in the VATS group. The detailed information of these patients is listed in Table 1.
Table 1
| Variables | VATS (n=48) | Thoracotomy (n=16) | P value |
|---|---|---|---|
| Age (years) | 48.9±12.2 | 45.1±20.4 | 0.49 |
| Gender | 0.36 | ||
| Male | 33 (68.8) | 9 (56.3) | |
| Female | 15 (31.3) | 7 (43.8) | |
| Smoking | 14 (29.2) | 3 (18.8) | 0.62 |
| Alcohol | 14 (29.2) | 6 (37.5) | 0.53 |
| Comorbidity | |||
| Diabetes | 7 (14.6) | 3 (18.8) | >0.99 |
| Hypertension | 6 (12.5) | 3 (18.8) | 0.84 |
| Previous neoplastic diseases | 2 (4.2) | 1 (6.3) | >0.99 |
| Etiology | |||
| Neck infection | 22 (45.8) | 4 (25.0) | 0.14 |
| Esophageal perforation | 8 (16.7) | 8 (50.0) | 0.02 |
| Odontogenic infection | 13 (27.1) | 2 (12.5) | 0.39 |
| Thoracic infection | 1 (2.1) | 2 (12.5) | 0.31 |
| Others | 4 (8.3) | 0 (0.0) | 0.42 |
| Abscess involvement | >0.99 | ||
| Superior mediastinum | 1 (2.1) | 0 (0.0) | |
| Inferior mediastinum | 5 (10.4) | 2 (12.5) | |
| Superior and inferior mediastinum | 42 (87.5) | 14 (87.5) | |
| With or without cervical approach | 0.19 | ||
| Yes | 30 (62.5) | 7 (43.8) | |
| No | 18 (37.5) | 9 (56.3) | |
| Operation side | >0.99 | ||
| Left | 5 (10.4) | 2 (12.5) | |
| Right | 41 (85.4) | 14 (87.5) | |
| Bilateral | 2 (4.2) | 0 (0.0) | |
| Sputum and secretion culture | 0.31 | ||
| Negative | 20 (41.7) | 9 (56.3) | |
| Positive | 28 (58.3) | 7 (43.8) | |
Data are shown as mean ± SD or n (%). VATS, video-assisted thoracic surgery; SD, standard deviation.
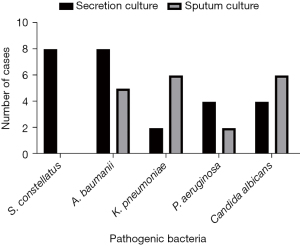
A total of 35 patients (54.7%) had positive sputum and/or positive secretion cultures. In sputum bacterial culture, the most common pathogens were Klebsiella pneumoniae (6 patients) and Acinetobacter baumannii (A. baumannii) (5 patients). In secretion cultures, the most frequent pathogens were Streptococcus constellatus (S. constellatus) (8 patients) and A. baumannii (8 patients). In fungal cultures, Candida albicans represented the most common pathogen in both secretion culture (4 patients) and sputum culture (6 patients) (Figure 3).
The treatment outcomes were compared between the VATS group and Open group, which included parameters like blood transfusion (33.3% vs. 43.8%; P=0.45), postoperative drainage {14 [1–47] vs. 17 [4–54] days; P=0.15}, days on antibiotics {14.5 [1–54] vs. 18 [4–54] days; P=0.29}, ICU stays {5 [1–58] vs. 8.5 [1–37] days; P=0.20}, postoperative hospital stays {17 [2–61] vs. 21 [5–56] days; P=0.22}, reoperation rate (12.5% vs. 6.25%; P=0.82), mortality rate (14.6% vs. 12.5%, P>0.99), and complications. The complications consisted of pneumonia (58.3% vs. 31.3%; P=0.06), electrolyte disturbance (33.3% vs. 6.3%; P=0.07), pleural effusion (31.3% vs. 25.0%; P=0.87), venous thrombosis (25.0% vs. 12.5%; P=0.49), sepsis (33.3% vs. 6.3%; P=0.07), and atelectasis (10.4% vs. 6.3%; P>0.99). Postoperative outcomes were similar between the VATS group and the Open group (Table 2).
