
A novel localization device for small pulmonary nodules in thoracoscopic wedge resection with adequate margin distance: a retrospective study
Highlight box
Key findings
• Preoperative computed tomography (CT)-guided 4-hook needle with scaled suture localization is a safe, efficient, and precise strategy for wedge resection of small pulmonary nodules (SPNs) via video-assisted thoracoscopic surgery with sufficient resection margin distance.
What is known and what is new?
• The commonly used localization methods are unable to determine the depth of SPNs or to obtain precise sufficient surgical margin distance.
• This study analyzed the efficacy of a 4-hook needle with a scaled suture to assist in determining the depth of SPNs and sufficient resection margin distance during thoracoscopic wedge resection.
What is the implication, and what should change now?
• The CT-guided 4-hook needle with scaled suture localization method has advantages in obtaining sufficient surgical margin distance.
• This method is applicable not only to superficial SPNs but also to deep SPNs.
Introduction
With the widespread use of low-dose chest computed tomography (CT) for lung cancer screening and regular physical examinations, the detection rate of small pulmonary nodules (SPNs) has increased significantly in China. Although the diagnostic accuracy of CT has recently been significantly improved (1), histopathological diagnosis is still the gold standard for SPNs that are suspected to be malignant. According to the 2021 Chinese guidelines for the screening and early detection of lung cancer (2) and the National Comprehensive Cancer Network guidelines for lung cancer screening (version 1.2020) (3), needle biopsy or surgical excision is recommended for SPNs when they show malignant characteristics. However, it is still difficult to obtain accurate histopathological diagnosis for SPNs with percutaneous or transtracheal biopsy (4,5). Rather, surgical resection is preferred in such cases to provide a definite diagnosis and complete removal of the SPN.
With the advantages of minimally invasion and fast recovery, video-assisted thoracoscopic surgery (VATS) has been widely used in the treatment of thoracic diseases, including SPNs. However, part of the SPNs may not be detectable during the surgery due to their soft texture, small size, or deep localization. A few localization methods have been applied to counter this problem, including percutaneous or transtracheal localization (4,6,7). CT-guided percutaneous localization with microcoils or other markers is a common and efficient method. However, this cannot determine the depth of SPNs during the surgery, leading to insufficient surgical margin distance or even occasional positive margins during wedge resection (8) that may require extended excision or lobectomy, which are less than optimal procedures.
Recently, the use of a novel SPN localization device, the 4-hook needle with scaled suture, has been reported in clinical settings with good success, safety, feasibility, and tolerability (9). One study found that with the anchor claw and scale system, this device can reduce the occurrence of displacement or dislodgement and facilitate effective and precise placement (9). However, this preliminary study did not elucidate the best indications, localization skills needed for this device, or the means to obtaining a safe resection margin distance during surgery, among other parameters. Given the design of the hook and scale system, we speculated that it could help obtain sufficient surgical margin distance, preventing residual tumor or extended excision. Therefore, in this study, we used this novel device for SPN localization with the aim of obtaining sufficient resection margin distance for “precise wedge resection” by modifying the anchor point and surgical procedures. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-871/rc).
Methods
Patients and inclusion criteria
In the present study, we performed a retrospective analysis on patients with SPNs undergoing CT-guided 4-hook needle localization and VATS via the electronic medical record system at The Third Affiliated Hospital of Sun Yat-Sen University. From November 1, 2021, to August 31, 2022, data on 58 patients recently diagnosed with 1 or more SPNs via CT were collected in total. All SPNs for localization and resection were highly suspicious for malignancy or their malignancy could not be ruled out according to a discussion by a multidisciplinary team of thoracic surgeons and radiologists. The selected criteria for wedge resection in this study included the following: (I) peripheral SPNs (major lesion with a maximum transverse diameter ≥8 mm but ≤20 mm) that were ≤3 cm from the visceral pleura, (II) CT indicated isolated lung metastasis when the primary tumor was well controlled, (III) patients desired surgical treatment, and (IV) patients had no contraindications to preoperative localization and surgery. Secondary ipsilateral nodules <8 mm in size suspected to be malignant were synchronously localized and resected. The time between diagnosis and localization was less than 4 weeks. A flow diagram of included and excluded patients is provided in the Figure 1. Written informed consent was obtained from patients and/or immediate family members. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the ethics committee of The Third Affiliated Hospital of Sun Yat-sen University (No. 02-246-01).
