
Compliance and rehabilitation effects of Zheng’s supine rehabilitation exercise performed at home among patients with chronic obstructive pulmonary disease: a retrospective study
Highlight box
Key findings
• Home Zheng’s supine rehabilitation exercise (ZSRE) can be performed with high compliance by elderly patients with severe or extremely severe chronic obstructive pulmonary disease (COPD) and can reduce the number of readmissions.
What is known and what is new?
• The home ZSRE compliance rate was 57.96%. The number of readmissions significantly increased in the non-rehabilitation group and significantly decreased in the one- and multiple-session rehabilitation groups.
What is the implication, and what should change now?
• The study indicates the effectiveness of ZSRE on patients with COPD.
Introduction
Chronic obstructive pulmonary disease (COPD) is an airway disease characterized by progressive exacerbation of shortness of breath, declining exercise endurance and quality of life, and increasing annual medical expenses (1). Because the prognosis is related to the frequency of acute exacerbations, prevention of acute exacerbation events is one of the main objectives of long-term management of COPD (2-4). Pulmonary rehabilitation is an important technique for long-term management in patients with COPD because it can reduce medical expenses, improve dyspnea and exercise endurance, and reduce the frequency of acute exacerbations and hospitalizations (5-8). However, previous studies showed that because of inconvenient transport options (9). and lack of help from family members, up to 49.6% of patients were unwilling to go to medical institutions for pulmonary rehabilitation (10) and up to 31.08% of patients withdrew from pulmonary rehabilitation (11).
We have developed a simple, safe, and easy-to-follow exercise called Zheng’s supine rehabilitation exercise (ZSRE) to enable patients with COPD to perform pulmonary rehabilitation exercise at home, improve the compliance of patients with advanced or severe COPD, reduce the dependence on family members to assist with pulmonary rehabilitation, and safely implement these procedures. ZSRE involves three actions (pull-ups, bridging, and air stepping) and is helpful for increasing exercise endurance, alleviating symptoms, and relieving dyspnea in patients with acute exacerbation of COPD (AECOPD) (12,13). Since 2014, our department has been providing routine health education to patients hospitalized because of AECOPD, including education on the etiology, symptoms, treatment, inhalation methods, prognostic factors, and ZSRE for COPD. During hospitalization, patients are required to perform 3 sessions of ZSRE daily with at least 15 repetitions of each action per session, and there is no restriction on the completion time.
In the present study, patients who had received COPD education and ZSRE training were interviewed by telephone to investigate their compliance with ZSRE at home after discharge and its effect on rehospitalization due to acute exacerbation in both the previous and following years. We present this article in accordance with the SURGE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-779/rc).
Methods
Sample and design
This retrospective study was performed to assess compliance with home ZSRE and its rehabilitation effect on rehospitalization of patients with COPD. We used the hospital inpatient medical administration system to identify patients with AECOPD who were hospitalized on the 26th floor of the National Clinical Research Center for Respiratory Disease and who had received COPD education and ZSRE training from September 2015 to August 2016. We then contacted the patients and their family through the telephone records in our medical administration system. If the patients and their family agreed to be interviewed by telephone, the research group administered a follow-up survey. All patients provided informed consent to participate in the study. The last included patient follow-up was completed on 30 June, 2019. The study was approved by the ethics committee of the First Affiliated Hospital of Guangzhou Medical University (2016 No. 28). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
General aspects and data collection
Data on age, sex, height, weight, lung function and blood gas analysis of patients with AECOPD hospitalized on the 26th floor of the National Clinical Research Center for Respiratory Disease from 1 September, 2015 to 31 August, 2016 were obtained from the hospital inpatient medical administration system.
The inclusion criteria of the study were as follows: (I) men or women aged 40 to 95 years, (II) the lung function in the previous year was: forced vital capacity rate of one second (FEV1)/forced vital capacity (FVC) <70% after using bronchodilator, (III) ability to perform ZSRE under instruction. AECOPD was confirmed by a set of criteria including signs, symptoms, and previous pulmonary function test results as per the COPD Diagnosis and Treatment Guidelines established by the Chinese Society of Respiratory Diseases, Chinese Medical Association, in 2013. The exclusion criteria were as follows: (I) severe malignant tumors, (II) audiovisual and cognitive dysfunction, (III) inability to complete the ZSRE, (IV) uncontrolled active tuberculosis, (V) heart, liver, or kidney failure, (VI) unstable angina or myocardial infarction in the past 6 months, (VII) connective tissue-related vascular disease, or (VIII) tracheal incision.
