
Etiology, diagnostic modalities, and short-term outcomes of hemoptysis—a retrospective cross-sectional study from a tertiary care center in Qatar
Highlight box
Key findings
• Respiratory tract infections continue to dominate the etiology of hemoptysis in our center at Qatar.
What is known and what is new?
• Known: Management of the patients with hemoptysis are mainly conservative in majority of the patients, and interventional procedures are required only in patients with severe hemoptysis.
• New: Lung cancers although a leading cause of hemoptysis for hemoptysis in the developed world, is not a major etiology in our study. This is likely attributed to the young age and diversity of the population in Qatar.
What is the implication, and what should change now?
• Clinical pathway guidelines must be tailored according to the etiology of hemoptysis that is influenced by the age and diversity of the population.
Introduction
Background
Hemoptysis is a symptom that has long captured the attention of physicians and researchers due to its potential implications for diagnosing and managing respiratory diseases. It refers to the expectoration of blood originating from the respiratory tract, which can range from mild streaks to life-threatening episodes. Hemoptysis may arise from various etiologies, including infectious, neoplastic, inflammatory, and vascular conditions, making its evaluation and management complex (1).
Rationale and knowledge gap
Identifying the underlying cause of hemoptysis is crucial for appropriate management and prognosis, as different etiologies require specific treatment approaches (2). The incidence of these various etiologies varies according to the geographic location and the population mix of the region (3,4). Qatar’s population is diverse and dynamic and comprises mainly of expatriate workers, mostly originating from South Asia (5). Data on the etiology and outcome of hemoptysis previously published from Qatar comprised of data from 1997–2007 when the population of Qatar was approximately 1.2 million (6). Since then, the population of Qatar has rapidly grown with an increasing diversity.
Objective
We conducted a comprehensive evaluation of the etiology, diagnostic modalities employed and short-term outcomes in patients with hemoptysis admitted to the major tertiary care hospital at Qatar, Hamad General Hospital (HGH). We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-939/rc).
Methods
Retrospective data collection from HGH Qatar over 3 years from 2015–2018 was conducted whereby the population of Qatar was approximately 2.76 million (5). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board (IRB) of Hamad Medical Corporation (HMC) under protocol number MRC-01-18-105, and individual consent for this retrospective analysis was waived. The electronic health records at HGH were reviewed for a diagnosis of hemoptysis in patients with an age >14 years, the age beyond which patients are managed by internal medicine physicians at HGH. The generated medical records were then reviewed retrospectively to complete the data collection sheet. The comprehensive data sheet comprised of demographic variables, quantification of hemoptysis, documented etiology, diagnostic modalities, and short-term treatment outcomes to discharge from the hospital.
Study definitions
In this study, hemoptysis was divided into mild (<30 mL/24 hour), moderate (≥30 and <100 mL/24 hour), and severe or massive (≥100 mL/24 hour) according to Fidan et al. (3).
Statistical analysis
To summarize the quantitative data, we calculated the mean and standard deviation (SD) for interval variables, and for categorical variables, we presented frequencies and percentages. Data normality was checked using the Kolmogorov-Smirnov test. For comparisons between two groups, we utilized independent t-tests or Mann-Whitney tests as appropriate for interval variables. For categorical variables, we employed Chi-square tests (or Fisher’s exact tests when necessary). A significant level of 0.05 (two-tailed) was considered statistically significant. We performed the analysis using SPSS version 29.0 statistical software package.
Results
Search of electronic health records resulted in 172 patient records. Majority were men 128 (74.4%), and the mean age was 37.9 years. South Asians were the majority ethnic group followed by Qatari nationals and non-Qatari Arabs as detailed in Table 1. The majority of the patients, 128 (74.4%) were non-smokers. Hypertension and diabetes were the most commonly associated comorbidities in 12.2% and 9.9% respectively (Table 1). Antiplatelet and anticoagulant use was noted in only 9.9% patients. Presenting symptoms were cough in 77.3% followed by fever in 27.3%. With regards to severity of hemoptysis, 154 (89.5%) patients presented with mild hemoptysis, 12 (7%) with moderate hemoptysis and 6 (3.5%) had severe hemoptysis. Mean duration of hemoptysis was 1.72±0.72 days (Table 2).