Interventional equipment and localization techniques
A 64-slice helical CT scanner (AquilionTSX-101A, Toshiba, Tokyo, Japan) was used to guide percutaneous puncture. The locating device was a 4-hook needle with a scaled suture (Sheng Jie Kang Biological Technology Co., Ltd., Ningbo, China). The components of this new device include a 4-hook anchor and a tricolored suture with a scale. The scale of the tricolored suture indicates different depths in the localization and operation procedure. The length of each colored suture is 3 cm, and it is divided into 6 sections on average that are white color, with 5 mm for each section (Figure 2). The 4-claw shape facilitates fixing in lung tissue to reliably estimate the depth of the nodule.
The puncture route and posture of the patient were determined by the location of nodule in the lung. The puncture route was the shortest and perpendicular to the pleura as possible and adjusted according to the planned VATS approach (Figure 3A). The detailed steps of the localization procedure have been described previously (9,10), with the difference in our study being that the 4-hook was localized behind or beside the nodule within 10 mm (Figure 3B), rather than through or in front of the nodule, in order to determine the depth of resection. The intended 4-hook anchor site was within 10 mm of the pulmonary nodule. After localization, the patient was subjected to a final CT scan to confirm the site of locating device and any complications. Patients typically underwent the operation within 24 hours after the localization procedure.

Surgical procedure
Most the patients were placed under general anesthesia via a laryngeal mask. If the patient was considered to have pleural adhesions in preoperative evaluation, a double-lumen endotracheal tube was used. According to the site of nodule and estimated difficulty of operation, the single- or 2-port VATS was used. In the fourth or fifth intercostal space, an incision of about 3 cm was made near the anterior axillary line. Under the 2-port method, another incision about 1 cm was made in the seventh intercostal space ipsilaterally at the midaxillary line to insert the thoracoscope.
The scaled suture was exposed outside the visceral pleura and found easily during surgery. The suture was pulled gently to read the scale (Figure 4A), and then an oval or curved forceps was used to tightly grasp the suture and the adjacent visceral pleura (Figure 4B). According to the reading on the scale to estimate the depth of nodule, and an oval forceps (diameter 10 mm) or a scale was used to measure the excision distance (Figure 4B). The predicted cutting edge was marked with an electrotome, and then wedge resection was performed with staplers. Predicted cutting distance was defined as the reading on the scale plus maximum transverse diameter of the nodule.
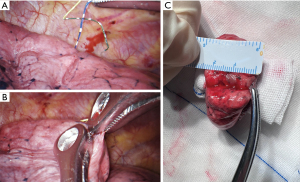
Frozen pathologic examination was performed during the operation. Regardless of the pathological result, the surgery was stopped if the margin distance was more than 5 mm. If adequate margin distance could not be guaranteed, expanded wedge resection or segmentectomy was performed. While the specimen was intact and collapsed, the nodule was palpated through the pleural surface, and then the nodule was transected through the maximum diameter, perpendicular to staple. The resection margin distance, including the staple line, was measured macroscopically with a ruler from the edge of the tumor to the nearest resection line (Figure 4C) and recorded by the surgeon in the operation note.
Histopathological evaluations
Clinical specimens were examined by pathologists. The margin distance was defined as the shortest width between the resection line and the tumor and was measured macroscopically. Tumor size was also measured. The staples were carefully cut away, and the margin tissue was examined histologically. If lung adenocarcinoma was diagnosed, the subtype and the percentage were recorded. According to the 2015 World Health Organization (WHO) Classification of Lung Tumors, minimally invasive adenocarcinoma (MIA) and adenocarcinoma in situ (AIS) were defined as small (≤3 cm) solitary adenocarcinomas that exhibited a lepidic growth pattern with ≤5 mm invasion (MIA) or without invasion (AIS) respectively. Invasive adenocarcinoma was described according to the following subtypes: lepidic, acinar, papillary, micropapillary, solid adenocarcinoma, and other. These data were recorded in the final pathological reports.
Main observation indicators
Data on the depth of the nodule, maximum diameter of the nodule, depth of localization device, and the distance from the claw to the edge of nodule were collected in the picture archiving and communication system. The depth of the nodule was defined as the distance from the pleura to the medial border of the nodule. The duration of localization, success rate, localization-related complications, effect of localization, operation time and margin distance, and margin to tumor ratio [margin distance (mm)/maximum tumor diameter (mm)] were recorded. All the indicators were determined by two surgeons and recorded after they reached a consensus.
