
Comparison of safety and anxiety/depression in computed tomography-guided hook-wire localization versus electromagnetic navigation bronchoscopy-guided localization: a retrospective cohort study
Highlight box
Key findings
• Electromagnetic navigation bronchoscopy (ENB)-guided localization has fewer complications, lower incidence of adverse events, and less impact on postoperative anxiety or depression.
What is known and what is new?
• Both ENB and computed tomography-guided localization techniques have been extensively studied for their accuracy and effectiveness in preoperative localization of small pulmonary nodules.
• This manuscript aims to compare the accuracy, safety, and effectiveness of two localization methods while further assessing postoperative lung function and the presence of anxiety and depression. By analyzing the short-term physiological and psychological effects, we aim to evaluate the impact of different localization techniques on patient outcomes.
What is the implication, and what should change now?
• Both localization methods effectively enable nodule localization, but ENB-guided localization demonstrates greater advantages in terms of patient safety and short-term psychological outcomes.
Introduction
Annually, the global incidence of lung cancer, the predominant form of malignancy, reached 2.2 million reported cases every year, resulting in a mortality rate of 1.8 million deaths, the highest among all malignant tumors (1). With the application of low-dose spiral computed tomography (CT) scanning, the early detection rate of lung cancer increased by 12%, and the mortality rate decreased by 20%, which is conducive to the early diagnosis and treatment of lung cancer (2). Recently, an increasing number of small, deep, and solitary pulmonary nodules are found, many of which have a propensity for early malignant transformation requiring surgical intervention. However, intraoperative identification of some solitary nodules is challenging because these target lesions are difficult to see or touch during the surgery. Previous studies have demonstrated that failure to visualize or palpate nodules resulted in 54% of patients requiring thoracotomy instead of video-assisted thoracoscopic surgery (VATS) for successful resections (3,4). In fact, failure to locate nodules may result in prolonged surgery or conversion to unplanned thoracotomy. Therefore, preoperative localization is very important for successful and accurate VATS resections.
Since the 1990s, CT-guided percutaneous location for small pulmonary peripheral nodules has become widespread, and lots of methods have been developed, such as hook-wires, microcoils, and dyes (5). These CT-guided locating tools show excellent detection rates, but there are many reports of major and minor complications such as pain, bleeding, pneumothorax, dislodging and migration of the marker (6). To avoid these adverse events, some bronchoscopic localization methods have become another choice. In general, bronchoscopic location has a high accuracy with no major complications in marking small pulmonary peripheral nodules (7).
Electromagnetic navigation bronchoscopy (ENB) is an emerging bronchoscopic technology which finds lung lesions with three-dimensional (3D) virtual map based on thin-section CT reconstructed images and an electromagnetic tracking system. More and more studies have demonstrated promising outcomes in terms of the accuracy and safety of ENB-guided transbronchial needle aspiration or biopsy (8). It has also been used as a preoperative localization method to target lung lesions for precise and successful VATS resection. Meanwhile, intraoperative near-infrared (NIR) imaging with indocyanine green (ICG) has emerged in thoracic surgery to achieve safe, accurate, and intuitive operations. ICG was injected under the guidance of ENB to mark the position of the target lesion (9).
Studies have reported that anxiety and depression are more prevalent in postoperative non-small cell lung cancer (NSCLC) patients than in healthy participants (10). Anxiety and depression are common psychological disorders associated with poor clinical outcomes in patients with NSCLC and are predictors of poor survival in patients with lung cancer. However, the etiology of postoperative anxiety or depression remains incompletely investigated in the existing literature (11). In a clinical context, the presence of acute pain related to hook-wire localization remains a significant concern, despite the implementation of local anesthesia (12). The protracted duration of such acute pain has the potential to contribute to the development of various mental health disorders, such as anxiety and depression (13). Currently, there is a lack of research regarding the impact of preoperative localization on postoperative anxiety and depression in patients. Therefore, to assess the effects of two different localization methods on postoperative anxiety and depression, we utilized the Hospital Anxiety and Depression Scale (HADS). HADS is a self-assessment tool designed to measure the severity of anxiety and depression in patients receiving treatment in a hospital. It includes two subscales: one for anxiety and one for depression, each consisting of 7 items. The questionnaire aims to identify and quantify symptoms of anxiety and depression, providing healthcare professionals with valuable insights into the psychological well-being of patients. HADS is frequently employed in both clinical research and practical healthcare settings to assist in the assessment and management of patients’ mental health.