Table 1
| Baseline characteristics | Value, N=172 |
|---|---|
| Gender, n (%) | |
| Male | 128 (74.4) |
| Female | 44 (25.6) |
| Ethnicity, n (%) | |
| South Asian | 75 (43.6) |
| Other Asian | 20 (11.6) |
| Qatari | 35 (20.3) |
| Non-Qatari Arab | 24 (14.0) |
| African | 13 (7.6) |
| European | 5 (2.9) |
| Age, years | |
| Mean ± standard deviation | 37.9±16.4 |
| <25, n (%) | 33 (19.2) |
| 25–50, n (%) | 101 (58.7) |
| 51–75, n (%) | 31 (18.0) |
| Occupation, n (%) | |
| Unskilled/semiskilled worker | 66 (38.8) |
| Professionals | 13 (7.6) |
| Others | 93 (54.1) |
| Smoking status, n (%) | |
| Active smoker | 36 (20.9) |
| Ex-smoker | 8 (4.7) |
| Non-smoker | 128 (74.4) |
| Comorbidities, n (%) | |
| Diabetes mellitus | 17 (9.9) |
| Hypertension | 21 (12.2) |
| History of tuberculosis | 11 (6.4) |
| Coronary artery disease | 10 (5.8) |
| Bronchiectasis | 8 (4.7) |
| Chronic kidney disease | 6 (3.5) |
| Chronic obstructive pulmonary disease/asthma | 5 (2.9) |
| History of lung cancer | 3 (1.7) |
| Antiplatelet or anticoagulants, n (%) | |
| Aspirin | 11 (6.4) |
| Aspirin and clopidogrel | 2 (1.2) |
| Warfarin | 3 (1.7) |
| Rivaroxaban | 1 (0.6) |
Table 2
| Characteristics | Value |
|---|---|
| Severity of hemoptysis, n (%) | |
| Mild (<30 mL) | 154 (89.5) |
| Moderate (30–100 mL) | 12 (7.0) |
| Severe (>100 mL) | 6 (3.5) |
| Duration of hemoptysis | |
| Mean ± standard deviation, days | 1.72±0.72 |
| <3 days, n (%) | 73 (42.4) |
| 3 days–2 weeks, n (%) | 72 (41.9) |
| >2 weeks, n (%) | 27 (15.7) |
| Presenting symptoms, n (%) | |
| Cough | 133 (77.3) |
| Fever | 47 (27.3) |
| Bronchoscopy findings (N=30), n (%) | |
| Active bleeding | 6 (20.0) |
| Blood clot | 4 (13.3) |
| Endobronchial lesion (infiltrative) | 5 (16.7) |
| Erythema/inflammation | 4 (13.3) |
| Treatment, n (%) | |
| Observation | 77 (44.8) |
| Antibiotics | 53 (30.8) |
| Anti-tuberculous medications | 10 (5.8) |
| Bronchial artery embolization | 2 (1.2) |
| Endobronchial instillation of adrenaline | 1 (0.5) |
Respiratory infection was the most common cause in 125 (72.6%) patients. Other identified causes are depicted in Figure 1. Respiratory infection subgroups included acute lower respiratory infection in 80 (46.5%) patients followed by pneumonia in 35 (20.3%) and infective exacerbation of asthma or chronic obstructive pulmonary disease in 10 (5.8%). The microbiological results are detailed in Table 3.
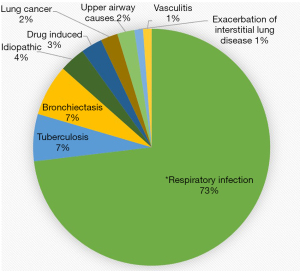
Table 3
| Respiratory sample | Number of patients, n (%) |
|---|---|
| Sputum gram stain and culture (N=39*) | |
| Bacteria | 5 (12.8) |
| Hemophilus influenzae | 3 (7.7) |
| Klebsiella pneumonia | 1 (2.6) |
| Staphylococcus aureus | 1 (2.6) |
| Fungus | |
| Candida albicans | 2 (5.1) |
| Sputum acid fast bacilli stain and culture (N=79) | |
| Mycobacterium tuberculosis | 5 (6.3) |
| Nontuberculous mycobacterium | 2 (2.5) |
| Bronchoalveolar lavage (N=30) | |
| Positive results | 18 (60.0) |
| Bacteria | 10 (33.3) |
| Hemophilus influenzae | 3 (10.0) |
| Pseudomonas aeruginosa | 3 (10.0) |
| Enterobacter | 1 (3.3) |
| Staphylococcus aureus | 1 (3.3) |
| Klebsiella pneumonia | 2 (6.7) |
| Fungus | 3 (10.0) |
| Aspergillus niger | 1 (3.3) |
| Aspergillus terreus | 1 (3.3) |
| Candida species | 1 (3.3) |
| Acid fast bacilli stain and culture | |
| Mycobacterium tuberculosis | 3 (10.0) |
| Nontuberculous mycobacterium | 2 (6.7) |
*, multiple isolates from single specimen culture.
