
Women in thoracic, cardiac and vascular surgery claim for a change in the working situation: an Italian national survey
Highlight box
Key findings
• Women cardiac, thoracic, and vascular surgeons in Italy face many gender-related issues. Surgical exposure is limited and may be crucial in surgeons’ dissatisfaction.
What is known and what is new?
• Women’s participation in the surgical workforce has increased throughout the years.
• In Italy, women thoracic, cardiac, and vascular surgeons face gender-related issues including some episodes of sexual harassment and microaggressions. Surgical exposure is limited, which may be crucial in surgeons’ dissatisfaction.
What is the implication, and what should change now?
• Diversity, equity, and inclusion should become priorities. Surgical societies may address these issues by providing mentorship programs and networking opportunities.
Introduction
Women’s participation in the medical workforce has increased throughout the years, including in surgical specialties (1,2). In Italy, in 2019, women accounted for 46% of all surgical trainees (3).
According to a nationwide analysis conducted in 2018 (4), thoracic surgery was the surgical specialty with the higher proportion of female residents after gynecology (61.7% females versus 38.2% males). The predominance of women over men was also seen in vascular surgery (54.8% females versus 43.5% males), whereas they were still a minority among cardiac surgery residents (59.6% males versus 40.3% females).
However, female surgeons are often professionally disregarded by patients and staff (5), and a glass ceiling seems to prevent most women from reaching leadership positions (6-8). Thoracic and cardiovascular surgery have long been male-dominated fields, where the masculine culture generated a subtle barrier to women’s inclusion (9,10). Apart from some similarities, these three specialties do not share a common training pathway in Italy and the staff and services are usually separated. Despite the significant increase in the representation of women in surgical societies among members, meeting moderators, and sub-committee members, their representation among chairs and society leadership positions has not kept up the pace (11).
In 2020, the Italian Society of Thoracic Surgery asked all the directors of divisions in Italy to report the number of male and female surgeons in their staff (12). Whereas both genders were equally represented among residents, staff surgeons were mainly males. Only two associate professors out of 56 and 1 director of unit out of 82 were women. As far as vascular surgery is concerned, women struggle to enter the academic field as they do not publish as frequently and are cited less than their male counterparts (13). Apart from sporadic reports, literature regarding the gender gap in surgery in Italy is scant (2).
From November through December 2020, an extensive survey was conducted in Italy by the Women In Surgery Italia (WIS Italia), and addressed to Italian female surgeons of all surgical specialties (14). Its results showed that most Italian women surgeons faced gender discrimination at work. This sub-study aimed to analyze the current situation of women in thoracic, cardiac, and vascular surgery surveyed in Italy compared to the other specialties. We present this article in accordance with the STROBE and SURGE reporting checklists (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1123/rc).
Methods
An 83-item questionnaire was designed to capture objective data regarding demographics, surgical practice, training, satisfaction, mentorship, discrimination, and harassment of the responders. The first draft of the questionnaire underwent revisions and retesting by the board members of Women in Surgery Italia (WIS Italia, composed of 7 women surgeons). The WIS Italia executive committee approved the final questionnaire. The ethical approval was waived by the ethics committee due to the nature of the study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The survey was composed of multiple-choice questions, and some responses were scored using a 5-point Likert scale (see Appendix 1).
The REDCap (15,16) online survey was distributed from November through December 2020. All responses were voluntary and anonymous, and electronic informed consent was obtained from responders. The survey was disseminated through a social media campaign (Facebook, LinkedIn, Twitter, and Instagram). It was also sent to 2,871 electronic mails of female surgeons, which were collected from the WIS Italia membership database and a Google search on institutions of employment and surgical department websites. Invitations to participate in the survey were sent to the contacts with up to 3 reminders. Additional invitations were sent via e-mail to the chairpersons of 310 surgical training programs, 1,887 surgical units, 98 surgical societies, and 107 medical boards.
Respondents working in general thoracic, cardiac, and vascular surgery were extracted from the available pool of 3,242 female surgeons who completed the survey. Both specialists and residents who responded to at least 50% of the questions were included in the analysis.
Of note, the residency training pathway in Italy consists for all the surgical specialties of 5 years of training in the field of interest, directly after medical school, with no previous training in general surgery.