In this retrospective cohort study, we designed to validate the accuracy and safety of preoperative ENB-guided localization with ICG compared with CT-guided localization with hook-wire for resection of small pulmonary peripheral solitary nodules. Furthermore, we also investigated follow-up results regarding the loss of pulmonary function and changes in anxiety and depression after resections with different location methods. The purpose is to investigate the impact of different localization methods on immediate physiological and psychological well-being postoperatively, in order to provide additional insights into the psychological well-being of postoperative patients undergoing preoperative localization of pulmonary nodules, and to offer a basis for healthcare professionals to develop more effective intervention strategies. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1351/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the institutional review board of the First Affiliated Hospital of Soochow University (ethical approval No. 2023293). This study was a retrospective, single-center pilot study on patients who received preoperative ENB-guided localization with ICG or CT-guided localization with hook-wire for VATS resections of small pulmonary solitary nodules between January 2022 and December 2022, and therefore the individual consent was waived. The inclusion criteria were: (I) patients aged older than 18 years; (II) pulmonary nodules confirmed by thin-layer high-resolution CT (HRCT) scan and requiring VATS resection after professional assessment by the multidisciplinary committee of lung neoplasms; (III) pulmonary nodules smaller than 20 mm; (IV) inability to accurately identify the location of pulmonary nodules with intraoperative observation and palpation; and (V) patients who received electromagnetic navigation combined with ICG inject or CT scan with hook-wire puncture for preoperative localization. Patient demographics, nodules CT scan characteristics (size, depth, location), localization characteristics (time, results, complications), operative characteristics (surgical moods, pathology types), postoperative complications were collected. Patients received regular follow-up by telephone or clinical visit for more than 3 months. The results of pulmonary function tests were recorded. The study adopted HADS to quantify the anxiety and depression in patients after VATS resections. Anxiety was evaluated using HADS-A and depression was assessed through HADS-D. We administer patient satisfaction surveys, including the HADS scoring scale, to the majority of patients upon admission, discharge, and during postoperative follow-ups. All surveys are conducted anonymously through online questionnaires or with the assistance of medical staff, and patient consent is obtained verbally or through self-completion of the forms.
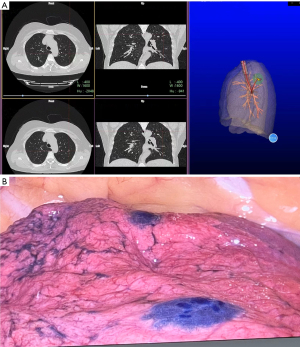
ENB-guided localization with ICG
All ENB procedures were performed in the operating room using LungCare navigation system (LungCare Medical Technologies Ltd., Inc., Suzhou, China). Chest CT scan with 1 mm cuts was performed prior to surgery and virtual 3D route to the target lesion was reconstructed through the software with chest-CT data. After general anesthesia induction using a single-lumen endotracheal tube, routine bronchoscopy was conducted and the bronchoscope was kept at the carina while locatable wire (LW) covered with guided sheath (GS) was inserted. Then the bronchoscope was advanced into the left and right main bronchus and pulled back to the trachea to complete the registration. The actual images were matched with the virtual route and the matching degree should reach more than 80%. After observing three regular respiratory cycles to reduce correction errors, the operator began to direct the bronchoscope into the target bronchus following the route through multiple planar reconstruction images. If the target lesion was reached according to the actual images and virtual route, LW was withdrawn and 2.3 mL ICG (25 mg; Dandong Yichuang Pharmaceutical Co., Ltd., China) was injected for marking. A total of 0.3 mL ICG was reached and 2.0 mL was retained in the sheath (Figure 1). In this study, if the surgeon can quickly locate and remove the nodule from the localization point during the operation, it is considered successful localization while unsuccessful localization refers to the inability to do so. ENB localization was conducted by qualified endoscopists.