Table 2
| Perioperative outcome | VATS (n=48) | Thoracotomy (n=16) | P value |
|---|---|---|---|
| Blood transfusion | 0.45 | ||
| Yes | 16 (33.3) | 7 (43.8) | |
| No | 32 (66.7) | 9 (56.3) | |
| Duration of postoperative drainage (days) | 14 [1–47] | 17 [4–54] | 0.15 |
| Length of antibiotic medication (days) | 14.5 [1–54] | 18 [4–54] | 0.29 |
| Admission to ICU | 0.43 | ||
| Yes | 42 (87.5) | 12 (75.0) | |
| No | 6 (12.5) | 4 (25.0) | |
| ICU stay (days) | 5 [1–58] | 8.5 [1–37] | 0.20 |
| Postoperative hospital stay (days) | 17 [2–61] | 21 [5–56] | 0.22 |
| Reoperation rate | 6 (12.5) | 1 (6.25) | 0.82 |
| Complication | |||
| Pneumonia | 28 (58.3) | 5 (31.3) | 0.06 |
| Electrolyte disturbance | 16 (33.3) | 1 (6.3) | 0.07 |
| Pleural effusion | 15 (31.3) | 4 (25.0) | 0.87 |
| Venous thrombosis | 12 (25.0) | 2 (12.5) | 0.49 |
| Sepsis | 16 (33.3) | 1 (6.3) | 0.07 |
| Atelectasis | 5 (10.4) | 1 (6.3) | >0.99 |
| Mortality | 7 (14.6) | 2 (12.5) | >0.99 |
Data are shown as median [range] or n (%). VATS, video-assisted thoracic surgery; ICU, intensive care unit.
Discussion
In this study, a total of 64 patients with ANM were enrolled, with 48 in the VATS group and 16 in the OPEN group. The most common origin of infection was the neck. The results showed that thoracotomy was more frequently chosen for patients with esophageal perforation. The postoperative outcomes of the two groups were compared, and it was found that these outcomes were similar between the two groups, which was consistent with a previous report (13).
ANM is a severe thoracic infection that despite advancements in medical imaging, intravenous antibiotics, and surgical procedures, has a high mortality rate (16). This may be attributed to the delayed diagnosis of ANM and invasion into the vital structures of the mediastinum. Moreover, symptoms of ANM are nonspecific at initiation, as ANM often starts with cough, fever, or may even be asymptomatic. By the time patients are admitted to the hospital, they are often in poor physical condition with a severe infection (17). Therefore, physicians should carefully review patients’ medical history, physical examination, and imaging examinations to accurately identify mediastinal abscess. Patients should be asked about characteristic clinical manifestations such as cervical swelling, cervical pain, and dysphagia (18). Among the imaging examinations, contiguous cervicothoracic CT is considered as the most reliable and accurate method for diagnosis. Fluid density, the presence of gas bubbles in soft tissue, and increased density of the fat and cellulitis are typical signs of infection (19). CT can not only detect infections and abscesses at an early stage but can also guide surgical approaches. Therefore, CT is recommended for all patients with suspected mediastinal abscess.
For newly admitted patients, initiating intravenous antibiotic therapy as soon as ANM is diagnosed is essential. The sensitivity test of pathogens can provide important guidance for subsequent antibiotic use. Our study found that the most frequent pathogens were S. constellatus and A. baumannii, while in a study for patients with DNM, the dominant species were Prevotella oris and S. constellatus (20). Therefore, collection of multiple abscess samples during surgery is recommended to identify the causative pathogens. Additionally, after the surgery, it is advised to collect repeated sputum samples. Aggressive surgical drainage is recommended in almost all cases because if an abscess in the mediastinum is not adequately drained, it is extremely difficult to control infection intravenously (12). Based on our experiences, the surgical approach should be carefully selected based on cervical and chest CT scans. Various approaches for mediastinal drainage have been reported, such as transcervical, subxiphoid, clamshell incision, video-assisted mediastinoscopic drainage, thoracotomy, and VATS (9,10,21,22).
For mediastinum drainage, the most suitable surgical approach remains controversial. Posterolateral thoracotomy is the most commonly used surgery for mediastinal abscess drainage (23-25). The VATS approach was firstly described to treat ANM in 1997 (26). However, in our center, thoracotomy is more commonly chosen for patients with esophageal perforation. The reason for this may be that thoracic surgeons need a wide operating space for repairing the esophagus and ensuring hemostasis. Other researchers have also argued that the dissection of infected tissues via thoracoscopy may not be as complete as that performed via thoracotomy, as the surgical field and operating space are wider in thoracotomy (8,27). Previous studies have examined various indicators, such as blood transfusion, drainage days, and the length of hospital stays to compare the relative advantages and disadvantages of the two approaches. In patients with lung cancer, it is widely accepted that VATS requires fewer drainage days and days in hospital compared to thoracotomy (5,9,26,28). In our study, complications, postoperative drainage days, and hospital stay length were similar between the two groups. This may be explained by the fact that ANM is a severe infectious disease. Thorough clearance of the necrotic tissues and effective drainage are essential for the treatment of ANM. It has been argued that thoracotomy offers the broadest exposure, allowing surgeons to place their hands into the chest to perform blunt dissection of the abscess and thoroughly drain the abscess (8,27). These abovementioned issues may limit the value of VATS. Moreover, in our study, the reoperation and mortality rate were not significantly different between the two groups, suggesting that VATS was equally effective as thoracotomy in treating ANM. Furthermore, although VATS has the advantages of a smaller wound and a magnified surgical field, it is relatively difficult to dissect a severe adhesion under thoracoscopy. Additionally, patients with septic shock cannot tolerate single-lung ventilation for an extended period of time, and thus intermittent single-lung ventilation during the surgery may be preferable.