Statistical analysis
The respondents were placed into three groups (thoracic, cardiac, and vascular surgery) and separately analyzed. Descriptive statistics were reported for each variable. Categorical data were reported as relative and absolute frequencies; continuous data as median, I, and III quartiles. Wilcoxon-type tests were performed for continuous variables and chi-square test for categorical variables. A significance level of 0.05 was used for the analyses. Computations have been performed with the R 3.6.2 system.
Results
Overall, the multidisciplinary survey obtained 3,242 volunteer respondents. Of them, 1,833 responded to at least 50% of the questions, and 222 identified themselves as thoracic, cardiac, or vascular surgeons. These 222 respondents were included in this sub-analysis.
Demographics, professional status, and family
The cohort comprised 48 cardiac surgeons, 62 thoracic surgeons, and 112 vascular surgeons. Of these, trainees were 16 cardiac (33%), 19 thoracic (31%), and 41 vascular (37%), surgeons. The median age of responders was similar in the three groups, 35 years, with a median of 8 years in practice. The median age for having the first child was 35 overall, higher among thoracic surgeons (37 years). Sixty-six percent of respondents declared that they would have liked to have more children, and 46% stated that the main reason why they did not were mainly professional. The need to delay the first pregnancy for professional reasons was reported by 61% of respondents. Although only 7% of respondents worked less than their spouses, most of them were the primary care providers for home and family. Demographics, professional status, and training are summarized in Table 1.
Table 1
| Variable | Evaluable responders | Cardiac (n=48) | Thoracic (n=62) | Vascular (n=112) | Overall (n=222) | P value |
|---|---|---|---|---|---|---|
| Surgeons, n [%] | 222 | |||||
| Residents | 16 [33] | 19 [31] | 41 [37] | 76 [34] | ||
| Specialists | 32 [66] | 43 [69] | 71 [63] | 146 [66] | ||
| Age, median [IQR] | 220 | 36 [31–40] | 35 [31–41.75] | 35 [30–40] | 35 [30–40] | 0.81 |
| Working years, median [IQR] | 222 | 9 [4–14] | 8 [5–15.75] | 7.5 [4–15] | 8 [4–15] | 0.85 |
| Working hours per week, median [IQR] | 216 | 50 [48–60] | 50 [45–55] | 50 [40–55] | 50 [43–60] | 0.009 |
| Area of practice | 222 | 0.08 | ||||
| Northern Italy | 38 [79] | 34 [55] | 68 [61] | 140 [63] | ||
| Central Italy | 4 [8] | 17 [27] | 25 [22] | 46 [21] | ||
| Southern Italy | 6 [13] | 11 [18] | 19 [17] | 36 [16] | ||
| Academic position, n [%] | 89 | 0.13 | ||||
| PhD students | 3 [16] | 3 [12] | 1 [2] | 7 [8] | ||
| Research fellows | 0 [0] | 0 [0] | 1 [2] | 1 [1] | ||
| Assistant professor | 0 [0] | 2 [8] | 0 [0] | 2 [2] | ||
| Associate professor | 0 [0] | 0 [0] | 2 [4] | 2 [2] | ||
| Full professor | 0 [0] | 1 [4] | 0 [0] | 1] [1] | ||
| Resident | 16 [84] | 19 [76] | 41 [91] | 76 [85] | ||
| Non-academic position, n [%] | 135 | 0.18 | ||||
| Attending surgeon | 27 [96] | 37 [95] | 67 [98] | 131 [97] | ||
| Chief of unit/department | 1 [4] | 2 [5] | 1 [2] | 4 [3] | ||
| Annual income, n [%] | 204 | 0.02 | ||||
| <€60,000 | 35 [85] | 42 [70] | 89 [86] | 166 [81] | ||
| ≥€60,000 | 6 [15] | 18 [30] | 14 [14] | 38 [19] | ||
| Training outside Italy (>3 months), n [%] | 221 | 18 [38] | 17 [27] | 22 [20] | 57 [26] | 0.06 |
| Extra titles (PhD, Master, other higher-level training titles), n [%] | 222 | 14 [29] | 22 [35] | 26 [23] | 62 [28] | 0.22 |
IQR, interquartile range.