CT-guided localization with hook-wire
The appropriate position was selected according to the target lesion in previous CT images, and a radiopaque grid was placed on the body surface. CT scan with 1 mm cuts was performed in the determined area. Then the puncture point was marked in the intersection of laser and radiopaque grid. After routine disinfection and local anesthesia, needle (18 G × 10 cm, BLR18/10, Gallini S.R.L., Mantova, Italy) was inserted in the chosen puncture level, angle, and depth determined by CT images. Hook-wire was released after appropriate adjustment in repeated CT scans (Figure 2). In this study, successful localization is defined as the final CT scan confirming the presence of the hook-wire within the lung, and the surgical team being able to promptly locate and remove the nodule from the designated site during the operation while unsuccessful localization refers to the inability to do so. CT-guided localization was performed by qualified thoracic surgeons.

VATS procedure
After placing double-lumen tube for general anesthesia, the patient was placed in a lateral decubitus position. A single 3-cm skin incision was made in the fourth or fifth intercostal space along the anterior axillary line. When identifying the target lesion, endostaplers were applied to complete resections. Standardized anatomical resection was performed when frozen section biopsy results reported the existence of invasive components, including segmentectomy or lobectomy with mediastinal lymph node dissection. To confirm the effective resection of the nodule in the excised specimen, tactile examination or rapid frozen section pathology is performed.
Statistical analyses
Data were analyzed using SPSS software (SPSS 25.0, Chicago, IL, USA). Enumeration data were presented as percentages and analyzed by χ2 test, and measurement data were presented as mean ± standard deviation (SD) and analyzed by t-test. A P value ≤0.05 was considered statistically significant.
Results
Characteristics of the patients
We included a total of 177 patients (65 males and 112 females) who underwent single-port VATS to remove nodules after localization. The nodules were localized by ENB in 57 patients and by CT guidance in 120 patients. Clinical characteristics of the patients and lung nodules are listed in Table 1. There were no significant differences in the average size and depth of the nodules localized by the two positioning methods. These nodules were distributed in each lobe of the lung, including 47 nodules in the left upper lobe, 43 nodules in the left lower lobe, 42 nodules in the right upper lobe, 4 nodules in the right middle lobe, and 41 nodules in the right lower lobe. The pathology diagnoses of 177 nodules were as follows: 31 cases of benign nodules, 15 cases of atypical adenomatous hyperplasia (AHH), 100 cases of adenocarcinoma in situ (AIS), 14 cases of microinvasive adenocarcinoma (MIA) and 17 cases of invasive adenocarcinoma (IAC). Standard lobectomy was performed in 9 patients with IAC. Postoperative complications occurred in 10 patients, including 9 patients with postoperative air leakage (≥3 days) and 1 patient with postoperative pleural effusion (≥3 days). There were no significant differences in the average length of hospital stay between the two groups. All nodules were confirmed to be effectively removed through tactile examination and rapid frozen section pathology in the resected specimens.
Table 1
| Variables | ENB localization | CT-guided hook-wire localization | P value |
|---|---|---|---|
| Total | 57 | 120 | |
| Age (years) | 50.3±11.9 | 49.8±13.4 | 0.799 |
| Gender | 0.617 | ||
| Male | 19 [33] | 46 [38] | |
| Female | 38 [67] | 74 [62] | |
| Nodule size (mm) | 9.0±2.8 | 8.3±3.0 | 0.104 |
| Nodule depth (mm) | 10.3±7.5 | 9.4±8.2 | 0.503 |
| Location | |||
| LUL | 13 [23] | 34 [28] | |
| LLL | 11 [19] | 32 [27] | |
| RUL | 20 [35] | 22 [18] | |
| RML | 3 [5] | 1 [1] | |
| RLL | 10 [18] | 31 [26] | |
| Air bronchus sign | 36 [63] | 59 [49] | – |
| Surgical mode | 0.941 | ||
| Lobectomy | 3 [5] | 6 [5] | |
| Sublobar resection | 54 [95] | 114 [95] | |
| Postoperative complication | 0.878 | ||
| No | 54 [95] | 113 [94] | |
| Yes | 3 [5] | 7 [6] | |
| Prolonged air leak (≥3 days) | 3 | 6 | |
| Pleural effusion (≥3 days) | 0 | 1 | |
| Length of hospitalization (days) | 2.7±1.3 | 2.4±0.9 | 0.097 |
| Pathology | – | ||
| AAH | 3 [5] | 12 [10] | |
| AIS | 34 [60] | 66 [55] | |
| MIA | 4 [7] | 10 [8] | |
| IAC | 6 [11] | 11 [9] | |
| Benign | 10 [18] | 21 [18] |
Data are presented as n, mean ± SD, or n [%]. ENB, electromagnetic navigation bronchoscopy; CT, computed tomography; LUL, left upper lobe; LLL, left lower lobe; RUL, right upper lobe; RML, right middle lobe; RLL, right lower lobe; AAH, adenomatous hyperplasia; AIS, adenocarcinoma in situ; MIA, microinvasive adenocarcinoma; IAC, invasive adenocarcinoma; SD, standard deviation.