Statistical analysis
The quantitative data are expressed as a number, median, and range, while categorical variables are described as a number and percentage. A chi-squared test or Fisher exact test was used for categorical variables, while a 2-sided Student t-test was used to compare continuous variables between the groups. A P value <0.05 was considered statistically significant. All statistical analyses were performed using SPSS 20 software (IBM Corp., Armonk, NY, USA).
Results
Baseline statistics
In this study, 58 patients (23 males and 35 females; median age 48 years; age range, 25–80 years) with 68 SPNs were collected according to the above mentioned inclusion and exclusion criteria (Figure 1). Most of the patients (48/58, 82.8%) had a single pulmonary nodule localization, and 10 patients (10/58, 17.2%) with two nodules underwent a simultaneous localization procedure. The clinical and pathologic characteristics are shown in Table 1. The nodules were classified into ground-glass opacity (64, 94.1%) and solid nodules (4, 5.9%). The median size and depth of nodules were 10.0 mm (range, 4–23 mm) and 18.9 mm (range, 4–52 mm), respectively, according to the CT image. The detail of pathological results and stage of nodules are summarized in Table 1.
Table 1
| Variables | Data (N1=58, N2=68) |
|---|---|
| Gender | |
| Male | 23 (39.7) |
| Female | 35 (60.3) |
| Age (years) | 48 [25–80] |
| Smoking history | |
| Yes | 16 (27.6) |
| No | 42 (72.4) |
| Size (diameter mm) | 10.0 [4–23] |
| Nodule type | |
| GGO | 64 (94.1) |
| Solid | 4 (5.9) |
| Location | |
| Right upper lobe | 37 (54.4) |
| Right middle lobe | 0 (0.0) |
| Right lower lobe | 9 (12.3) |
| Left upper lobe | 14 (20.6) |
| Left lower lobe | 8 (11.8) |
| Nodule depth* (mm) | 18.9 [4–52] |
| Depth ≤10 | 10 (14.7) |
| 10< depth ≤20 | 31 (45.6) |
| 20< depth ≤30 | 22 (32.4) |
| Depth >30 | 5 (7.4) |
| Pathological diagnosis | |
| Atypical adenomatous hyperplasia | 1 (1.5) |
| Adenocarcinoma in situ | 11 (16.2) |
| Minimally invasive adenocarcinoma | 45 (66.2) |
| Invasive adenocarcinoma | 4 (5.9) |
| Metastatic tumor | 3 (4.4) |
| Others** | 4 (7.4) |
| Stage*** | |
| Benign | 5 (5.9) |
| 0 | 11 (16.2) |
| IA1 | 49 (72.1) |
| IV (metastatic tumor) | 3 (4.4) |
Data are presented as median [range] or n (%). N1, number of patients. N2, number of small pulmonary nodules. *, nodule depth was defined as the distance from the pleura to the medial border of the nodule. **, including inflammation, granuloma, lymph node, and Langerhans histiocytosis. ***, stage was determined by the eighth edition classification of lung cancer. GGO, ground-glass opacity.
Localization procedure and surgery outcomes
Modified CT-guided 4-hook needle implantation was successfully achieved for 65 (95.6%) nodules in this study and failed in 3 cases (Table 2). The median time of the localization and surgical procedure were 24.9 min (range, 12–45 min) and 81.1 min (range, 35–240 min) respectively, and the median time interval between surgery and localization was 23.4 hours (range, 0.5–32 hours). The localization procedure was performed the day before surgery except in 1 patient for whom it was performed within 0.5 hours. The mean time of hospitalization was 5.1 days (range, 2–13 days), and no deaths occurred.
Table 2
| Variable | Data (N1=58, N2=68) |
|---|---|
| Time of localization procedure (min) | 24.9 [12–45] |
| Time of operation (min) | 81.1 [35–240] |
| Time between placement and surgery (hours) | 23.4 [0.5–32] |
| The time of hospitalization (days) | 5.1 [2–13] |
| The depth of the anchor claw (mm) | 19.5 [6–45] |
| Location of the anchor claw | |
| In nodules | 4 (5.9) |
| Around nodules (mm) | 61 (89.7) |
| 1< distance ≤5 | 48 (70.6) |
| 5< distance ≤10 | 7 (10.3) |
| 10< distance ≤15 | 5 (7.4) |
| Distance >15 | 1 (1.5) |
| Displacement | 3 (4.4) |
| Distance between claw and lesion (mm) | 4.2 [0–20] |
| Successful localization | 65 (95.6) |
| Unsuccessful localization | 3 (4.4) |
| Complications | 18 (26.6) |
| Parenchymal hemorrhage | 11 |
| Asymptomatic | 8 (11.8) |
| Symptomatic | 3 (4.4) |
| Pneumothorax | 7 |
| Asymptomatic | 6 (8.8) |
| Symptomatic | 1 (1.5) |
| Others | 0 (0.0) |
| Resection | |
| Wedge resection | 66 (97.1) |
| Segmentectomy | 1 (1.5) |
| Lobectomy | 1 (1.5) |
| Margin distance (mm) | 14.0 [8–26] |
| 8≤ distance <10 | 16 (23.5) |
| 10≤ distance <15 | 32 (47.1) |
| Distance ≥15 | 20 (29.4) |
| Margin distance/tumor size | |
| ≥1 | 62 (91.2) |
| <1 | 6 (8.8) |
Data are presented as median [range] or n (%). N1, the number of patients; N2, the number of small pulmonary nodules.