Review of investigations noted that tuberculin skin test was done in 13 patients and only 7 (4.1%) had a positive result and Interferon Gamma Release Assay (QuantiFERON, Qiagen, Hilden, Germany) done in 32 patients reported positive result in 10 (5.8%). Chest radiographs were done in 153 cases with the majority (43.8%) showing no discernable abnormalities. Among the abnormal chest radiographs, consolidation was noted in 30 (19.6%) and fibrotic changes in 7 (4.6%) patients (Table 4). The decision to proceed with a chest computed tomography (CT) scan was based on the attending physician’s clinical impression. CT chest was done in patients with abnormal chest X-ray (CXR) and high-risk features like moderate to severe hemoptysis, history of recurring episodes of hemoptysis, duration of hemoptysis more than 2 weeks, history of smoking and personal history of malignancy. Patients who had a normal CXR were noted to have abnormal findings in CT chest, that comprised of nodular infiltrates in lung parenchyma, ground glass changes, localized fibrotic changes, small cavitary lesions and non-significant lymphadenopathy as denoted in Table 4. The most common reported finding was consolidation in 56.6% followed by nodules or mass in 23.7% and a representative CT image is shown in Figure 2.
Table 4
| Radiological findings | Chest radiograph, N=153, n (%) | CT chest, N=76, n (%) |
|---|---|---|
| Normal | 67 (43.8) | 14 (18.4) |
| Infiltrates/consolidation | 30 (19.6) | 43 (56.6) |
| Mass/nodule | 4 (2.6) | 18 (23.7) |
| Ground glass changes | Not applicable | 15 (19.7) |
| Bronchiectasis | 2 (1.3) | 12 (15.8) |
| Pleural effusion | 6 (3.9) | 8 (10.5) |
| Pleural thickening | Not applicable | 2 (2.6) |
| Fibrotic changes | 7 (4.6) | 7 (9.2) |
| Bronchial thickening | Not applicable | 6 (7.9) |
| Emphysema | Not applicable | 6 (7.9) |
| Mediastinal lymphadenopathy | Not applicable | 5 (6.6) |
| Collapse | Not applicable | 1 (1.3) |
| Cavity | Not applicable | 1 (1.3) |
CT, computed tomography.

Bronchoscopy was conducted in 30 patients and reported normal findings in 11 and hence a diagnostic yield for localization at 63.3% as reported in Table 2. All patients with severe hemoptysis who underwent bronchoscopy had localization of the source of bleeding. Bronchoscopy was considered in all patients with moderate and severe hemoptysis and in those patients with history of recurring episodes of hemoptysis and duration of hemoptysis more than 2 weeks with history of smoking and abnormal CXR and or CT chest findings. During bronchoscopy, active bleeding was reported in 6 patients, along with clots in 4 patients, erythema and inflammation in 5 patients and endobronchial lesion (infiltrative lesions) in 5 patients as shown in Figure 3. All 5 patients who had endobronchial lesions were offered biopsy for histopathology. One patient refused biopsy and in the 4 patients who underwent biopsy, 2 patients had lung cancer, 1 had chronic non-specific inflammation and inconclusive findings in the last.

Treatment options were conservative with only observation in 44.8% patients followed by treatment with antibiotics in 30.8% and anti-tuberculous medication in 5.8%. Of the 6 patients with severe/massive hemoptysis, 2 required BAE; 1 was treated with endobronchial administration of adrenaline.