Localization of the nodules
The mean calibration time and navigation time of ENB-guided localization, respectively, were 1.59±1.44 and 12.2±10.8 minutes. There were no significant differences in the operative time between the two groups of localization methods. Of the patients who received ENB-guided localization, 5 failed due to failure to reach the specified location. In the CT-guided localization group, six instances of failure occurred as a result of needle hook location deviation. There were no significant complications in ENB-guided localization group (0/57). Compared with ENB-guided localization group, CT-guided hook-wire localization group had more complications (61/120, P<0.001). The incidence of pneumothorax was 33.3% (40/120), Pulmonary hemorrhage was 10% (12/120), hemopneumothorax was 2.5% (3/120), and hook-wire migration was 5% (6/120). There were no death or severe complications such as tension pneumothorax and massive hemoptysis (Table 2).
Table 2
| Variables | ENB localization | CT-guided hook-wire localization | P value |
|---|---|---|---|
| Calibration time (min) | 1.59±1.44 | 0 | <0.001 |
| Navigation time (min) | 12.2±10.8 | 0 | <0.001 |
| Localization time (min) | 17.3±11.9 | 15.1±7.3 | 0.146 |
| Needle-carrying time (min) | 0 | 25.1±7.3 | <0.001 |
| Localization result | 0.335 | ||
| Satisfied | 52 | 114 | |
| Failed | 5 | 6 | |
| Localization complication | <0.001 | ||
| Yes | 0 | 61 | |
| Pneumothorax | 0 | 40 | |
| Pulmonary hemorrhage | 0 | 12 | |
| Hemopneumothorax | 0 | 3 | |
| Hook-wire migration | 0 | 6 | |
| No | 57 | 59 |
Data are presented as mean ± SD or n. ENB, electromagnetic navigation bronchoscopy; CT, computed tomography; SD, standard deviation.
Postoperative short-term pulmonary function effects
The impact of different localization methods on the extent of lung resection and its effect on postoperative outcomes in patients remains uncertain. Therefore, we collected pre- and post-operative pulmonary function data for comparative analysis. The average forced expiratory volume in 1 second (FEV1) values from preoperative pulmonary function tests did not show significant differences between the ENB localization group and the CT-guided hook-wire localization group. At the 3-month post-surgery, the ENB-guided localization group exhibited a mean FEV1 value of 1.77±0.34 L, while the CT-guided hook-wire localization group had a mean FEV1 value of 1.89±0.43 L (P=0.063). There were no significant differences in the FEV1 loss between the two groups. Similarly, there were no significant differences in the average forced vital capacity (FVC) values from preoperative pulmonary function tests between the ENB localization group and the CT-guided hook-wire localization group. After a postoperative period of 3 months, there was no significant difference observed in the average FVC values and FVC loss rates between the two groups. These findings suggest that the impact of different localization methods on the extent of lung resection may be similar (Table 3).
Table 3
| Pulmonary function | ENB localization | CT-guided hook-wire localization | P value |
|---|---|---|---|
| FEV1 (L) | |||
| Baseline | 2.03±0.39 | 2.17±0.49 | 0.051 |
| T3 | 1.77±0.34 | 1.89±0.43 | 0.063 |
| FEV1 loss (%) | 12.70±2.21 | 13.00±2.12 | 0.397 |
| FVC (L) | |||
| Baseline | 2.60±0.40 | 2.62±0.43 | 0.782 |
| T3 | 2.42±0.39 | 2.45±0.41 | 0.676 |
| FVC loss (%) | 6.81±2.40 | 6.38±3.01 | 0.346 |
Data are presented as mean ± SD. Baseline: preoperative; T3: 3 months after surgery. ENB, electromagnetic navigation bronchoscopy; CT, computed tomography; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; SD, standard deviation.