On the survey sheet, the patients and their family were questioned on the following: (I) the number of sessions of home ZSRE performed per day after discharge, over a period of 1 year, with at least 15 repetitions of each action per session (none, one session/day, or more than two sessions/day); (II) the number of hours of home oxygen treatment received after discharge (0, ≤15, or >15 h/day); (III) the number of hospitalizations in the year prior to completion of COPD education and ZSRE training (the number of readmissions mentioned in article was the number of readmissions to hospital for AECOPD within a timespan of a year after discharge obtained by questioning the patient and/or family members); (IV) the number of hospitalizations in the year following the completion of COPD education and ZSRE training; (V) the number of hours of home noninvasive ventilation after discharge (patients receiving noninvasive ventilation were classified as “yes”, otherwise was classified as “no”); (VI) home medication on sustained release theophylline formulation/carbocisteine/long acting muscarine anticholinergic (LAMA)/long acting β2-agonist (LABA)/inhaled corticosteroids (ICS); and (VII) deaths following 1 year after discharge from hospital.
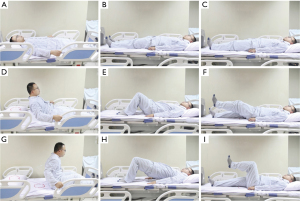
ZSRE involves three actions (12): (I) pull-ups—the patient grasps the edge of the bed with his or her hand, pulls the upper body to the upright sitting position, and maintains this position for 5 s before slowly lying down while holding the edge of the bed; (II) bridging—the patient begins lying supine with both knees bent and feet flat on the bed, then raises the buttocks away from the bed by approximately 10 to 15 cm; and (III) air stepping—the patient begins lying supine with both knees bent, then performs alternate cycling motions with the lower limbs raised while the upper body remains motionless; this is continued until the lower limbs are fatigued. ZSRE has the following advantages: (I) it can strengthen the upper and lower limbs, abdominal muscles, diaphragm, and back muscles; (II) the exercise intensity, frequency, and duration can be tailored to the individual patient’s needs; (III) the patient can rest in bed whenever tired; (IV) minimal care is required, and it can be performed anywhere at any time; and (V) it does not require any equipment.
Statistical analysis
The patients were divided into three groups according to the number of sessions of home ZSRE performed per day: the non-rehabilitation group, one-session rehabilitation group, and multiple-session rehabilitation group. The statistical analysis was performed using statistical software (SPSS v24.0; IBM Corp., Armonk, NY, USA). Measurement data are presented as mean ± standard deviation. Measurement data were presented as median (quartile) if the variable did not follow a normal distribution. One-way analysis of variance, Kruskal-Wallis test, the Chi-squared test, and Fisher’s exact probability method were used to compare differences among the groups. The frequency and composition ratio were used to describe the distribution of qualitative data. All tests were bilateral. A P value of <0.05 was considered statistically significant.
Results
General data
In total, 211 inpatients with AECOPD were hospitalized on the 26th floor of the National Clinical Research Center for Respiratory Disease and received COPD education and ZSRE training from 1 September 2015 to 31 August 2016. Among the 211 patients, 157 (74.4%) were willing to conduct the telephone interview (Table 1). The patients were divided into three groups based on the number of sessions of ZSRE they performed at home after discharge: the non-rehabilitation group (n=66), one-session rehabilitation group (n=41), and multiple-session rehabilitation group (n=50). There were no differences in age, height, weight, partial pressure of carbon dioxide or oxygenation index before discharge, FEV1, home oxygen therapy or received home-based noninvasive ventilation among the groups.