Surgical case volume
Thirty-six percent of the respondents partially abandoned surgical activities in favor of other professional activities not including the operating room. The majority (90%) of respondents spent less than 50% of their working hours in surgery, and 64% declared they would spend more time on these activities than they did. Among those who worked in a unit where an endoscopy service was present, 15% stated they were mainly assigned to this service. This percentage was higher among thoracic surgeons (23%). On average, our respondents took part in 33% of all surgical cases performed in their units; however, of 12 high-complexity surgeries per month, less than one is performed by them (Figure 1). In the operating room, only 31% of respondents declared they did not meet any difficulty, while 38% thought they did not receive adequate surgical training. This complaint was particularly common among cardiac surgeons (46% of responders) (Figure 2).

Professional satisfaction and work-life balance
Of the surveyed women surgeons, 7 participants (3%) were in leadership roles (2 associate professors, 1 full professor, 3 chiefs of unit, and 1 chief of department).
Overall satisfaction levels were similar within the three groups, with half of the respondents satisfied with their job most of the time. However, over half complained about their work schedule and found their work-life balance impaired. Fifty-nine percent of all respondents reported prioritizing work over their personal life, while only 23% prioritized their family. Fifty-one percent had to sacrifice their sleep to spend time for self-care, while 36% used to do it to spend time with their family.
Most identified helping patients and acquiring surgical skills as their primary work reward sources. On the other hand, the most common sources of dissatisfaction were the lack of surgical training, work-life balance, and the amount of administrative work (Figure 3). Overall, 84% of thoracic, cardiac, and vascular surgeons would choose their job again.

Work environment, mentorship, and harassment
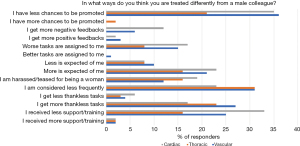
Twenty percent of responders among cardiac, 30% among thoracic, and 31% among vascular surgeons had at least a woman in their units. The percentage of responders who had a female surgeon colleague who was not involved in operating patients was significantly higher among cardiac surgeons (54%) and lower among thoracic and vascular (24%) (P=0.003). The vast majority of responders (90%) had encountered someone they considered a role model during their career, but for only 18% of them, it was a female. Thirty-eight percent of responders stated that women supported other women at work, while only 23% of men did the same. Notwithstanding, when they were asked how they felt about the gender composition of their working team, 31% stated they would prefer working in a gender-balanced team, 21% would rather work with men, and only 4% would rather work with other women. Most responders (74%) thought they had been treated differently due to their gender. This perceived gender influence was negative rather than positive. Thirty-two percent felt they have fewer chances to be promoted than a male colleague (Figure 4).
Ninety-two percent reported hearing the sentence “surgery is not a woman thing” frequently or occasionally from their colleagues. Sixty-one percent of respondents were told that they were “too aggressive”. Most surgeons (59%) reported having been subject to unwelcome sexual advances, verbal or physical conduct of a sexual nature, during their professional career (Table 2). Of these, only 15% have reported it to a supervisor, with higher reporting rates among thoracic surgeons (21%), while 48% handled the situation alone.
Table 2
| Responses | Cardiac (n=43) | Thoracic (n=57) | Vascular (n=101) | Overall (n=201) | P value |
|---|---|---|---|---|---|
| Never, n [%] | 17 [39] | 25 [44] | 41 [40] | 83 [41] | 0.975 |
| Yes, rarely, n [%] | 18 [42] | 22 [39] | 42 [41] | 82 [41] | |
| Yes, frequently, n [%] | 8 [19] | 10 [17] | 18 [18] | 36 [18] | |
| Prefer not to answer, n [%] | 0 [0] | 0 [0] | 1 [1] | 1 [0] |
Discussion
Our results demonstrated that roughly half of women working in cardiac, general thoracic, and vascular surgery in Italy are quite satisfied with their professional status, and they would make the same choice if they had the chance to. However, crucial situations have been identified as obstacles in their career path: the heavy administrative workload, poor surgical training, and profound work-life imbalance were the most frequent sources of stress. As expected (7), concerning gender-sensitive topics, many barriers and critical issues have been highlighted. Our study confirmed that perceived gender bias is still strong in these surgical fields. Discrimination toward female surgeons seems to have evolved from an explicit to a more subtle attitude, as most women in surgery still perceived they were treated differently because of their gender, receiving less consideration, less training, and fewer opportunities for promotion.