In the patients who had BAE, one had left hilar mass with inconclusive pathology and recurring massive hemoptysis despite administration of adrenaline via bronchoscopy. The second patient had multiple cavitary lesions from active pulmonary tuberculosis (TB) and persistent hemoptysis during hospital stay.
The differences between moderate and massive hemoptysis on baseline characteristics, CT chest and causes of hemoptysis are described in Table 5. There were no reports of hemoptysis or death at hospital discharge.
Table 5
| Characteristic | Severe hemoptysis (N=6) | Moderate hemoptysis (N=12) | P value |
|---|---|---|---|
| Gender, n (%) | |||
| Male | 6 (100.0) | 7 (58.3) | 0.11 |
| Female | 0 | 5 (41.7) | |
| Age, mean ± standard deviation, years | 46.3±12.0 | 42.3±18.6 | 0.64 |
| Smoking status, n (%) | |||
| Active smoker | 3 (50.0) | 3 (25.0) | 0.02 |
| Ex-smoker | 3 (50.0) | 1 (8.3) | |
| Non-smoker | 0 | 8 (66.7) | |
| Comorbidities | |||
| Diabetes mellitus | 2 (33.3) | 1 (8.3) | 0.25 |
| Hypertension | 2 (33.3) | 2 (16.7) | 0.57 |
| Bronchiectasis | 0 | 4 (33.3) | 0.24 |
| Chronic obstructive pulmonary disease/asthma | 1 (16.7) | 0 | 0.33 |
| CT chest findings, n (%) | |||
| Infiltrates/consolidation | 5 (83.3) | 8 (66.7) | 0.61 |
| Ground glass changes | 4 (66.7) | 3 (25.0) | 0.14 |
| Bronchiectasis | 2 (33.3) | 4 (33.3) | >0.99 |
| Mass | 1 (16.7) | 0 | 0.33 |
| Cavity | 1 (16.7) | 0 | 0.61 |
| Bronchoscopy findings, n (%) | |||
| Active bleeding | 4 (66.7) | 2 (16.7) | 0.10 |
| Blood clot | 2 (33.3) | 0 | 0.12 |
| Infiltrative endobronchial lesion | 4 (66.7) | 1 (8.3) | 0.02 |
| Erythema/inflammation | 3 (50.0) | 1 (8.3) | 0.11 |
| Microbiology, n (%) | |||
| Hemophilus influenzae | 0 | 2 (16.7) | 0.52 |
| Staphylococcus aureus | 1 (16.7) | 0 | 0.33 |
| Pseudomonas aeruginosa | 2 (33.3) | 0 | 0.12 |
| Causes of hemoptysis, n (%) | |||
| Lung cancer | 2 (33.3) | 0 | 0.12 |
| Bronchiectasis | 2 (33.3) | 4 (33.3) | >0.99 |
| Pneumonia | 1 (16.7) | 6 (50.0) | 0.32 |
| Tuberculosis | 1 (16.7) | 1 (8.3) | >0.99 |
| Acute lower respiratory tract infection | 0 | 1 (8.3) | >0.99 |
CT, computed tomography.
Discussion
In this retrospective data review, non-tuberculous infection with acute lower respiratory tract infection and pneumonia were the most common causes of hemoptysis in Qatar. Data from middle east has reported bronchiectasis and TB as the major causes of hemoptysis (7). Prior study from Qatar reports idiopathic causes in 23.5% patients followed by pneumonia (12.8%), and bronchiectasis (11.8%) with malignancy in only 7.8% patients (6). This is consistent with our study reporting infection as the leading cause. Data collection in our study was through review of electronic health record while paper-based records were reviewed in the previous study. Improved documentation and access to diagnostic tests can contribute to having more confirmed diagnosis in our cohort. It is interesting to note that over the period of a decade, the etiology continues to remain the same despite doubling of the population and the increase in the diversity from people of only five nationalities apart from nationals and Arabs to 77 other nationalities (8,9). However, 40% of the population over the period continues to be from the Indian subcontinent. The mean age of the previous cohort was 46.2 years, and our cohort are younger by almost 10 years reflecting the increasing influx of young working-class population into Qatar. Our findings are similar to the reported worldwide etiology where acute respiratory tract infections are the most common cause of hemoptysis accounting for around 60–70% of cases followed by bronchiectasis and malignancy (10,11). Lung cancers are a significant etiology for hemoptysis in the developed world (12). On the contrary, there is a small contribution of lung carcinomas to hemoptysis in our study. This finding is in tandem with the sparse literature from the middle east region where age, a predominantly young population is considered as a factor that dilutes the contribution of lung carcinomas in hemoptysis (6). In endemic regions and in developing countries like India however, TB continues to be the leading cause of hemoptysis (1,13). Despite most of the studied cohort being young adult men from working class of South Asian origin, the predominance of respiratory tract infections as compared to TB in causing hemoptysis may be explained by the rigorous health screening policies exercised by the Ministry of Interior, Qatar in ensuring that expatriates especially from TB endemic regions undergo medical fitness clearance and treatment at entry to Qatar (14).