The median depth of the anchor claw was 19.5 mm (range, 6–45 mm), and the median distance from claw to the edge of the nodule was 4.2 mm (range, 0–20 mm). The distance between the claw and the nodule in most cases (59, 86.8%) was less than 10 mm, and the distance was more than 10 mm in 6 cases (Table 2).
Of the 3 failed cases, one failed due to the lesion being so close to the pleura such that the coaxial needle was in the thoracic cavity, one failed due to the tricolored suture with scales being completely embedded in the lung tissue, and another failed due to a coaxial needle displacement in the oblique fissure, as confirmed during VATS. The first two cases occurred in the early attempts and the last case occurred due to the puncture route passing through the dorsal segment while the posterior segment nodules were located in the upper lobe. All three failed cases were resected successfully under the guidance of a puncture point on the pulmonary visceral pleural surfactant.
No major complications occurred during the localization procedure. The common complications included parenchymal hemorrhage (11, 16.2%) and pneumothorax (7, 10.3%). These conditions did not require intervention except for 1 case, in whom thoracentesis occurred immediately after the end of the localization procedure after the last CT scan was performed.
None of the study patients received an incomplete resection. Complete resection was defined as the absence of residual cancer (grossly and microscopically), especially in the resection margins microscopically. Wedge resection was successfully performed for all target SPNs on the first attempt, which was quickly confirmed by surgeon and pathologists. Due to an invasive disease stage with margin distance/tumor size <1, two cases were subsequently converted to segmentectomy or lobectomy, respectively.
Resection margin distance
The minimum resection margin distance was 8 mm in all target lesions, and the median resection margin distance was 14 mm (range, 8–26 mm). There were 16 cases with a resection margin distance between 8 and 10 mm, 32 cases with a distance between 10 to 15 mm, and 20 cases with a distance >15 mm (Table 2).
There were 62 (91.2%) cases with a margin distance to tumor size ratio ≥1 and 6 (8.8%) cases with a margin distance to tumor size ratio <1. Of these six cases, two were subsequently converted to segmentectomy or lobectomy, respectively, due to invasive disease stage, and the other four cases underwent wedge resection due to minimal invasive disease stage.
According to the nodule depth, the nodules were classified into 4 groups: group A (depth ≤10 mm), group B (10 mm< depth ≤20 mm), group C (20 mm< depth ≤30 mm), and group D (depth >30 mm) (Table 3). The median resection margin distance was 11.1, 15, 13, and 18.4 mm, respectively, in groups A, B, C, and D (Table 3). The median resection margin distance was 14 mm in group A + B (depth of nodule ≤20 mm) and in group C + D (depth of nodule >20 mm) (P>0.05). For all nodules in group A, the margin distance to tumor size ratio was greater than 1. There were three cases with a margin distance to tumor size ratio less than one in group B, one case in group C, and two cases in group D. Finally, there were 38 cases with a margin distance to tumor size ratio ≥1 in group A + B (38/41, 92.7%) and 24 cases in group C + D (24/27, 88.9%) (P>0.05) (Table 3).
Table 3
| Nodule depth (mm) | N# | Median resection margin distance (mm) |
Margin distance/tumor size ≥1 (n, %) |
Margin distance/tumor size <1 (n, %) |
|---|---|---|---|---|
| Group A (depth ≤10) | 10 | 11.1 | 10, 100% | 0, 0% |
| Group B (10< depth ≤20) | 31 | 15 | 28, 90.3% | 3, 9.7% |
| Group C (20< depth ≤30) | 22 | 13 | 20, 90.9% | 2, 9.1% |
| Group D (depth >30) | 5 | 18.4 | 4, 80% | 1, 20% |
| Group A + B (depth ≤20) | 41 | 14 | 38, 92.7% | 3, 7.3% |
| Group C + D (depth >20) | 27 | 14 | 24, 88.9% | 3, 11.1% |
#, the numbers of small pulmonary nodules.