Our findings highlighted that our respondents worked at least 50 hours per week. Our search was focused on understanding how this amount of time is spent. In units where surgeons may be more involved in endoscopic cases (namely, thoracic and vascular surgery), women seemed to be frequently assigned to these activities, especially among thoracic surgeons. This finding may explain why, when they do not operate, thoracic surgeons are less involved in research and administrative work than the other two specialties.
The endoscopy service is often considered a suitable alternative to the operating room for surgeons who are less interested in traditional surgery. It may be interesting to understand whether endoscopy cases are actively chosen by the women surgeon, or they are assigned to them as they are excluded from the operating room for other reasons. A response may be suggested by the fact that most responders declared they spent less time in the operating room than they would have liked to.
Our data seemed to be following the situation described by Stephens et al. (17) among cardiothoracic residents in the US, women were more likely to pursue training in minimally invasive surgery and less likely to perform research, and they felt less prepared technically and for practicing independently. Indeed, most respondents, especially cardiac surgeons, identified the lack of surgical training as a critical issue. In a recent study conducted in the US, Meyerson et al. (18) revealed that thoracic surgical faculty gave less operative autonomy to female residents compared to male trainees.
Concerning case volume, a substantial difference compare to male colleagues has been reported in the overall responses. The respondents participated in 33% of all surgical cases in their units, and their involvement as the first surgeon seemed to be limited to low and medium-complexity cases. The most frequent surgical activity reported is assistant surgeon in high complexity cases and team leader in medium and low complexity cases. This situation seemed to be no worse than the other specialties included in this survey (19-21). A similar problem for vascular surgeons was noted by Silva et al. (22), who pointed out how, in Brazil, major arterial surgery was often the domain of men, while women surgeons frequently performed minor venous surgery.
In the last decades, this imbalance was more evident among cardiac surgeons, as they performed no operations as first surgeon or assistant in an average month, which implied that they were involved only as the second assistant in all cases. These data prompt us to consider further the reorganization and development of training pathways in Italy, where the opportunity to develop surgical autonomy in complex cases seems to be limited for junior surgeons.
Among our respondents, thoracic surgeons were the least satisfied with their work-life balance. In general, most responders strive to balance work and personal life. This finding is similar to what has already been described in the literature in the US (17,23). A recent survey (24) conducted on cardiothoracic surgeons in Europe highlighted that many more women than men did not have children. Childbearing trends among thoracic surgeons seem to be delayed as they felt their career would be adversely affected by it (25). This is also confirmed among our respondents, with a reported median age at birth of the first child considerably higher than the national average (14). The balance between professional and personal life is a source of concern for female vascular surgeons too. Around 60% of our responders wanted more than one child but were withheld for professional reasons, 44% and 67% take care of children and household, respectively. These data confirm that family concerns may be actual deterrents to a surgical career.
According to our results, episodes of sexual harassment and microaggressions still occur among female surgeons. The reported incidence of harassment among our responders was similar to other recent surveys conducted on this topic of interest (25-28). These data could be exacerbated by the fact that surgical training is mainly provided by men. Of note, thoracic surgeons seemed to handle sexual harassment complaints better than the other specialties, as they formally reported such experiences more frequently. As already demonstrated by previous studies (29,30), people who have reported being harassed are not only the trainees but also senior women surgeons. Notwithstanding, only a minority reported these episodes. The hesitation in complaining may be due to the male-dominated environment, where most tutoring and power are entrusted to men.
A major concern for our responders was the inadequacy of surgical training. Although this issue may not be related to gender, an interesting point of view has been offered by Wood (9), who recently analyzed how cardiothoracic surgery had one of the highest gender disparities in any medical field. While reflecting on the role of men as allies, the author pointed out an unintended backlash in response to the light shed on sexual harassment. This attitude is counterproductive as many women would miss out on the mentorship of well-intentioned men, or they would be passed over because it is easier for men to supervise other men (31). This was pointed out even between vascular female surgeons in a survey conducted by Smeds and Aulivola (29). The authors declared that although victims of harassment often think that reporting may negatively impact their career, there is also a growing fear in men of mentoring women. This fear could mean lost opportunities for women to advance with good mentorship in a predominantly male field.
