
A novel method for the bronchial occlusion of prolonged air leakage using customized endobronchial plugs
Highlight box
Key findings
• Bronchial occlusion with customized endobronchial plugs represents an effective and simple option for the management of prolonged air leakage (PAL) in patients who are not fit for surgery.
What is known and what is new?
• Endoscopic interventions have been used as options for the management of PAL in patients who are unfit for surgery.
• This study focuses on the safety and efficacy of using customized endobronchial plugs for bronchial occlusion of PAL treatment.
What is the implication, and what should change now?
• The new customized plug is a cost-effective alternative in the management of PAL, especially for developing countries.
Introduction
Refractory pneumothorax includes recurrent pneumothorax and prolonged air leakage (PAL). PAL is defined as persistent air leakage for more than seven days (1) and is indicated by abnormal communication between the pleural space and lung parenchyma or airways. PAL can be caused by alveolar-pleural fistulas (APFs) or bronchopleural fistulas (BPFs) and is associated with prolonged hospitalization and significant morbidity; thus, PAL represents a significant clinical challenge for both clinicians and patients (2,3).
Surgery is currently considered to be the recommended treatment for the management of PAL (4,5). However, surgical management is not without risk for patients in poor condition or with limited cardiopulmonary function; these patients are known as the suboptimal surgical candidates. Existing guidelines recommend medical pleurodesis as an alternative treatment in patients with PAL who are not suitable candidates for surgery (4,5). However, medical pleurodesis may not be suitable or effective for patients with extremely vigorous air leaks that prevent the visceral and parietal pleura from coming into contact. With the development of bronchoscopic techniques, endoscopic interventions have been increasingly used as options for the management of PAL in patients who are unfit for surgery (6). Bronchial occlusion can help control air leakage, involving biocompatibility sealants and closure devices. Silicone plugs have been confirmed to be highly effective for managing PAL as endobronchial blockers (7-9). A key step after identifying the suspect airway is the placement of silicone plugs. Several approaches have been reported to facilitate insertion of such plugs into the target bronchus (10-12). However, it is still difficult to insert the plugs into the angulated bronchi such as the apical segment of the right upper lobe. In addition, the commercially produced endobronchial Watanabe spigot (EWS) is not available in China. Therefore, we designed a conical silicone plug for the treatment of PAL. In this study, we evaluated the efficacy of bronchial occlusion when applying the customized silicone plugs for the management of PAL. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1053/rc).
Methods
Patients
This was a retrospective study conducted in the Second Affiliated Hospital of Fujian Medical University between August 2012 and December 2021. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of the Second Affiliated Hospital of Fujian Medical University (FYFE2021-51) and individual consent for this retrospective analysis was waived.
All the included participants had PAL and had been administered with intercostal drainage for more than seven days. These patients were unsuitable for surgical management due to their poor overall clinical condition. We excluded the patients with the following conditions: (I) patients were allergic to silicone material; (II) patients had uncontrolled acute lung infection or severe chronic infection at the target bronchi; (III) patients with compromised cardiopulmonary function unable to tolerate the bronchoscopic procedure. Bronchoscopic treatment for bronchial occlusion was performed on each patient using the customized silicone plugs. Written informed consent was obtained from all patients.
Customized silicone plugs
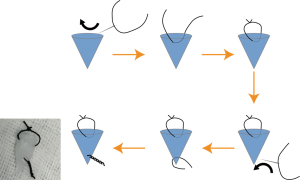
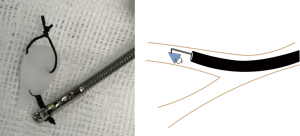
The silicone plugs were manufactured from a mandibular prosthesis (Kangning Medical Device, Shanghai, China). Plug size was designed to be slightly larger than the diameter of the target bronchus measured on high-resolution computerized tomography (HRCT). Then, we used scissors to trim the silicone material to a conical shape with rough surface to facilitate insertion into the airway. A knot (length =1 cm) was tied at the tip of the silicone plug using 1-0 suture thread to manipulate orientation. In addition, a thread loop was placed at the back end of the plug for convenient removal (Figure 1).
Bronchoscopic procedure and plug placement
All patients underwent flexible bronchoscopy under local anesthesia with 2% lidocaine and mild sedation with intravenous midazolam. The bronchi responsible for feeding the air leakage were identified by the balloon occlusion test or by end-tidal carbon dioxide (EtCO2) detection. Technical details have been described in our previous publication (1). In brief, for balloon occlusion detection, the target bronchi were defined as those exhibiting a reduction or disappearance of air leakage through the chest tube after being occluded by an inflated balloon. If the balloon occlusion test failed to determine the responsible bronchi, then multiple leaks were considered. The affected bronchi were then determined by EtCO2 detection. When the EtCO2 value of a specific bronchus was approximately 5 mmHg lower than that of the main bronchus on the side of the pneumothorax, then this would be defined as the responsible bronchus.
