
Factors influencing surgical choice and anxiety in patients with pulmonary nodules smaller than 8 mm
Highlight box
Key findings
• Our findings suggest that the ability to perform activity of daily living, the presence of solid and multiple nodules, and a family history of lung cancer put patients at greater risk of experiencing anxiety during treatment decisions.
What is known and what is new?
• At present, there are few reports about the reasons why patients with small pulmonary nodules choose surgical treatment at home and abroad. In terms of lung nodule anxiety, the current study shows that patients who are older, smoke, and less educated seem to be more prone to anxiety.
• Our research shows that the most common reasons for patients to choose surgery are doctor-patient communication and patient psychological stress, and patients with poor daily activity ability, solid and multiple lung nodules, and a family history of lung cancer are more likely to experience anxiety.
What is the implication, and what should change now?
• Promote patient-centered service forms, and strive to improve the mental health of patients. Enhance doctor-patient communication, and communicate the points that patients care about with appropriate words.
Introduction
Millions of patients each year are diagnosed with pulmonary nodules, with this number expected to increase as more people undergo screening computed tomography (CT) (1). Even though most ground glass nodules (GGNs) present as incipient, minimally invasive adenocarcinomas (MIAs), they convey a significant psychological burden to patients and their families (2). Given the serious implications of pulmonary nodules, clinicians are advised to better understand the emotional needs of their patients (3,4). According to the 2020 National Comprehensive Cancer Network (NCCN) guidelines, long-term follow-up is recommended for pulmonary nodules ≤8 mm, without the requirement for surgical intervention. However, some patients still opt for surgical removal of pulmonary nodules.
Recognizing the increasing emphasis on patient-centered care, the American Thoracic Society has recently called for additional study of the psychologic effects that patients experience when making treatment decisions (5). While the preponderance of patients with small pulmonary nodules will opt for non-invasive surveillance to manage their condition, a non-trivial percentage still elects to undergo surgical excision. One of the key aims of our study was to better understand the reasons why certain patients choose to surgically remove their small (≤8 mm) pulmonary nodules, rather than submitting to observation.
Based on the patient-centered communication model, we hypothesized that patients would experience anxiety owing to their own condition, the nature of nodules, and other factors when facing surgical treatment. Specifically, we posited that high-quality doctor-patient communication and the psychological stress caused by a positive pulmonary nodules test would have an important influence on the choice of treatment for patients with small nodules. Our experience was that many patients overestimate their risk of cancer, and these patients seem to suffer more anxiety than those who think they are at low-risk. Thus, from the perspectives of clinical communication and nodular monitoring, we aimed to identify the root causes of anxiety experienced by patients making treatment choices (1). We present this article in accordance with the SURGE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1701/rc).
Methods
Study population
The inclusion criteria were as follows: (I) participants belonging to our local hospital catchment area; (II) American Society of Anesthesiologists (ASA) grade ≤ III; (III) alertness and ability to express basic information normally; (IV) age 18–90 years; (V) nodules <8 mm; and (VI) hospitalization for thoracoscopic surgery. Patients were excluded if they were: (I) unwilling to participate in the research; (II) already diagnosed with lung cancer; or (III) currently (or previously) using psychotropic drugs [including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), sedatives, and antidepressants] and alcohol abuse.
Survey instrument
We designed a self-management questionnaire covering four aspects: (I) patient characteristics; (II) nodule-specific knowledge; (III) patient-clinician communication; and (IV) nodule-specific distress. A series of pilot tests were conducted to assess the content, relevance, and understandability of the questionnaire, with 5 patients randomly selected for further in-depth investigation of factors that might influence their choice of surgical treatment and perioperative anxiety (4). The final survey tool consisted of 28 items, including validated scales and new questions.
Survey administration
Data were collected from October 2021 to February 2022. Participants were recruited from the Department of Thoracic Surgery of Taizhou Hospital. The content and purpose of the questionnaire were explained to all patients. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Taizhou Hospital Research Ethics Committee (No. K202107138), and informed consent was taken from all the patients. Patients were able to access the questionnaire by scanning a quick-response (QR) code (Figure 1).