Among our respondents, microaggressions seem to frequently occur in daily interactions, which included devaluing assertive women with sexist stereotypes such as “aggressive”, or subtly verbalizing derogatory messages such as “surgery is not a women thing”. These situations can contribute to building a stressful work environment with a negative impact on the workers’ performance. Female and male physicians differ in their practice of medicine in ways that might substantially affect patient outcomes. The presence of female surgeons, as confirmed by recent evidence (32,33), can help organizations improve both patient care quality and financial results. A diversity-friendly environment may be crucial to avoiding frictions that come with change. For these reasons, it is mandatory to educate workers on how to avoid any kind of microaggression, and especially men on how to be allies to women colleagues in common progress toward gender parity. In the last decades, many women surgeons have shed light on gender-related challenges faced throughout their lives and increased awareness on barriers limiting women’s progression in their careers. This awareness led to the birth and progressive diffusion of women’s surgical societies, intending to share experiences and find solutions to common issues (30,34,35). These societies are creating same-gender mentorship networks and projects to improve the working conditions of women at several stages of their careers. In recent years, several societies in Italy and Europe have made a further step forward to address these issues. Women in Surgery Italia developed and launched a structured 1:1 mentorship program for general surgery trainees in collaboration with the University of Padua (36). The Women in General Thoracic Surgery Committee (WGTS) (37), part of the European Society of Thoracic Surgeons, and the Women in CardioThoracic Surgery Committee (38), part of the European Association for Cardio-Thoracic Surgery, began offering a structured program for early-career female thoracic surgeons wishing to acquire surgical skills by offering networking, live webinars, and observerships. In 2021, the American Society for Vascular Surgery (SVS) approved a new section for women, with the intent to address their specific needs, and encourage a pathway to engage and serve the SVS (39). Its mission is to create and strengthen a network of women in vascular surgery, to support their career progression and foster leadership skills that will permit a more robust presence for women in the SVS, leadership roles included.
In this context, social media have served as a valuable tool to enhance networking and mentorship of surgeons (40). Considering the paucity of women in surgical departments, these societies can play a fundamental role in supporting women throughout their careers and, as social media have bridged the gap between surgeons, they should enhance and actively promote sponsorship and mentoring programs between members.
This study has some potential limitations. First, the overall number of responders is high, but the number of respondents in the three categories is small and the distribution method hinders the response rate calculation. Moreover, the identities of the responders were self-declared, and we cannot guarantee there were no multiple submissions from a single responder. Second, a limit to this study is the absence of comparison between genders, as only women have been surveyed. Some critical issues may be shared and independent of gender at certain professional levels in Italy (e.g., residents). Third, the median age of respondents is low, which may hide a possible selection bias that should have been mitigated by the extensive distribution method. The low median age may presumably represent the progressive increase of the number of female surgeons in the last few years. Moreover, the survey was distributed at the end of 2020, during the second wave of COVID-19 in Italy. As the effect of the COVID-19 pandemic offered an added burden on the mental well-being of the surgical workforce, some of the critical issues highlighted may have been worsened by the pandemic (41).