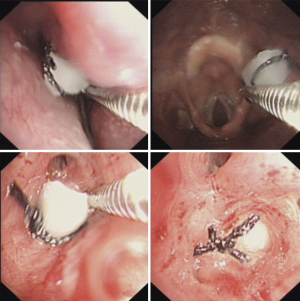
After identifying the responsible bronchus, a grasping forceps was passed through the working channel of a flexible bronchoscope to grasp the knot at the tip of the plug (Figure 2). Subsequently, guided by the bronchoscope, the grasping forceps held the plug to reach the target bronchus by adjusting the angle and direction. While maintaining the bronchoscope at the bronchial opening, the plug was inserted into the target bronchus with the assistance of the forceps. Once the plug blocked the target bronchus, the bronchoscope was used to press the back end of the plug further into the bronchus while simultaneously retracting the forceps. Finally, the forceps were reintroduced to impact against the back end of the plug to ensure a tight seal (Figure 3). In cases where local anesthesia was administered, patients were instructed to cough after the plug placement to ensure its stability and prevent potential migration. After the procedure, oral codeine was prescribed for the first 3 days to suppress coughing and prevent expectoration. For multiple leaks, we used multiple plugs, or a single large plug, to occlude the affected bronchi. The plugs were removed by grasping the loop at the back end when the physician deemed this to be clinically feasible.
Outcomes measurement
After the bronchoscopic procedure, all patients were continuously observed for 7 days. When the air leakage was not completely resolved after bronchial occlusion, we implemented additional treatment by performing chemical pleurodesis with interleukin-2 infusion. When no bubbling was detected in the water seal chest drain system for at least 3 days, the drainage tube was then clamped for a minimum of 1 day. After the lung recruitment was confirmed through chest X-ray or chest CT, the drainage tube was removed.
Statistical analysis
We used descriptive statistics, such as the mean, median, range, and percentage, to summarize patient demographics and outcomes. The data analysis was conducted using IBM® SPSS® Software version 22.0.
Results
A total of 23 male patients, with a median age of 62 years (range, 24–81 years), underwent bronchial occlusion using the customized silicone plugs (Table 1). The location of PAL was on the right in 15 cases and on the left in 8 cases. Each patient had at least one of the following underlying diseases: chronic obstructive disease (n=19), pneumoconiosis (n=6), old pulmonary tuberculosis (n=4), bronchiectasis (n=1) and bronchiolitis obliterans (n=1). Prior to bronchoscopic treatment, the median degree of collapsed lung was 20% (range, 10% to 85%), and the median duration of chest drainage was 28 days (range, 12–133 days).
Table 1
| Demographics | Values |
|---|---|
| Number of participations | 23 |
| Age (years) | 62 [24–81] |
| Sex (male/female) | 23/0 |
| Location of air leakage | |
| Right side | 15 |
| Left side | 8 |
| Duration of chest drainage (days) | 28 [12–133] |
| Degree of collapsed lung (%) | 20 [10–85] |
| Underlying diseases of pulmonary | |
| Chronic obstructive pulmonary disease | 19 |
| Pneumoconiosis | 6 |
| Old pulmonary tuberculosis | 4 |
| Bronchiectasis | 1 |
| Bronchiolitis obliterans | 1 |
Data are presented as n or median [range].
The outcomes of the plug procedures are listed in Table 2 and Table S1. Bronchial occlusion was performed 1 to 3 (median =1) times per patient. The median number of plugs inserted for bronchial occlusion was 2 (range, 1–3), and the mean diameter of the plugs used was 5.5 mm, with a range of 3 to 10 mm. Based on the localization of the responsible bronchi, the plugs were placed in the right upper (n=7), right middle (n=5), right lower (n=3), left upper (n=7), and left lower lobe (n=1). All plugs were successfully inserted into the target bronchi (success rate: 100%), although 60.9% (14/23) of the target bronchi were located in the upper lobe. Only one patient experienced expectoration of the plugs and required a repeat insertion.
Table 2
| Variables | Values |
|---|---|
| Number of plugs inserted per patient | 2 [1–3] |
| Position of plugs placement | |
| RUL | 7 |
| RML | 5 |
| RLL | 3 |
| LUL | 7 |
| LLL | 1 |
| Diameter of plugs used (mm) | 5.5 (3–10) |
| Number of bronchial occlusion procedure | 1 [1–3] |
| Successful removal of the drainage tube | 20 (87.0) |
| Status of air leaks after bronchial occlusion | |
| Cessation | 13 (56.5) |
| Reduction | 7 (30.4) |
| No change | 3 (13.0) |
| Duration of air leak stopped (days) | 5.9 (0–21) |
| Recurrence | 3 (13.0) |
Data are presented as median [range], n, mean (range) or n (%). RUL, right upper lobe; RML, right middle lobe; RLL, right lower lobe; LUL, left upper lobe; LLL, left lower lobe.