Outcome measures
The primary outcome of this trial was pulmonary nodule-specific distress, as measured by the Impact of Event Scale-Revised (IES-R) from the onset of nodule discovery (6). The scale consists of two subscales: avoidance scale (actively staying away from reminders of the nodule) and intrusion scale (intrusive thoughts). The degree of vicarious trauma can be obtained by adding the avoidance scale and the intrusion scale (7,8). IES-R consisted of 16 questions, each with a score of 0–4, and an overall score of 0–64, with 0–8 being subclinical; 9–25 mild; 26–43 moderate; and over 44 severe. We defined moderate or severe nodular distress as significant (4).
Preoperative localization
However, solely relying on visual and finger exploration, endoscopic exploration of pulmonary nodules can no longer meet the surgical requirements. Ground-glass opacity (GGO) and solitary pulmonary nodule (SPN) lesions are small in size and difficult to locate intraoperatively. In particular, thoracoscopic surgery has a small incision, which can only be located by finger touch, and the positioning is more fuzzy. CT-guided medical glue injection can provide accurate reference for the location of thoracoscopic GGO and SPN, which has positive significance for shortening the operative time, controlling the resection range and reducing the difficulty of surgery. We often use n-butyl α-cyanoacrylate as a material for preoperative localization, which can help us accurately locate nodules before surgery and improve the safety and effectiveness of surgery. There are also metal spring rings or metal hooks for positioning.
Statistical analyses
Analyses were performed using SPSS 26.0 (IBM Corp., Armonk, NY, USA). A two-tailed, chi-square test was used to assess the association between patient characteristics and nodule-specific distress. The multivariable logistic regression model included variables identified as potential confounders (self-care ability, nodule nature, presence of multiple lesions, and family history of lung cancer). Adjusted odds ratios (aORs) were used as the primary measure statistical association, with P values and 95% confidence intervals (CIs) estimated using normal theory methods. Rounding was based upon significant digits rather than a fixed number of decimal places (i.e., Goldilocks method) (9).
Results
A total of 338 patients responded to the questionnaire, of whom 69% had nodules smaller than 8 mm (Table 1). There were no significant differences in basic conditions and complications between responders and non-responders. On average, participants were 59 years old [standard deviation (SD) =12 years], with 55% being female. The majority of patients were non-smokers (69%) while 68% had high levels of economic insecurity (as indicated by their inability to pay for surgery).
Table 1
| Characteristics of patients | Value (n=234) |
|---|---|
| Age (years), mean ± SD | 59±12 |
| Gender | |
| Male | 45% |
| Female | 55% |
| Highest level of education | |
| Primary and below | 57% |
| Junior high school | 23% |
| High school/technical secondary school | 10% |
| Junior college/bachelor | 10% |
| Whether patient’s own salary was enough to cover expenses | |
| Not enough | 47% |
| Enough | 32% |
| No answer | 21% |
| Spouse | |
| Yes | 95% |
| No | 5% |
| Number of children | |
| 0 | 2% |
| 1 | 27% |
| 2 | 49% |
| ≥3 | 22% |
| ADL | |
| Dependent | 17% |
| Independence | 73% |
| Current or past smoking history | |
| Smoking never quit | 17% |
| Quit smoking | 14% |
| No smoking | 69% |
| CT examination demonstrates the nature of pulmonary nodules | |
| Solid nodule | 36% |
| Part-solid nodule | 50% |
| GGN | 14% |
| Pulmonary nodule morphology | |
| Round, quasi-round | 34% |
| Having irregular, polygonal or flat, straight edges | 35% |
| Unaware of | 31% |
| Number of lesions | |
| Single lesion | 71% |
| Multifocal diseases | 29% |
| Family history of lung cancer | |
| Yes | 10% |
| No | 90% |
| Pulmonary nodule properties | |
| Benign | 19% |
| Malignant | 81% |
| Scope of resection | |
| Wedge resection | 13% |
| Segmentectomy | 75% |
| Lobectomy | 12% |
SD, standard deviation; ADL, activity of daily living; GGN, ground glass nodule.
Approximately 9% of patients had subclinical distress and anxiety (Table 1). Majority of patients (69%) reported moderate to clinically significant distress. More than 92% of participants were unable to take care of themselves in daily life (Table 2), with a corresponding aOR for clinically significant distress of 4.4 (P=0.022) (Table 3). Presence of solid nodules (P=0.015), family history of lung cancer (P=0.048), and multifocal disease (P=0.006) also were important predictive factors, with each having aORs ≥2.7.