Conclusions
In Italy, women in general thoracic, cardiac, and vascular surgery face gender-related issues including some episodes of sexual harassment and microaggressions. Diversity, equity, and inclusion should become strategic priorities in all today’s institutions and surgical societies, raising awareness and educating coworkers on how to avoid perpetuating the gender gap and create an inclusive workplace. Among our respondents, surgical exposure was reported extremely limited, which may be a deterrent to a surgical career and play a crucial role in surgeons’ dissatisfaction. Surgical societies may address these issues by providing women surgeons with structured mentorship programs and networking opportunities. The contribution of scientific society might strongly impact supporting and retaining women surgeons at different stages of their careers.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE and SURGE reporting checklists. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1123/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1123/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1123/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1123/coif). C.P. serves as an unpaid editorial board member of Journal of Thoracic Disease from October 2022 to September 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The ethical approval was waived by the ethics committee due to the nature of the study. All responses were voluntary and anonymous, and electronic informed consent was obtained from responders. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shin SH, Tang GL, Shalhub S. Integrated residency is associated with an increase in women among vascular surgery trainees. J Vasc Surg 2020;71:609-15. [Crossref] [PubMed]
- Franchi E, Parini S, Capelli G, et al. Women in Transplant Surgery in Italy. Transplantation 2023;107:793-6. [Crossref] [PubMed]
- Formazione Post Laurea - Informazioni sui file relativi alle Scuole di Specializzazione - Open Data dell’istruzione superiore. Accessed May 1, 2022. Available online: http://dati.ustat.miur.it/dataset/formazione-post-laurea/resource/6b8ef5b8-94ad-440f-92e7-83e7977e3085
- Specializzazioni. Le chirurgie sono sempre più al femminile. Lo studio di Anaao Giovani - Quotidiano Sanità. Accessed July 18, 2023. Available online: https://www.quotidianosanita.it/studi-e-analisi/articolo.php?articolo_id=80389
- McKinley SK, Wang LJ, Gartland RM, et al. "Yes, I'm the Doctor": One Department's Approach to Assessing and Addressing Gender-Based Discrimination in the Modern Medical Training Era. Acad Med 2019;94:1691-8. [Crossref] [PubMed]
- Zhuge Y, Kaufman J, Simeone DM, et al. Is there still a glass ceiling for women in academic surgery? Ann Surg 2011;253:637-43. [Crossref] [PubMed]
- Ferrari L, Mari V, Parini S, et al. Discrimination Toward Women in Surgery: A Systematic Scoping Review. Ann Surg 2022;276:1-8. [Crossref] [PubMed]
- Ferrari L, Mari V, De Santi G, et al. Early Barriers to Career Progression of Women in Surgery and Solutions to Improve Them: A Systematic Scoping Review. Ann Surg 2022;276:246-55. [Crossref] [PubMed]
- Wood DE. How can men be good allies for women in surgery? #HeForShe. J Thorac Dis 2021;13:492-501. [Crossref] [PubMed]
- Ikonomidis JS, Boden N, Atluri P. The Society of Thoracic Surgeons Thoracic Surgery Practice and Access Task Force-2019 Workforce Report. Ann Thorac Surg 2020;110:1082-90. [Crossref] [PubMed]
- Humphries MD, Mikityuk A, Harris L, et al. Representation of women in vascular surgery science and societies. J Vasc Surg 2021;74:15S-20S. [Crossref] [PubMed]
- Pompili C, Veronesi G, Novoa NM, et al. Women in thoracic surgery: European perspectives. J Thorac Dis 2021;13:439-47. [Crossref] [PubMed]
- Carnevale M, Phair J, Batarseh P, et al. Gender disparities in academic vascular surgeons. J Vasc Surg 2020;72:1445-50. [Crossref] [PubMed]
- Parini S, Lucidi D, Azzolina D, et al. Women in Surgery Italia: National Survey Assessing Gender-Related Challenges. J Am Coll Surg 2021;233:583-592.e2. [Crossref] [PubMed]
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-81. [Crossref] [PubMed]
- Harris PA, Taylor R, Minor BLThe REDCap consortium, et al. Building an international community of software platform partners. J Biomed Inform 2019;95:103208. [Crossref] [PubMed]