Discussion
Research regarding the novel 4-hook and scaled suture device has confirmed its high success rate, feasibility, and good tolerance (9-11). However, there are some shortcomings and a lack of details concerning how to determine an adequate resection margin distance during VATS. In this study, we modified the procedures in CT-guided 4-hook needle with scaled suture localization and VATS for patients with SPNs to obtain sufficient and accurate surgical margin distance, and the preliminary result showed a high success rate, with good efficacy and safety. This study provides a simple and precise method to obtaining sufficient resection margin distance in wedge resection for SPNs using VATS.
In the localization method described by Fan et al. (9), the localizer is placed inside or ahead of the nodule. However, there is a risk of hematogenous dissemination if the localizer is placed inside a malignant nodule. Moreover, if the localizer is implanted farther in front of the nodule, the depth of the nodule cannot be accurately determined due to lung tissue with ductility when it is pulled intraoperatively, which can result in a positive residual tumor margin or an insufficient resection margin. Therefore, in this study, we modified the localization point beside or behind the nodule as close as possible but not inside the nodule to overcome these problems. However, there were four cases that the localizer was placed inside the nodule. There were 55 cases for which the distance between the nodule and the claw was within 10 mm, and the distance was more than 10 mm in 6 cases. The total success rate was 95.6%. Fan et al. (9) reported a success rate of 96.7%, while Chen et al. reported a success rate of 99% (10) with this SPN localization device, and this is expected to further improve.
For wedge resection of SPNs suspected of malignant disease, it is important to obtain an adequate margin distance while preserving as much normal lung tissue as possible. As stated above, no details concerning the means to determining the resection margin accurately have been published in the literature in relation to this novel device (9-11). Usually, surgeons judge the resection distance according to personal experience during operation, which lacks accuracy and repeatability. Therefore, we designed an effective and precise procedure to acquire adequate resection distance during operation. In this procedure, first, the suture and some visceral pleura are pulled gently with oval or curved forceps after the scale in the suture is read. Second, the farthest resection margin distance is measured using a ruler or an oval forceps with a diameter of 10 mm. Third, the farthest resection margin is marked with an electrotome. Fourth, wedge resection is performed using staplers through the markers. The excision margin distance is determined by a reading of the scaled suture, the depth of nodule, and the 3-dimensional relationship between the claw and the nodule. In this study, all SPNs were resected completely on the first attempt using this method.
Ensuring a sufficient and precise resection margin distance is considerably difficult when wedge resection is performed for malignant pulmonary nodules (12). Some combinations of techniques have been used for dual localization to confirm resection margins, such as a hookwire combination with radiotracer/lipiodol or a microcoil combination with indocyanine green (13,14). However, all these methods have some limitations, such as being relatively complex and time-consuming; moreover, they still cannot ensure a sufficient and precise margin distance. In our study, the preoperative use of modified CT-guided 4-hook needle with scaled suture localization combined with an intraoperative measurement procedure improved the accuracy of the resection margin distance. The minimum resection margin distance was 8 mm, and the median resection margin distance was 14 mm. According to the JCOG 0804 study, the minimum resection margin distance for ground-glass opacity (GGO) with a diameter less than 20 mm and consolidation to tumor ratio (CTR) less than 0.25 is 5 mm, which was considered to be sufficient and safe (15). Therefore, the results of our study are satisfactory.
There were 62 (91.2%) cases with a margin distance to tumor size ratio ≥1, and 6 (8.8%) cases with a ratio <1. In group A + B, there were 38 cases with a margin distance to tumor size ratio ≥1 (38/41, 92.7%) and 24 in group C + D (24/27, 88.9%) (P>0.05). The median resection margin distance was 14 mm in group C + D, which was the same as that in group A+B. It can be seen that this method is suitable not only for superficial nodules (depth of nodule ≤20 mm) but also for deep nodules (depth of nodule >20 mm). Next, we will conduct a prospective cohort study to evaluate the feasibility of this approach in the wedge resection of deep pulmonary nodules.