Table 2
| Variables | Number with clinically significant distress | Positive rate (%) | P value | |
|---|---|---|---|---|
| No | Yes | |||
| Gender | 0.762 | |||
| Female | 41 | 87 | 68 | |
| Male | 32 | 74 | 70 | |
| Age | 0.138 | |||
| <60 years | 30 | 83 | 73 | |
| ≥60 years | 43 | 78 | 64 | |
| BMI | 0.900 | |||
| <24 kg/m2 | 41 | 89 | 68 | |
| ≥24 kg/m2 | 32 | 72 | 69 | |
| Education background | 0.278 | |||
| Junior high school and above | 35 | 65 | 65 | |
| Junior high school and below | 38 | 96 | 72 | |
| ADL | 0.001 | |||
| Independent | 70 | 125 | 64 | |
| Dependent | 3 | 36 | 92 | |
| Nodules nature | 0.003 | |||
| GGN | 15 | 18 | 55 | |
| Part-solid nodule | 43 | 74 | 63 | |
| Solid nodule | 15 | 69 | 82 | |
| Smoking history | 0.589 | |||
| No | 52 | 109 | 68 | |
| Yes | 21 | 52 | 71 | |
| Multifocal diseases | 0.043 | |||
| No | 58 | 107 | 65 | |
| Yes | 15 | 54 | 78 | |
| Partner | 0.634 | |||
| No | 3 | 9 | 75 | |
| Yes | 70 | 152 | 68 | |
| Family history of lung cancer | 0.011 | |||
| No | 71 | 139 | 66 | |
| Yes | 2 | 22 | 92 | |
BMI, body mass index; ADL, activity of daily living; GGN, ground glass nodule.
Table 3
| Characteristics | OR | 95% CI | P value |
|---|---|---|---|
| ADL | |||
| Yes | 1.0 | Referent | – |
| No | 4.4 | 1.2–16 | 0.022 |
| Family history of lung cancer | |||
| No | 1.0 | Referent | – |
| Yes | 4.7 | 1.02–21 | 0.048 |
| Nodules nature | |||
| GGN | 1.0 | Referent | – |
| Part-solid nodule | 1.2 | 0.52–2.7 | 0.691 |
| Solid nodule | 3.2 | 1.3–8.3 | 0.015 |
| Multifocal diseases | |||
| No | 1.0 | Referent | – |
| Yes | 2.7 | 1.3–5.4 | 0.006 |
OR, odds ratio; CI, confidence interval; ADL, activity of daily living; GGN, ground glass nodule.
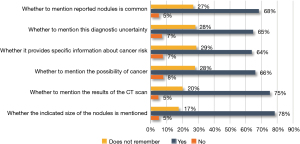
Various factors prompted patients to choose surgical excision to manage their condition. Most noteworthy was seeing the CT scan results (75%), reference to the pulmonary nodule size (78%), and number of nodules (68%) (Figure 2).
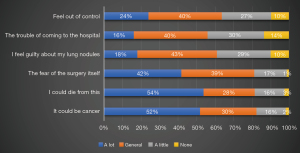
Among the concerns associated with pulmonary nodules, the risk of cancer (52%) and the fear of surgery (42%) or dying (54%) were observed to have a significant psychological impact on patients (Figure 3). Approximately 24% of patients indicated often feeling uneasy or ‘out of control’ about pulmonary nodules. Upward of 80% of patients who decided to have surgery said they clearly remembered their doctor’s clinical communication, but ~29% mentioned lacking adequate medical knowledge to understand the topic (not shown in tables).
Discussion
According to a September 2021 study from the Affiliated Hospital of Chongqing Medical University (10), patients with pulmonary nodular anxiety tend to exhibit significantly altered perfusion status in parts of their brain. As clinical anxiety can affect decision-making and quality of life, we attempted to determine the root causes of this anxiety (11,12).
After receiving the CT report, patients usually feel nervous when they see nodules in their lungs, and the first choice of many patients is to search on the Internet using a search engine (for example, Google, Bing, and Baidu). In our opinion, the Internet is also a double-edged sword. The Internet enables people to obtain all kinds of knowledge and information conveniently and quickly, but how to correctly understand and screen valuable information for their own use is also a huge challenge. Many patients through the Internet constantly search for information about the diagnosis of lung nodules, the results are often more anxious, more nervous, more afraid. From a psychological point of view, this is a typical “Barnum effect” brought by the suggestive results, that is, we usually say “right seat” (13).