Table 1
| General information | Non-rehabilitation (n=66) | One-section rehabilitation group (n=41) | Multiple-sections rehabilitation group (n=50) | F/h value | P value |
|---|---|---|---|---|---|
| Age (year) | 70.38±8.69 | 70.02±8.08 | 67.8±8.59 | 1.413 | 0.247 |
| Height (cm) | 158.7±24.5 | 164.63±7.5 | 162.46±9.55 | 1.476 | 0.232 |
| Weight (kg) | 55.98±16.81 | 55.71±10.78 | 52.3±8.37 | 1.224 | 0.297 |
| Blood oxygen level before discharge (%) | 99.14±28.66 | 90.33±22.08 | 99.06±28.54 | 1.581 | 0.209 |
| Carbon dioxide partial pressure (mmHg) | 44.7 (19.3) | 44.3 (14) | 45.4 (12.6) | 2.154 | 0.341 |
| Oxygen saturation (%) | 96.27±2.72 | 95.45±2.76 | 96.6±2.36 | 2.248 | 0.109 |
| Oxygenation index | 341.87±98.84 | 311.48±76.15 | 341.6±98.4 | 1.581 | 0.209 |
| Home oxygen therapy groups (0, ≤15, or >15 h/day) | 1.927 | 0.749 | |||
| 0 | 16 (24.24) | 10 (24.39) | 10 (20.0) | ||
| ≤15 | 33 (50.0) | 23 (56.1) | 31 (62.0) | ||
| >15 | 17 (25.76) | 8 (19.51) | 9 (18.0) | ||
| Whether the family is non-invasive (yes/no) | 4.871 | 0.088 | |||
| No | 52 (78.79) | 28 (68.29) | 30 (60.0) | ||
| Yes | 14 (21.21) | 13 (31.71) | 20 (40.0) | ||
| Pulmonary function | |||||
| FEV1 | 1.03±0.58 | 0.96±0.45 | 0.88±0.46 | 0.924 | 0.400 |
| FEV1 (%) | 42.39±26.43 | 38.99±17.95 | 36.18±19.7 | 0.893 | 0.412 |
| FEV1/FVC (%) | 58.88±21.43 | 60.69±17.48 | 58.65±21.27 | 0.095 | 0.909 |
| Number of hospitalizations in the previous year (times/year) | 1.06±0.76 | 1.27±0.78 | 1.16±0.91 | 0.829 | 0.438 |
| Number of hospitalizations in the following year (times/year) | 1.44±1.17##&& | 0.78±0.82**&& | 0.66±0.75**&& | 10.641 | <0.001 |
| One year mortality (%) | 13.64 | 12.20 | 10.0 | 0.353 | 0.838 |
Data are presented as n (%), mean ± standard deviation or median (quartile). Compared with non-rehabilitation group: **, P<0.01. Compared with one-section rehabilitation group: ##, P<0.01. Compared with the number of hospitalizations in the previous year before rehabilitative training: &&, P<0.01. COPD, chronic obstructive pulmonary disease; FEV1, forced vital capacity rate of one second; FVC, forced vital capacity.
Home medicines
There were no significant differences in the use of home medicines, including slow-release theophylline, carbocysteine, LABA, LAMA, or ICS, among the non-rehabilitation group, one-session group, and multiple-session group (P>0.05) (Table 2).
Table 2
| Drug | Non-rehabilitation (n=66) | Rehabilitation one group (n=41) | Rehabilitation multiple group (n=50) | P |
|---|---|---|---|---|
| Sustained release aminophylline | 0.144 | |||
| No | 16 (24.24) | 8 (19.51) | 5 (10.0) | |
| Yes | 50 (75.76) | 33 (80.49) | 45 (90.0) | |
| Carbocysteine | 0.765 | |||
| No | 12 (18.18) | 9 (21.95) | 8 (16.0) | |
| Yes | 54 (81.82) | 32 (78.05) | 42 (84.0) | |
| LAMA | 0.168 | |||
| No | 11 (16.67) | 7 (17.07) | 15 (30.0) | |
| Yes | 55 (83.33) | 34 (82.93) | 35 (70.0) | |
| LABA | 0.454 | |||
| No | 20 (30.3) | 12 (29.27) | 20 (40.0) | |
| Yes | 46 (69.7) | 29 (70.73) | 30 (60.0) | |
| ICS | 0.155 | |||
| No | 45 (68.18) | 27 (65.85) | 41 (82.0) | |
| Yes | 21 (31.82) | 14 (34.15) | 9 (18.0) | |
Data are presented as n (%). LAMA, long acting muscarine anticholinergic; LABA, long acting β2-agonist; ICS, inhaled corticosteroids.