The influence of localization on anxiety and depression
The baseline mean anxiety scores for the ENB-guided localization group and CT-guided hook-wire localization group were 2.54±0.76 and 2.48±0.89, respectively. No significant differences were found between the two groups (P=0.658). Anxiety scores increased in both groups on the first day after surgery. The mean anxiety score for the CT-guided hook-wire localization group was significantly higher than that of the ENB-guided localization group (P<0.001). At the 2-week postoperative, both groups exhibited a decrease in anxiety scores compared to the initial day following surgery. However, the mean anxiety score of the ENB-guided localization group remained significantly different from that of the CT-guided localization group (P=0.003). As time progressed, at the 3-month postoperative, anxiety levels decreased in both groups, no statistical difference was observed between the two groups (P=0.706). The mean depression scores at baseline were 2.25±0.74 and 2.48±0.82 in the ENB-guided localization group and CT-guided hook-wire localization group, respectively. No significant intergroup differences were observed (P=0.065). Similar to anxiety scores, depression scores exhibited an increase in both groups on the initial day following surgery. Specifically, the mean depression score in the CT-guided localization group was, significantly surpassing that of the ENB-guided localization group (P<0.001). Notably, disparities between the two groups persisted even during the second week after surgery (P<0.001). Over the course of the third month, the mean depression scores in both groups exhibited a gradual decline, commencing from the first day of surgery and continuing until the conclusion of the third month (Table 4).
Table 4
| HADS | ENB localization | CT-guided hook-wire localization | P value |
|---|---|---|---|
| Anxiety | |||
| Baseline | 2.54±0.76 | 2.48±0.89 | 0.658 |
| T1 | 4.89±1.28 | 8.71±0.98 | <0.001 |
| T2 | 4.02±0.81 | 4.48±1.00 | 0.003 |
| T3 | 2.39±0.49 | 2.42±0.51 | 0.706 |
| Depression | |||
| Baseline | 2.25±0.74 | 2.48±0.82 | 0.065 |
| T1 | 4.82±0.95 | 7.27±1.12 | <0.001 |
| T2 | 3.53±0.60 | 4.58±0.82 | <0.001 |
| T3 | 2.33±0.93 | 2.51±0.87 | 0.223 |
Data are presented as mean ± SD. Baseline: preoperative; T1: the day after surgery; T2: 2 weeks after surgery; T3: 3 months after surgery. HADS, Hospital Anxiety and Depression Scale; ENB, electromagnetic navigation bronchoscopy; CT, computed tomography; SD, standard deviation.
Discussion
With the popularity of HRCT, more and more pulmonary nodules are being discovered (14,15). VATS is widely used in the surgical treatment of lung diseases because of its advantages of small incision, beautiful appearance and quick postoperative recover (16). Because it is difficult to identify ground-glass or solid nodules in the subpleura during VATS, it is difficult for the operator to directly touch the lung parenchyma. When it is difficult to determine whether the nodule is completely removed, the surgeon may remove more lung or switch to thoracotomy to achieve complete removal of the nodule. Therefore, accurate preoperative localization is essential for the successful removal of nodules during thoracoscopic surgery (17). CT-guided localization is the most widely used method for marking pulmonary nodules for resection. This method requires transdermal placement of hook-wires, microcoils, or staining of nodules (18,19). However, CT-guided percutaneous localization is an invasive procedure performed externally to the body surface, resulting in inevitable complications such as pain, pneumothorax, hemothorax, pulmonary hemorrhage, pleural reaction, and potentially air embolism (6,19,20). Additionally, patients are subjected to repeated exposure to radiation. The ongoing advancements in ENB-guided technology have significantly expanded its potential for utilization in preoperative puncture localization within the field of thoracic surgery. This study retrospectively evaluated and compared the safety, efficacy, and postoperative anxiety and depression status of CT-guided hook-wire localization and ENB-guided localization in patients with solitary pulmonary nodules. Our findings indicate that the two localization methods exhibit differences in terms of localization complications, short-term postoperative anxiety, and depression status, while demonstrating no significant differences in terms of procedural success rate, efficacy, and short-term postoperative physiological recovery. These observations may contribute to providing references for individualized treatment strategies in clinical practice.