Misconceptions about pulmonary nodules are common. Our finding highlights the importance of improving clinical communication with patients to correct patient misunderstandings of pulmonary nodules. For example, patients’ perceived cancer risk has been shown to be more strongly linked to pain than actual cancer (1). Many patients also equate cancer with death. What they do not know is that indolent (slow growing) tumors are unlikely to cause problems in their lifetime. Importantly, a significant number of patients do not fully understand what their doctors are trying to convey. That is, not all nodules will develop into cancer, most nodules are benign, and that patients with small nodules are suitable for conservative treatment. Again, a patient’s disproportionate fear of death and cancer suggests a lack of effective doctor-patient communication.
Our data help to quantify the impact of nodule detection on patients’ physical and mental health (11). However, the current findings differ from those of Freiman et al. (4), who showed that patients older than 65 years, current smokers, and those with a high school diploma or less were more likely to have anxiety (14).
In brief, we observed that poor performance in ADL, presence of solid and multiple pulmonary nodules, and a family history of lung cancer affected patients’ moods to varying degrees. The average age of the cases in our study was about 60 years, belonging to the older group, which has more underlying diseases than the younger age group. Patients who lacked the ability to take care of themselves showed greater anxiety after pulmonary nodules were accidentally detected (12). Due to their own serious underlying diseases, some patients need to rely on others in daily life, and these patients often have negative words and deeds. Their future is more uncertain. We should pay more attention and care to these patients, and give them hope in life again. Although most patients have little knowledge of nodules, after learning about nodules, whether from a physician, the Internet, or other sources, they will also know that the presence of solid and multiple nodules conveys a greater likelihood of malignancy. These aspects may bring more psychological pressure to patients in the face of surgery. It also is well known that lung cancer has a family history. Therefore, patients with a family history of lung cancer can experience more stress when facing pulmonary nodules especially their loved ones who died of lung cancer in front of them will bring greater pressure to themselves, and there will be more obvious clinical anxiety in the face of surgery. Medical workers should give clear guidance and comfort to such patients. Surprisingly, there was no clear correlation between smoking (vs. non-smoking) and anxiety (15).
In our experience, patients often overestimate the risk of nodules, and although patients know the cause of their distress, the uncontrollable and unknown nature of their nodules is the main cause of their anxiety (16,17). This demonstrates the importance of helping patients through the nodule monitoring period. A recent study by Slatore et al. suggested that this suffering may be alleviated with high-quality clinical communication (18). As noted in a study of communication about abnormal Papanicolaou tests (19), doctors may not mention cancer because they want to avoid arousing fears that might not be warranted, but patients tend to worry about cancer no matter the doctor mentions it or not. Therefore, doctors should explicitly discuss cancer risks unless the patient explicitly asks not to be told. The American College of Chest Physicians recommends that all patients with pulmonary nodules adopt a shared decision-making approach, which clearly explains that the treatment process helps patients to understand and reduce their feelings of anxiety. In 1986, a 9-year compulsory education requirement was implemented in China; there had been no primary education for patients above 50 years in the local area. While patients can seek advice from their children to decide whether to choose surgery, such communication often yields unexpected results.
The ability to explain the risk of pulmonary nodules to patients from a professional perspective and enlighten patients is an essential component of being a good clinician. These simple communication strategies can help to improve the lives of the large number of patients found to have pulmonary nodules each year.
Our study lacked dynamic follow-up data for patients who experienced peak pain at the onset of nodule discovery. Moreover, our catchment area was limited to Linhai City, and thus observed findings may not apply to the general Chinese population. The observational nature of our study also may have resulted in undetermined bias and reporting errors.
Conclusions
In our cohort of patients who elected to surgically remove their pulmonary nodules, our findings suggest that the ability to perform ADL (P=0.022), presence of solid (P=0.015) and multiple nodules (P=0.006), and a family history of lung cancer (P=0.048) place patients at greater risk for experiencing anxiety during their treatment decision-making process. As indicated, the detection of nodules seriously affected patients’ physical and mental health, and perioperative anxiety is very common in this patient group.