Number of hospitalizations prior to and following education and training
The mean number of hospitalizations in the year prior to receiving COPD education and ZSRE training in the non-rehabilitation group, one-session group, and multiple-session group was 1.06±0.75, 1.27±0.78, and 1.16±0.91, respectively (P>0.05), while that in the year following the receipt of COPD education and ZSRE training was 1.44±1.17, 0.78±0.82, and 0.66±0.75, respectively (P<0.05) (Table 1). Compared with the year prior to education and training, the number of hospitalizations in the following year was significantly increased in the non-rehabilitation group and significantly decreased in both the one-session and multiple-session groups. The difference did not reach statistical significance in spite of a lower number of readmissions to hospital for AECOPD within a year after discharge in the multiple-session group (0.66±0.75) compared with one-session group (0.78±0.82).
One-year mortality
The 1-year mortality rate at the end of the following year in the non-rehabilitation group, one-session group, and multiple-session group was 13.64%, 12.20%, and 10.00%, respectively (P>0.05); the multiple-session group showed a decreasing trend (Table 1).
Discussion
Similar to previous study, this study showed that adherence to in ZSRE at home in patients with COPD reduced the frequency of COPD exacerbations and the higher the patient adherence to ZSRE, the less the number of readmissions to hospital for AECOPD after discharge. Pulmonary rehabilitation is one of the main treatments for COPD and has the same clinical value as medical therapy. However, the duration of pulmonary rehabilitation affects its efficacy (14,15). The effect of 6 to 12 weeks of pulmonary rehabilitation exercise begins to decline in the third month and (16) can only be maintained for 1 year (17,18). Therefore, long-term rehabilitation is needed to maintain the effect of pulmonary rehabilitation. As such, it is important to consider compliance with long-term pulmonary rehabilitation in patients with COPD (19,20).
The factors that affect compliance with long-term pulmonary rehabilitation in patients with COPD include the caregiver’s suggestion to undergo pulmonary rehabilitation (21,22), the patient’s health status (depression, exercise tolerance, and smoking), family and social support (transportation, economic status, and family support), and degree of entertainment provided by the pulmonary rehabilitation activities (9,10,23,24). The convenience of traveling to the rehabilitation site and assistance from family members are also crucial factors for elderly patients and patients with severe COPD (25).
As long as it is supervised, the effect of pulmonary rehabilitation at home is identical to that performed in hospitals or medical rehabilitation institutions (26-28). Therefore, pulmonary rehabilitation at home is a prerequisite for improving compliance with long-term pulmonary rehabilitation in patients with COPD. We have developed ZSRE, an innovative pulmonary rehabilitation regimen, to enable patients with COPD to safely perform pulmonary rehabilitation exercises at home, improve the compliance of elderly patients and patients with severe COPD, and reduce dependence on family members (Figure 1) (12). Since 2014, all inpatients with AECOPD admitted to our department have received COPD education and ZSRE training from the day of admission onward. The basic exercise prescription involves three sessions per day, with at least 15 repetitions of each action per session. However, the amplitude, speed, maximum repeat number, daily frequency of each action, and resting duration can be adjusted according to the conditions of the patient.
This was a retrospective study. We followed up patients who were hospitalized for AECOPD, received COPD education and ZSRE training, and had been discharged for >1 year. Ninety-one of 157 patients (57.96%) with COPD insisted on performing ZSRE at home; among them, 50 performed at least two sessions per day and 41 performed one session per day. Even without long-term follow-up, the patients’ compliance with home ZSRE was much higher than compliance with inhaled drugs (29). This might be explained by the simple movements of ZSRE, the individualized exercise intensity and duration, no requirement for external help, and no restriction or requirement on the facilities. As some patients with COPD are elderly with decreased comprehension ability and memory, pulmonary rehabilitation exercises must be simple and easy to master. ZSRE is simple in this respect because patients only require one or two trainings by professional rehabilitation personnel during hospitalization. ZSRE also requires no specific facilities and induces no additional economic burden, and it can be performed in the early morning, daytime, or nighttime. Further, there is no need to travel to a hospital or medical rehabilitation institution. Finally, during exercise, the patients can stop at any time and lie directly on their bed, thus avoiding accidents that may occur during rehabilitation on the ground.