VATS has been found to reduce postoperative pain (29,30) and better preserve pulmonary function and shoulder function (31,32), resulting in faster recovery and improved tolerance among older adults and critically ill patients, especially those with sepsis (33). Therefore, when combined with careful preoperative evaluation via CT scanning and meticulous clearance and effective drainage during the surgical procedure, VATS can be considered a feasible and safe option for ANM.
Several limitations to this study should be mentioned. First, the retrospective design of the study limits the definitiveness of our conclusions. ANM is a rare and lethal disease, and so it was difficult for us to conduct a prospective study. Furthermore, the choice of the surgical procedure was influenced by the personal preferences of the surgeons, and with the advancements in VATS, it has become a more commonly used approach. As a result, the sample size of patients who underwent thoracotomy was relatively small, which might have introduced some statistical bias. Finally, our study lacked long-term follow-up data.
Conclusions
ANM is a rare but lethal condition, and aggressive treatment, including open or minimally invasive cervical and thoracic operation, is often necessary. In this retrospective cohort study, VATS had comparable outcomes to thoracotomy. Therefore, VATS should be considered in the armamentarium of treatment modalities, offering these critically ill patients the advantages of a minimally invasive approach.
Acknowledgments
We thank Ms. Mi-Ye Wang, staff of the Big Data Center, West China Hospital, Sichuan University, for her help in preparing the data.
Funding: This study was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-845/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-845/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-845/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-845/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University (approval No. 2021-1420). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Estrera AS, Landay MJ, Grisham JM, et al. Descending necrotizing mediastinitis. Surg Gynecol Obstet 1983;157:545-52.
- Chen KC, Chen JS, Kuo SW, et al. Descending necrotizing mediastinitis: a 10-year surgical experience in a single institution. J Thorac Cardiovasc Surg 2008;136:191-8. [Crossref] [PubMed]
- Freeman RK, Vallières E, Verrier ED, et al. Descending necrotizing mediastinitis: An analysis of the effects of serial surgical debridement on patient mortality. J Thorac Cardiovasc Surg 2000;119:260-7. [Crossref] [PubMed]
- Endo S, Murayama F, Hasegawa T, et al. Guideline of surgical management based on diffusion of descending necrotizing mediastinitis. Jpn J Thorac Cardiovasc Surg 1999;47:14-9. [Crossref] [PubMed]
- Isowa N, Yamada T, Kijima T, et al. Successful thoracoscopic debridement of descending necrotizing mediastinitis. Ann Thorac Surg 2004;77:1834-7. [Crossref] [PubMed]
- Lavini C, Natali P, Morandi U, et al. Descending necrotizing mediastinitis. Diagnosis and surgical treatment. J Cardiovasc Surg (Torino) 2003;44:655-60.
- Mora R, Jankowska B, Catrambone U, et al. Descending necrotizing mediastinitis: ten years' experience. Ear Nose Throat J 2004;83:774-776-80.