Following bronchial occlusion with the plugs, drainage tubes were successfully removed in 20 (87.0%) of the 23 patients. In our study, after using bronchial occlusion alone, 13 patients (56.5%) observed complete cessation of air leakage without the need for pleurodesis, while seven patients (30.4%) experienced a reduction in bubbles in the water-sealed chamber and required additional pleurodesis as a combined therapy to achieve complete resolution of pneumothorax. The mean duration of time over which the air leakage stopped was 5.9 days, including the immediate disappearance of air leakage after the insertion of the plugs in three cases.
The plugs were removed in nine out of the 23 patients who achieved complete resolution of air leakage; the median duration of placement was 63 days (range, 14–151 days). The other patients retained the plugs in their bronchi without any obvious discomfort over a 1-year period of follow-up. One patient experienced fever on day 3 following bronchial occlusion and was cured by antibiotic therapy without plug removal. Three patients experienced pneumothorax recurrence, and successfully managed air leakage through intercostal drainage. No severe treatment-related complications were observed during follow-up.
Discussion
Several occlusive devices can be used in the bronchoscopic treatment of PAL, including endobronchial valves (EBVs), Amplatzer devices, and spigots (6,13-15). Both EBVs and the Amplatzer device require special placement equipment and technical expertise. Furthermore, these two occlusive devices are expensive and not widely available in developing countries. The EWS is the most widely used endobronchial spigot and most often, yields successful outcomes when being applied for the bronchial occlusion in the treatment of PAL. However, the EWS spigot is not licensed in China. Therefore, we developed a silicone plug made from commercial chin implants that could also be replaced by other implants with the same quality of silicone. The biocompatibility and safety of this material have been verified previously by implant surgery over the long term. Our customized plugs have several key features that allow them to be placed successfully in the target bronchus as effective endobronchial occlusive devices. First, as the knot at the tip is tightly grasped with forceps, the spigot can be rotated in any direction without dropout during the placement procedure. Second, the plug can be easily removed as necessary by bronchoscopic grasping forceps with the knot created at the bottom of the plug. Third, the plug can be trimmed to a conical shape of any size so that it can be inserted into any distal airways. In addition, the cost of each plug is approximately 10 U.S. dollars, thus representing a highly affordable treatment option.
It is a significant challenge to insert an EWS spigot into the target bronchus via a bronchoscope, especially into the apical segment bronchus, by holding the graspable end of the EWS spigot with forceps (the conventional technique). The procedure used to insert the plug should be convenient and simple without the need of special devices. The technique used to place the customized plug described herein is a simple method that allows the plug to be inserted into the target bronchi at any angle without the aid of special instruments.
Unlike the previous methods used to maneuver the ends of the plugs, our new placement technique is characterized by grasping the knot at the tip of the plug for its insertion. This is more effective in terms of manipulating the direction at the tip of the plug. Using grasping forceps to adjust the orientation, the plug can be inserted into any bronchi in only a short period of time. We found that grasping the knot was more reliable than previously described techniques; furthermore, none of the plugs were dropped during the placement procedure. For patients who were unable to tolerate oral insertion of the bronchoscope, we successfully completed the placement procedure of the plug via transnasal bronchoscopy (Figure 3). In addition, the forceps that we used to grasp the knot were able to pass through the working channel (2.0 mm in diameter) of a thin bronchoscope, thus allowing simple insertion into the target bronchus. We also found that grasping the knot at the tip of the plug was associated with a shorter learning curve and a lower failure rate with regards to plug placement when compared with grasping the end of the plug (unpublished data). Junior bronchoscopists would also be easily able to master this technique after only simple training.
Previous studies reported that air leakage was stopped or reduced in 50% and 29.2% of patients, respectively, when EWS spigots were applied for the management of PAL (7). The success rate for drainage tube removal was from 72.7% to 86%, respectively, when using EWS alone or combined with pleural adhesions (7-9). In our study, the proportion of patients achieving complete cessation or a reduction in air leakage was 56.5% and 30.4%, respectively. Overall, 87.0% of patients achieved complete resolution of PAL when customized plugs were combined with pleurodesis. The efficacy of the customized plugs used in our case series was like that described in previous reports.