The treatment goal in patients with stable COPD is to improve symptoms, improve exercise tolerance, and prevent acute exacerbations. Our follow-up study showed significant differences in the number of rehospitalizations within 1 year following discharge among the non-rehabilitation group, one-session rehabilitation group, and multiple-session rehabilitation group. Compared with the previous year, the number of hospitalizations increased in the non-rehabilitation group but decreased in both the one-session and multiple-session rehabilitation groups. This is consistent with previous research reports (30). However, there were no differences in the 1-year mortality rate in the following year among the three groups (non-rehabilitation group, 13.64%; one-session rehabilitation group, 12.20%; and multiple-session rehabilitation group, 10.00%; F value =0.353, P=0.838). This result may have been related to the low number of patients. Nevertheless, there was a decreasing trend in the 1-year mortality rate in the multiple-session rehabilitation group compared with the non-rehabilitation and one-session rehabilitation groups. This finding is inconsistent with the highest actual need for noninvasive ventilation in the multiple-session rehabilitation group.
In addition, although the mean age of the patients in the non-rehabilitation, one-session rehabilitation, and multiple-session rehabilitation groups was as high as 70.38±8.69, 70.02±8.08, and 67.8±8.59 years, respectively, and although their pulmonary function (FEV1 % predicted) was 42.39%±26.43%, 38.99%±17.95%, and 36.18%±19.7% of the predicted value, respectively, 57.96% of patients insisted on performing ZSRE at home without supervision, and with no adverse events such as decreased hypoxemia, acute dyspnea, and arrhythmia.
Elderly patients and patients with severe COPD showed high compliance with ZSRE, which is simple, effective, safe, and economical and can reduce the number of rehospitalizations for AECOPD.
We have to admit that there are limitations in this retrospective study. The number of sessions of home ZSRE performed per day after discharge in COPD patients may not be absolutely accurate because it depends on the patients’ responses over the telephone. But combined with our previous article show that home ZSRE can be performed with high compliance by elderly patients with severe or extremely severe COPD (12). We firmly believe that the conclusions of this study are credible. We also expect that a multicenter prospective study further confirms the effectiveness of home ZSRE on patients with COPD.
Conclusions
The research results show that home ZSRE can be performed with high compliance by elderly patients with severe or extremely severe COPD, and can reduce the number of readmissions.
Acknowledgments
We would like to thank Guansheng Su for his help in statistical verification.
Funding: The study was supported by
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-779/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-779/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-779/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-779/coif). Z.C. is an employee of Yabao Pharmaceutical Group Co., Ltd. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the ethics committee of the First Affiliated Hospital of Guangzhou Medical University (2016 No. 28). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All patients provided informed consent to participate in the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2023 REPORT). Available online: https://goldcopd.org/.
- Celli BR, Decramer M, Wedzicha JA, et al. An Official American Thoracic Society/European Respiratory Society Statement: Research questions in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2015;191:e4-e27. [Crossref] [PubMed]
- Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet 2007;370:786-96. [Crossref] [PubMed]
- Man WD, Puhan MA, Harrison SL, et al. Pulmonary rehabilitation and severe exacerbations of COPD: solution or white elephant? ERJ Open Res 2015;1:00050-2015. [Crossref] [PubMed]
- Celli BR, MacNee WATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2004;23:932-46. [Crossref] [PubMed]
- Kon SS, Canavan JL, Man WD. Pulmonary rehabilitation and acute exacerbations of COPD. Expert Rev Respir Med 2012;6:523-31; quiz 531. [Crossref] [PubMed]