- Papalia E, Rena O, Oliaro A, et al. Descending necrotizing mediastinitis: surgical management. Eur J Cardiothorac Surg 2001;20:739-42. [Crossref] [PubMed]
- Min HK, Choi YS, Shim YM, et al. Descending necrotizing mediastinitis: a minimally invasive approach using video-assisted thoracoscopic surgery. Ann Thorac Surg 2004;77:306-10. [Crossref] [PubMed]
- Shimizu K, Otani Y, Nakano T, et al. Successful video-assisted mediastinoscopic drainage of descending necrotizing mediastinitis. Ann Thorac Surg 2006;81:2279-81. [Crossref] [PubMed]
- Marty-Ané CH, Berthet JP, Alric P, et al. Management of descending necrotizing mediastinitis: an aggressive treatment for an aggressive disease. Ann Thorac Surg 1999;68:212-7. [Crossref] [PubMed]
- Wheatley MJ, Stirling MC, Kirsh MM, et al. Descending necrotizing mediastinitis: transcervical drainage is not enough. Ann Thorac Surg 1990;49:780-4. [Crossref] [PubMed]
- Tanaka Y, Maniwa Y, Sugio K, et al. The efficacy of thoracoscopic surgery for descending necrotizing mediastinitis. Interdiscip Cardiovasc Thorac Surg 2023;36:ivad053. [Crossref] [PubMed]
- World Medical Association Declaration of Helsinki. ethical principles for medical research involving human subjects. JAMA 2013;310:2191-4. [Crossref] [PubMed]
- Wang M, Li S, Zheng T, et al. Big Data Health Care Platform With Multisource Heterogeneous Data Integration and Massive High-Dimensional Data Governance for Large Hospitals: Design, Development, and Application. JMIR Med Inform 2022;10:e36481. [Crossref] [PubMed]
- Sarna T, Sengupta T, Miloro M, et al. Cervical necrotizing fasciitis with descending mediastinitis: literature review and case report. J Oral Maxillofac Surg 2012;70:1342-50. [Crossref] [PubMed]
- Prado-Calleros HM, Jiménez-Fuentes E, Jiménez-Escobar I. Descending necrotizing mediastinitis: Systematic review on its treatment in the last 6 years, 75 years after its description. Head Neck 2016;38:E2275-83. [Crossref] [PubMed]
- Reuter TC, Korell V, Pfeiffer J, et al. Descending necrotizing mediastinitis: etiopathogenesis, diagnosis, treatment and long-term consequences-a retrospective follow-up study. Eur Arch Otorhinolaryngol 2023;280:1983-90. [Crossref] [PubMed]
- Scaglione M, Pezzullo MG, Pinto A, et al. Usefulness of multidetector row computed tomography in the assessment of the pathways of spreading of neck infections to the mediastinum. Semin Ultrasound CT MR 2009;30:221-30. [Crossref] [PubMed]
- Sun Q, Li Z, Wang P, et al. Unveiling the Pathogenic Bacteria Causing Descending Necrotizing Mediastinitis. Front Cell Infect Microbiol 2022;12:873161. [Crossref] [PubMed]
- Casanova J, Bastos P, Barreiros F, et al. Descending necrotising mediastinitis--successful treatment using a radical approach. Eur J Cardiothorac Surg 1997;12:494-6. [Crossref] [PubMed]
- Ris HB, Banic A, Furrer M, et al. Descending necrotizing mediastinitis: surgical treatment via clamshell approach. Ann Thorac Surg 1996;62:1650-4. [Crossref] [PubMed]
- De Palma A, Cantatore MG, Di Gennaro F, et al. Multidisciplinary Approach in the Treatment of Descending Necrotizing Mediastinitis: Twenty-Year Single-Center Experience. Antibiotics (Basel) 2022;11:664. [Crossref] [PubMed]
- Kocher GJ, Hoksch B, Caversaccio M, et al. Diffuse descending necrotizing mediastinitis: surgical therapy and outcome in a single-centre series. Eur J Cardiothorac Surg 2012;42:e66-72. [Crossref] [PubMed]
- Sandner A, Börgermann J. Update on necrotizing mediastinitis: causes, approaches to management, and outcomes. Curr Infect Dis Rep 2011;13:278-86. [Crossref] [PubMed]
- Roberts JR, Smythe WR, Weber RW, et al. Thoracoscopic management of descending necrotizing mediastinitis. Chest 1997;112:850-4. [Crossref] [PubMed]
- Yanık F, Karamustafaoğlu YA, Yoruk Y. Management of a difficult infectional disease: Descending necrotizing mediastinitis. J Infect Dev Ctries 2018;12:748-54. [Crossref] [PubMed]
- Son HS, Cho JH, Park SM, et al. Management of descending necrotizing mediastinitis using minimally invasive video-assisted thoracoscopic surgery. Surg Laparosc Endosc Percutan Tech 2006;16:379-82. [Crossref] [PubMed]
- Yim AP, Liu HP. Complications and failures of video-assisted thoracic surgery: experience from two centers in Asia. Ann Thorac Surg 1996;61:538-41. [Crossref] [PubMed]
- Walker WS, Pugh GC, Craig SR, et al. Continued experience with thoracoscopic major pulmonary resection. Int Surg 1996;81:255-8.
- Giudicelli R, Thomas P, Lonjon T, et al. Video-assisted minithoracotomy versus muscle-sparing thoracotomy for performing lobectomy. Ann Thorac Surg 1994;58:712-7; discussion 717-8. [Crossref] [PubMed]
- Nakata M, Saeki H, Yokoyama N, et al. Pulmonary function after lobectomy: video-assisted thoracic surgery versus thoracotomy. Ann Thorac Surg 2000;70:938-41. [Crossref] [PubMed]
- Congedo MT, Nachira D, Pennisi MA, et al. Risk Factors Associated with Post-Operative Complications in Multidisciplinary Treatment of Descending Necrotizing Mediastinitis. J Clin Med 2022;11:6364. [Crossref] [PubMed]