Congruent with epidemiological statistics (15), our study observed an overwhelming majority of mild hemoptysis cases while massive or severe hemoptysis were rare. Mild hemoptysis is self-resolving but severe hemoptysis mandates immediate attention as bleeding may spread through the tracheobronchial tree leading to asphyxiation and death therefore identification of massive hemoptysis and its etiology is cardinal as untreated massive hemoptysis can be fatal in more than 50% (16,17). Appropriate imaging techniques can play a vital role in correctly diagnosing and managing this condition.
CXR is readily accessible, easily performed and therefore, preferred as an early diagnostic modality in patients presenting with hemoptysis (18,19). As in our cohort, CXR may reveal a focal or diffuse infiltration in the lung tissue and detect underlying lesions, masses and abnormalities in the parenchyma and pleura (17). However, CXR alone has a 55% positive diagnostic yield (20) and can be falsely normal in nearly one-fifth of bronchial malignancies (21). Therefore, CXR cannot be relied on their own and further investigation with CT scan and/or bronchoscopy is indicated. Although not a standard protocol, CT scan with contrast was performed prior to bronchoscopy in this study, reflecting a center-based practice to improve accuracy of patient assessment. Despite a sensitivity of 90% in identifying endobronchial lesions, CT chest is limited in its ability to distinguish between blood clots and tumor lesions, and it is therefore best to be complimented with a bronchoscopy for further clarification or, more information (22). In the study by Quigley et al. on 165 patients with moderate to severe hemoptysis, they recommend the strategy of CT chest and bronchoscopy to be complementary with no specific ranking order unless CT chest localizes the origin of severe hemoptysis in patients who are candidate for BAE (12). Although we have used the term severe hemoptysis according to Fidan et al., a more practical approach would be to replace both “severe” and “massive” hemoptysis with the term “life-threatening”. This terminology aligns with the proposed definition by Ibrahim, which describes life-threatening hemoptysis as that exceeding >100 mL in 24 hours or leading to abnormal gas exchange, airway obstruction, or hemodynamic instability. This adjustment underscores the urgency of diagnosing and managing such cases (3,23).
Strengths and limitations
While our study has been able to review useful data associated with hemoptysis, it is important to mention that the study has limitations inherent to a retrospective design. It is for the same reason that the amount of data was also missing. The small sample size also restricts us from advanced statistics looking into association with pertinent variables.
Explanations of findings
These are findings from a single center in the country. However, HGH is the only tertiary center with access to therapeutic bronchoscopy and interventional radiology service. Hence, these findings could indeed be generalized to the country as well as representative of the diversity of the region.
Implications and actions needed
We recommend that findings from this study and its few predecessors from the Gulf Cooperation Council (GCC) region should be used to guide future studies of prospective nature to extract more reliable results.
Conclusions
Respiratory infections continue to dominate the etiology of hemoptysis in Qatar. Conservative management with antibiotics and observation treated majority of the patients with no reported recurrence or death during the hospital stay. Massive hemoptysis is uncommon but will invariably need intervention for management in a third of the cases. We recommend that findings from this study and its few predecessors from the GCC region should be used to guide future studies of prospective nature to extract more reliable results.
Acknowledgments
We would like to acknowledge Dr. Omar Alsaed, Rheumatology consultant for his contribution to data analysis.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-939/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-939/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-939/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-939/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board (IRB) of Hamad Medical Corporation (HMC) under protocol number MRC-01-18-105, and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- O'Gurek D, Choi HYJ. Hemoptysis: Evaluation and Management. Am Fam Physician 2022;105:144-51.