The limitations of the study include its retrospective, single-center design and small sample size. Moreover, the lack of a control group makes it difficult to differentiate the specific benefits of this novel device and method for localization of deep pulmonary nodules during lung wedge resection via VATS. Further investigations are necessary to clarify the applicability and benefits of this novel device and the method for resection of SPNs with different locations.
Conclusions
Modified CT-guided 4-hook needle with scaled suture preoperative localization is a safe, efficient, and precise strategy for wedge resection of SPNs via VATS. Moreover, in terms of locating deep SPNs and obtaining sufficient resection margin distance, the method demonstrated some advantages. While the benefits of this method for deep SPNs should be verified in further studies, we believe that this novel device and localization method can enhance surgical accuracy.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-871/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-871/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-871/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-871/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Li S, Chen M, Wang Y, et al. An Effective Malignancy Prediction Model for Incidentally Detected Pulmonary Subsolid Nodules Based on Current and Prior CT Scans. Clin Lung Cancer 2023;24:e301-10. [Crossref] [PubMed]
- He J, Li N, Chen WQ, et al. China guideline for the screening and early detection of lung cancer(2021, Beijing). Zhonghua Zhong Liu Za Zhi 2021;43:243-68. [Crossref] [PubMed]
- NCCN Clinical Practice Guidelines in Oncology. Lung Cancer Screening. v1, 2020. Available online: www.nccn.org/professionals/physician_gls/f_guidelines.asp.
- Dominguez-Konicki L, Karam AR, Furman MS, et al. CT-guided biopsy of pulmonary nodules ≤10 mm: Diagnostic yield based on nodules' lobar and segmental distribution. Clin Imaging 2020;66:7-9. [Crossref] [PubMed]
- Khandhar SJ, Bowling MR, Flandes J, et al. Electromagnetic navigation bronchoscopy to access lung lesions in 1,000 subjects: first results of the prospective, multicenter NAVIGATE study. BMC Pulm Med 2017;17:59. [Crossref] [PubMed]
- Thistlethwaite PA, Gower JR, Hernandez M, et al. Needle localization of small pulmonary nodules: Lessons learned. J Thorac Cardiovasc Surg 2018;155:2140-7. [Crossref] [PubMed]
- Hsu PK, Chuang LC, Wu YC. Electromagnetic Navigation-Guided Preoperative Localization of Small Malignant Pulmonary Tumors. Ann Thorac Surg 2020;109:1566-73. [Crossref] [PubMed]
- Ajmani GS, Wang CH, Kim KW, et al. Surgical quality of wedge resection affects overall survival in patients with early stage non-small cell lung cancer. J Thorac Cardiovasc Surg 2018;156:380-391.e2. [Crossref] [PubMed]
- Fan L, Yang H, Yu L, et al. Multicenter, prospective, observational study of a novel technique for preoperative pulmonary nodule localization. J Thorac Cardiovasc Surg 2020;160:532-539.e2. [Crossref] [PubMed]
- Chen ZM, Xu JY, Cai WQ, et al. The 4-hook anchor coaxial needle with scaled suture is superior to the double spring coil for preoperative localization. J Thorac Dis 2021;13:4455-63. [Crossref] [PubMed]
- Kong J, Guo J, Zhang H, et al. CT-guided localization techniques of small pulmonary nodules: a prospective non-randomized controlled study on pulmonary nodule localization needle and methylene blue staining with surgical glue. J Thorac Dis 2020;12:6826-35. [Crossref] [PubMed]
- Lin CW, Ko HJ, Yang SM, et al. Computed tomography-guided dual localization with microcoil and patent blue vital dye for deep-seated pulmonary nodules in thoracoscopic surgery. J Formos Med Assoc 2019;118:979-85. [Crossref] [PubMed]
- Doo KW, Yong HS, Kim HK, et al. Needlescopic resection of small and superficial pulmonary nodule after computed tomographic fluoroscopy-guided dual localization with radiotracer and hookwire. Ann Surg Oncol 2015;22:331-7. [Crossref] [PubMed]
- Ujiie H, Kato T, Hu HP, et al. A novel minimally invasive near-infrared thoracoscopic localization technique of small pulmonary nodules: A phase I feasibility trial. J Thorac Cardiovasc Surg 2017;154:702-11. [Crossref] [PubMed]
- Suzuki K, Watanabe SI, Wakabayashi M, et al. A single-arm study of sublobar resection for ground-glass opacity dominant peripheral lung cancer. J Thorac Cardiovasc Surg 2022;163:289-301.e2. [Crossref] [PubMed]
(English Language Editor: J. Gray)