- Alcaraz FG. Pulmonary rehabilitation in chronic obstructive pulmonary disease Enferm Clin 2015;25:357-9. (Review). [Crossref] [PubMed]
- Cornelison SD, Pascual RM. Pulmonary Rehabilitation in the Management of Chronic Lung Disease. Med Clin North Am 2019;103:577-84. [Crossref] [PubMed]
- Arnold E, Bruton A, Ellis-Hill C. Adherence to pulmonary rehabilitation: A qualitative study. Respir Med 2006;100:1716-23. [Crossref] [PubMed]
- Taylor R, Dawson S, Roberts N, et al. Why do patients decline to take part in a research project involving pulmonary rehabilitation? Respir Med 2007;101:1942-6. [Crossref] [PubMed]
- Garrod R, Marshall J, Barley E, et al. Predictors of success and failure in pulmonary rehabilitation. Eur Respir J 2006;27:788-94. [Crossref] [PubMed]
- Lu H, Liu N, Hu JY, et al. The effectiveness, safety and compliance of Zheng's supine rehabilitation exercise as a rehabilitation programme among elderly patients with AECOPD. Clin Respir J 2020;14:533-40. [Crossref] [PubMed]
- Burtin C, Decramer M, Gosselink R, et al. Rehabilitation and acute exacerbations. Eur Respir J 2011;38:702-12. [Crossref] [PubMed]
- Bourbeau J. Making pulmonary rehabilitation a success in COPD. Swiss Med Wkly 2010;140:w13067. [Crossref] [PubMed]
- Watz H, Pitta F, Rochester CL, et al. An official European Respiratory Society statement on physical activity in COPD. Eur Respir J 2014;44:1521-37. [Crossref] [PubMed]
- Solanes I, Güell R, Casan P, et al. Duration of pulmonary rehabilitation to achieve a plateau in quality of life and walk test in COPD. Respir Med 2009;103:722-8. [Crossref] [PubMed]
- Troosters T, Gosselink R, Decramer M. Short- and long-term effects of outpatient rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Am J Med 2000;109:207-12. [Crossref] [PubMed]
- Sewell L, Singh SJ, Williams JE, et al. How long should outpatient pulmonary rehabilitation be? A randomised controlled trial of 4 weeks versus 7 weeks. Thorax 2006;61:767-71. [Crossref] [PubMed]
- Hoaas H, Andreassen HK, Lien LA, et al. Adherence and factors affecting satisfaction in long-term telerehabilitation for patients with chronic obstructive pulmonary disease: a mixed methods study. BMC Med Inform Decis Mak 2016;16:26. [Crossref] [PubMed]
- Lindenauer PK, Stefan MS, Pekow PS, et al. Association Between Initiation of Pulmonary Rehabilitation After Hospitalization for COPD and 1-Year Survival Among Medicare Beneficiaries. JAMA 2020;323:1813-23. [Crossref] [PubMed]
- Oliver SM. Living with failing lungs: the doctor-patient relationship. Fam Pract 2001;18:430-9. [Crossref] [PubMed]
- Zimmerman BW, Brown ST, Bowman JM. A self-management program for chronic obstructive pulmonary disease: relationship to dyspnea and self-efficacy. Rehabil Nurs 1996;21:253-7. [Crossref] [PubMed]
- Oates GR, Hamby BW, Stepanikova I, et al. Social Determinants of Adherence to Pulmonary Rehabilitation for Chronic Obstructive Pulmonary Disease. COPD 2017;14:610-7. [Crossref] [PubMed]
- Grosbois JM, Charlet Deffontaines L, Caron A, et al. Influence of DISC behavioral profile on the short- and long-term outcomes of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. Respir Med Res 2020;77:24-30. [Crossref] [PubMed]
- Young P, Dewse M, Fergusson W, et al. Respiratory rehabilitation in chronic obstructive pulmonary disease: predictors of nonadherence. Eur Respir J 1999;13:855-9. [Crossref] [PubMed]
- Vasilopoulou M, Papaioannou AI, Kaltsakas G, et al. Home-based maintenance tele-rehabilitation reduces the risk for acute exacerbations of COPD, hospitalisations and emergency department visits. Eur Respir J 2017;49:1602129. [Crossref] [PubMed]
- Zanaboni P, Hoaas H, Aarøen Lien L, et al. Long-term exercise maintenance in COPD via telerehabilitation: a two-year pilot study. J Telemed Telecare 2017;23:74-82. [Crossref] [PubMed]
- Jenkins AR, Gowler H, Curtis F, et al. Efficacy of supervised maintenance exercise following pulmonary rehabilitation on health care use: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 2018;13:257-73. [Crossref] [PubMed]
- Toy EL, Beaulieu NU, McHale JM, et al. Treatment of COPD: relationships between daily dosing frequency, adherence, resource use, and costs. Respir Med 2011;105:435-41. [Crossref] [PubMed]
- Ryrsø CK, Godtfredsen NS, Kofod LM, et al. Lower mortality after early supervised pulmonary rehabilitation following COPD-exacerbations: a systematic review and meta-analysis. BMC Pulm Med 2018;18:154. [Crossref] [PubMed]