- Mondoni M, Carlucci P, Job S, et al. Hemoptysis: diagnosis and management. ERJ Open Res 2018;51:1701813.
- Fidan A, Ozdoğan S, Oruç O, et al. Hemoptysis: a retrospective analysis of 108 cases. Respir Med 2002;96:677-80. [Crossref] [PubMed]
- Pires FS, Teixeira N, Coelho F, et al. Hemoptysis – etiology, evaluation and treatment in a university hospital. Rev Port Pneumol 2011;17:7-14. [Crossref] [PubMed]
- Available online: https://worldpopulationreview.com/countries/qatar-population
- Al-Nesf MA, Jerobin J, Al-Alawi AA, et al. Etiology and outcome of hemoptysis in Qatar, a high-resource country with a large expatriate population: A retrospective study. Qatar Med J 2019;2019:1. [Crossref] [PubMed]
- Abal AT, Nair PC, Cherian J. Haemoptysis: aetiology, evaluation and outcome--a prospective study in a third-world country. Respir Med 2001;95:548-52. [Crossref] [PubMed]
-
US Department of State - Population of Qatar by nationality - 2017 report. Available online: https://priyadsouza.com/population-of-qatar-by-nationality-in-2017
- Tsoumakidou M, Chrysofakis G, Tsiligianni I, et al. A prospective analysis of 184 hemoptysis cases: diagnostic impact of chest X-ray, computed tomography, bronchoscopy. Respiration 2006;73:808-14. [Crossref] [PubMed]
- Mondoni M, Carlucci P, Job S, et al. Observational, multicentre study on the epidemiology of haemoptysis. Eur Respir J 2018;51:1701813. [Crossref] [PubMed]
- Quigley N, Gagnon S, Fortin M. Aetiology, diagnosis and treatment of moderate-to-severe haemoptysis in a North American academic centre. ERJ Open Res 2020;6:00204-2020. [Crossref] [PubMed]
- Bhalla A, Pannu AK, Suri V. Etiology and outcome of moderate-to-massive hemoptysis: Experience from a tertiary care center of North India. Int J Mycobacteriol 2017;6:307-10. [Crossref] [PubMed]
- World Health Organization. Global Tuberculosis Control 2009. Epidemiology Strategy Financing [Internet]. 2009 [cited 2016 Dec 20]. Available online: http://reliefweb.int/sites/reliefweb.int/files/resources/878BDA5E2504C9F449257584001B5E60-who_mar2009.pdf
- Gershman E, Guthrie R, Swiatek K, et al. Management of hemoptysis in patients with lung cancer. Ann Transl Med 2019;7:358. [Crossref] [PubMed]
- Aidé MA. Hemoptysis. J Bras Pneumol 2010;36:278-80. [Crossref] [PubMed]
- Chun JY, Morgan R, Belli AM. Radiological management of hemoptysis: a comprehensive review of diagnostic imaging and bronchial arterial embolization. Cardiovasc Intervent Radiol 2010;33:240-50. [Crossref] [PubMed]
- Jeudy J, Khan AR, Mohammed TL, et al. ACR Appropriateness Criteria hemoptysis. J Thorac Imaging 2010;25:W67-9. [Crossref] [PubMed]
- Sirajuddin A, Mohammed TL A. 44-year-old man with hemoptysis: a review of pertinent imaging studies and radiographic interventions. Cleve Clin J Med 2008;75:601-7. [Crossref] [PubMed]
- Vanni S, Bianchi S, Bigiarini S, et al. Management of patients presenting with haemoptysis to a Tertiary Care Italian Emergency Department: the Florence Haemoptysis Score (FLHASc). Intern Emerg Med 2018;13:397-404. [Crossref] [PubMed]
- Bradley SH, Hatton NLF, Aslam R, et al. Estimating lung cancer risk from chest X-ray and symptoms: a prospective cohort study. Br J Gen Pract 2021;71:e280-6. [Crossref] [PubMed]
- Larici AR, Franchi P, Occhipinti M, et al. Diagnosis and management of hemoptysis. Diagn Interv Radiol 2014;20:299-309. [Crossref] [PubMed]
- Ibrahim WH. Massive haemoptysis: the definition should be revised. Eur Respir J 2008;32:1131-2. [Crossref] [PubMed]