- Stephens EH, Robich MP, Walters DM, et al. Gender and Cardiothoracic Surgery Training: Specialty Interests, Satisfaction, and Career Pathways. Ann Thorac Surg 2016;102:200-6. [Crossref] [PubMed]
- Meyerson SL, Sternbach JM, Zwischenberger JB, et al. The Effect of Gender on Resident Autonomy in the Operating room. J Surg Educ 2017;74:e111-8. [Crossref] [PubMed]
- Lucidi D, Parini S, Reale M, et al. Women in Surgery Italia: what are the opportunities in the operatory room? Results from a nationwide interdisciplinary survey. Updates Surg 2022;74:803-16. [Crossref] [PubMed]
- Scerrati A, Angelini C, Madoglio A, et al. Status of Women in Neurosurgery: Results from a National Survey in Italy. World Neurosurg X 2023;18:100149. [Crossref] [PubMed]
- Lucidi D, Reale M, Trecca EMC, et al. Perception of Gender Bias in Otolaryngology and Head & Neck Surgery - A Comparative Study. Ann Maxillofac Surg 2023;13:57-63. [Crossref] [PubMed]
- Silva FCS, Cerqueira MMBDF, Mercês MCD, et al. Strengths and Barriers for Women in Vascular Surgery: The Brazilian Perspective. Eur J Vasc Endovasc Surg 2020;60:165-6. [Crossref] [PubMed]
- Antonoff MB, David EA, Donington JS, et al. Women in Thoracic Surgery: 30 Years of History. Ann Thorac Surg 2016;101:399-409. [Crossref] [PubMed]
- Pompili C, Opitz I, Backhus L, et al. The impact of gender bias in cardiothoracic surgery in Europe: a European Society of Thoracic Surgeons and European Association for Cardio-Thoracic Surgery survey. Eur J Cardiothorac Surg 2022;61:1390-9. [Crossref] [PubMed]
- Nayyar A, Scarlet S, Strassle PD, et al. 85.06 A National Survey of Sexual Harassment Among Surgeons. Academic Surgical Congress Abstracts Archive. Accessed May 6, 2022. Available online: https://www.asc-abstracts.org/abs2019/85-06-a-national-survey-of-sexual-harassment-among-surgeons/
- Nukala M, Freedman-Weiss M, Yoo P, et al. Sexual Harassment in Vascular Surgery Training Programs. Ann Vasc Surg 2020;62:92-7. [Crossref] [PubMed]
- Freedman-Weiss MR, Chiu AS, Heller DR, et al. Understanding the Barriers to Reporting Sexual Harassment in Surgical Training. Ann Surg 2020;271:608-13. [Crossref] [PubMed]
- Vargas EA, Brassel ST, Cortina LM, et al. #MedToo: A Large-Scale Examination of the Incidence and Impact of Sexual Harassment of Physicians and Other Faculty at an Academic Medical Center. J Womens Health (Larchmt) 2020;29:13-20. [Crossref] [PubMed]
- Smeds MR, Aulivola B. Gender disparity and sexual harassment in vascular surgery practices. J Vasc Surg 2020;72:692-9. [Crossref] [PubMed]
- Ceppa DP, Dolejs SC, Boden N, et al. Sexual Harassment and Cardiothoracic Surgery: #UsToo? Ann Thorac Surg 2020;109:1283-8. [Crossref] [PubMed]
- Byerley JS. Mentoring in the Era of #MeToo. JAMA 2018;319:1199-200. [Crossref] [PubMed]
- Gomez LE, Bernet P. Diversity improves performance and outcomes. J Natl Med Assoc 2019;111:383-92. [Crossref] [PubMed]
- Wallis CJ, Ravi B, Coburn N, et al. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ 2017;359:j4366. [Crossref] [PubMed]
- Ceppa DP, Antonoff MB, Tong BC, et al. 2020 Women in Thoracic Surgery Update on the Status of Women in Cardiothoracic Surgery. Ann Thorac Surg 2022;113:918-25. [Crossref] [PubMed]
- Giuliano K, Ceppa DP, Antonoff M, et al. Women in Thoracic Surgery 2020 Update-Subspecialty and Work-Life Balance Analysis. Ann Thorac Surg 2022;114:1933-42. [Crossref] [PubMed]
- Pierobon ES, Capelli G, Frigerio I, et al. Mentor WIS: an Italian mentorship programme for female surgeons. Br J Surg 2023;110:983-4. [Crossref] [PubMed]
- ESTS Women in General Thoracic Surgery | European Society of Thoracic Surgeons. Accessed July 18, 2023. Available online: https://www.ests.org/about_ests/committees/539/ests_women_in_general_thoracic_surgery/public
- Women in Cardio-Thoracic Surgery. EACTS. Accessed July 18, 2023. Available online: https://www.eacts.org/resources/women-in-cardio-thoracic-surgery/
- SVS Women’s Section | Society for Vascular Surgery. Accessed July 18, 2023. Available online: https://vascular.org/vascular-specialists/networking/svs-womens-section
- Luc JGY, Stamp NL, Antonoff MB. Social Media as a Means of Networking and Mentorship: Role for Women in Cardiothoracic Surgery. Semin Thorac Cardiovasc Surg 2018;30:487-95. [Crossref] [PubMed]
- Lai J, Ma S, Wang Y, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open 2020;3:e203976. [Crossref] [PubMed]