The complications associated with bronchial occlusion when using the EWS spigot included dyspnea (3.4%), pneumonia (3.4%) and fever (1.7%) (15). In our series of patients who were fitted with customized plugs as occlusive devices, there was only one case of fever with a short duration; there were no severe complications. The plugs were made of silicone material acquired from a mandibular prosthesis; this material has been confirmed to be safe for patients as a permanent implant. In the present study, the silicone plugs were placed in the airways of 14 patients for more than 1 year. None of these patients experienced any significant discomfort. Generally, the plug as a foreign body, should be removed from the bronchi after the resolution of air leakage. However, a previous study reported one patient in which the EWS spigot was retained in the airway without significant complications for more than 3 years (9). Based on the excellent biocompatibility and tolerance of this silicone material, we consider that it is acceptable to place our plugs over a long period of time with careful follow-up.
There are several limitations in our study that need to be considered. First, this was a retrospective study with a limited number of participants in a single center, and all patients were male. Multicenter and prospective clinical trials involving a larger sample size are required. Second, we did not record the operation time used to insert each plug. In future research, it would be worth to record operation time during the bronchoscopic process. Third, the proportion of cases with BPF among the enrolled patients was low; different causes of air leaks may affect the outcomes of treatment.
Conclusions
In conclusion, our study demonstrates that bronchial occlusion with customized endobronchial plugs represents an effective and simple option for the management of PAL in patients who are not good candidates for surgery. In countries where EWS is not available, especially in developing countries, our new customized plug represents a cost-effective alternative.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1053/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1053/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1053/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1053/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of the Second Affiliated Hospital of Fujian Medical University (FYFE2021-51) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zeng YM, Chen YF, Lin HH, et al. Use of endo-bronchial end-tidal CO(2) test for location of the pleural air leakage in patients with intractable pneumothorax. Ther Adv Respir Dis 2018;12:1753465818756564. [Crossref] [PubMed]
- Aprile V, Bacchin D, Calabrò F, et al. Intraoperative prevention and conservative management of postoperative prolonged air leak after lung resection: a systematic review. J Thorac Dis 2023;15:878-92. [Crossref] [PubMed]
- Albert RK. Pneumothorax: Challenging the Paradigm of Persistent Air Leak, but Where Is the Leak? Am J Respir Crit Care Med 2023;207:223. [Crossref] [PubMed]
- Gottlieb M, Long B. Managing Spontaneous Pneumothorax. Ann Emerg Med 2023;81:568-76. [Crossref] [PubMed]
- Barton EC, Maskell NA, Walker SP. Expert Review on Spontaneous Pneumothorax: Advances, Controversies, and New Directions. Semin Respir Crit Care Med 2023;44:426-36. [Crossref] [PubMed]
- Keshishyan S, Revelo AE, Epelbaum O. Bronchoscopic management of prolonged air leak. J Thorac Dis 2017;9:S1034-46. [Crossref] [PubMed]
- Sasada S, Tamura K, Chang YS, et al. Clinical evaluation of endoscopic bronchial occlusion with silicone spigots for the management of persistent pulmonary air leaks. Intern Med 2011;50:1169-73. [Crossref] [PubMed]
- Zhang HT, Xie YH, Gu X, et al. Management of Persistent Air Leaks Using Endobronchial Autologous Blood Patch and Spigot Occlusion: A Multicentre Randomized Controlled Trial in China. Respiration 2019;97:436-43. [Crossref] [PubMed]
- Kaneda H, Minami K, Nakano T, et al. Efficacy and long-term clinical outcome of bronchial occlusion with endobronchial Watanabe spigots for persistent air leaks. Respir Investig 2015;53:30-6. [Crossref] [PubMed]
- Mizumori Y, Nakahara Y, Hirata N, et al. Toward Easy and Rapid Bronchial Occlusion With an Endobronchial Watanabe Spigot: A New Technique Using a Guide Sheath and Curette. J Bronchology Interv Pulmonol 2020;27:122-7. [Crossref] [PubMed]
- Morikawa S, Okamura T, Minezawa T, et al. A simple method of bronchial occlusion with silicone spigots (Endobronchial Watanabe Spigot; EWS®) using a curette. Ther Adv Respir Dis 2016;10:518-24. [Crossref] [PubMed]
- Kida H, Muraoka H, Inoue T, et al. A Novel Technique for the Placement of Endobronchial Watanabe Spigots Into the Bronchus: Side-Grasping Method. J Bronchology Interv Pulmonol 2016;23:71-5. [Crossref] [PubMed]
- Welling JBA, Koster TD, Slebos DJ. From plugging air leaks to reducing lung volume: a review of the many uses of endobronchial valves. Expert Rev Med Devices 2023;20:721-7. [Crossref] [PubMed]
- Zhang J, Hu H, Xu L, et al. Innovative method for Amplatzer device implantation in patients with bronchopleural fistulas. BMC Pulm Med 2021;21:137. [Crossref] [PubMed]
- Watanabe Y, Matsuo K, Tamaoki A, et al. Bronchial Occlusion With Endobronchial Watanabe Spigot. Journal of Bronchology 2003;10:264-7.