Acknowledgments
Funding: The present study was supported by
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1701/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1701/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1701/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1701/coif). S.L. received fees for consulting and training from Olympus, Fujifilm, and Ambu. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Taizhou Hospital Research Ethics Committee (No. K202107138), and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Slatore CG, Wiener RS. Pulmonary Nodules: A Small Problem for Many, Severe Distress for Some, and How to Communicate About It. Chest 2018;153:1004-15. [Crossref] [PubMed]
- Fang W, Xiang Y, Zhong C, et al. The IASLC/ATS/ERS classification of lung adenocarcinoma-a surgical point of view. J Thorac Dis 2014;6:S552-60. [Crossref] [PubMed]
- Wiener RS, Gould MK, Woloshin S, et al. What do you mean, a spot?: A qualitative analysis of patients' reactions to discussions with their physicians about pulmonary nodules. Chest 2013;143:672-7. [Crossref] [PubMed]
- Freiman MR, Clark JA, Slatore CG, et al. Patients' Knowledge, Beliefs, and Distress Associated with Detection and Evaluation of Incidental Pulmonary Nodules for Cancer: Results from a Multicenter Survey. J Thorac Oncol 2016;11:700-8. [Crossref] [PubMed]
- Slatore CG, Horeweg N, Jett JR, et al. An Official American Thoracic Society Research Statement: A Research Framework for Pulmonary Nodule Evaluation and Management. Am J Respir Crit Care Med 2015;192:500-14. [Crossref] [PubMed]
- Jeantieu M, Gaillat F, Antonini F, et al. Postoperative pain and subsequent PTSD-related symptoms in patients undergoing lung resection for suspected cancer. J Thorac Oncol 2014;9:362-9. [Crossref] [PubMed]
- Zhang Q, Wang Z, Liu Y, et al. Application of Simultaneous Localization of Multiple Pulmonary Nodules in a Hybrid Operating Room for Uniportal Video-Assisted Thoracic Surgery. Int J Gen Med 2022;15:1429-35. [Crossref] [PubMed]
- Fiscella K, Whitley E, Hendren S, et al. Patient navigation for breast and colorectal cancer treatment: a randomized trial. Cancer Epidemiol Biomarkers Prev 2012;21:1673-81. [Crossref] [PubMed]
- Sullivan DR, Golden SE, Ganzini L, et al. 'I still don't know diddly': a longitudinal qualitative study of patients' knowledge and distress while undergoing evaluation of incidental pulmonary nodules. NPJ Prim Care Respir Med 2015;25:15028. [Crossref] [PubMed]
- Wang XH, Liu XF, Ao M, et al. Cerebral Perfusion Patterns of Anxiety State in Patients With Pulmonary Nodules: A Study of Cerebral Blood Flow Based on Arterial Spin Labeling. Front Neurosci 2022;16:912665. [Crossref] [PubMed]
- Wu X, Chen T, Wang K, et al. Efficacy and safety of transcutaneous electrical acupoints stimulation for preoperative anxiety in thoracoscopic surgery: study protocol for a randomised controlled trial. BMJ Open 2023;13:e067082. [Crossref] [PubMed]
- Li L, Zhao Y, Li H. Assessment of anxiety and depression in patients with incidental pulmonary nodules and analysis of its related impact factors. Thorac Cancer 2020;11:1433-42. [Crossref] [PubMed]
- Hua J, Zhou YX. Personality assessment usage and mental health among Chinese adolescents: A sequential mediation model of the Barnum effect and ego identity. Front Psychol 2023;14:1097068. [Crossref] [PubMed]
- Boulate D, Fidelle M, Caramella C, et al. Epidemiological Study to Assess the Prevalence of Lung Cancer in patients with smoking-associated atherosclerotic cardiovascular diseases: PREVALUNG study protocol. BMJ Open 2022;12:e067191. [Crossref] [PubMed]
- Wiener RS, Gould MK, Woloshin S, et al. 'The thing is not knowing': patients' perspectives on surveillance of an indeterminate pulmonary nodule. Health Expect 2015;18:355-65. [Crossref] [PubMed]
- Dall'Era MA. Patient and disease factors affecting the choice and adherence to active surveillance. Curr Opin Urol 2015;25:272-6. [Crossref] [PubMed]
- Nebgen DR, Lu KH, Bast RC Jr. Novel Approaches to Ovarian Cancer Screening. Curr Oncol Rep 2019;21:75. [Crossref] [PubMed]
- Slatore CG, Golden SE, Ganzini L, et al. Distress and patient-centered communication among veterans with incidental (not screen-detected) pulmonary nodules. A cohort study. Ann Am Thorac Soc 2015;12:184-92. [Crossref] [PubMed]
- Wang XH, Wang T, Ao M, et al. Prevalence and characteristics of anxiety in patients with unconfirmed pulmonary nodules. Clin Respir J 2023;17:157-64. [Crossref] [PubMed]