At present, CT-guided hook-wire localization is widely used in clinical practice because of its simplicity, feasibility, and low cost. However, it faces high complications, additional radiation, damage to adjacent organs or tissues, transport time, and inevitable pain. Patients with CT-guided hook-wire localization need to be transported from the CT room to the operating room after puncture, which may increase the risk of localization. It has been reported that ENB-guided localization can have a lower incidence of complications during preoperative puncture localization (21,22). Because the ENB-guided localization is performed in the operating room, it can realize the rapid conversion from localization to surgery and has better operability. In our study, the success rates of both ENB-guided and CT-guided localizations were found to be satisfactory. However, it should be noted that the presence of a poor breath-holding effect during preoperative CT imaging in certain patients may result in errors in preoperative 3D reconstruction, consequently leading to unsuccessful ENB-guided localization. CT-guided localization failure may occur due to occlusion of the scapula and ribs or hook-wire migration due to activities during transport. In this study, 57 patients in the ENB-guided localization group had no complications, while 61 of the 120 patients in CT-guided hook-wire localization group had various degrees of complications. The most common complications were pneumothorax, including asymptomatic pneumothorax with lung volume compression less than 10%, followed by intrapulmonary hemorrhage, deviation of the puncture hook position and hemopneumothorax. There were no severe complications that affected the patient’s safety and surgical prognosis. In this study, the incidence of localization complications under CT guidance was higher than that reported in other centers, potentially attributable to variations in clinical practices (23). However, these findings further underscore the superior safety profile of ENB-guided localization compared to CT-guided localization. Although, our study did not show a clear difference between the time of ENB-guided localization and CT-guided localization like studies from other institutions (23). It is reasonable to believe that ENB-guided localization may bring less risk of puncture because of the lower incidence of complications and the avoidance of transit time after puncture.
The clinical data obtained from our institution substantiate the absence of substantial disparities between the two groups in terms of the occurrence of postoperative complications, duration of hospitalization, and postoperative pulmonary function test (at the 3-month mark). These findings imply that the two localization methods yield comparable impacts on postoperative physiological function and recuperation. Based on the clinical observations conducted at our institution, it has been observed that CT-guided hook-wire localization of small pulmonary nodules can elicit intense pain or discomfort in certain patients, particularly due to the insertion of a rigid wire through the chest wall and exacerbated during transportation. Furthermore, a minority of patients may experience an inability to assume a supine position due to the severe pain induced by transportation or alterations in body positioning. A retrospective study of 57 patients reported a 7% incidence of pain after CT-guided localization (24). Qin et al. found that moderate to severe pain after hook-wire localization during deep breathing or movement occurred in 50.8% and 45.7% of patients respectively (25). ENB-guided localization is done under general anesthesia and has great advantages in terms of operating comfort. For many patients, pain is a problem that cannot be ignored during percutaneous localization. Studies have reported that anxiety and depression are more prevalent in postoperative NSCLC patients than in healthy participants (10). Depression and anxiety are associated with pain severity (13). In this study, the HADS was employed to assess the levels of perioperative and postoperative anxiety and depression among patients. The findings indicate that the HADS-A/HADS-D scores of the CT-guided hook-wire localization group were higher than those of the ENB-guided localization group on the initial postoperative day. This observation suggests that the transient pain associated with CT-guided localization may serve as a significant contributing factor to postoperative anxiety and depression. During the initial postoperative review at 2 weeks, patients in the CT-guided hook-wire localization group exhibited a decrease in anxiety and depression scores. However, these scores remained higher compared to the ENB-guided localization group. Subsequently, the results of the second follow-up at 3 months indicated that the HADS-A/HADS-D scores of the CT-guided localization group had decreased from their initial levels at 2 weeks. Furthermore, no significant difference was observed between the CT-guided localization group and the ENB-guided localization group. This outcome may be attributed to the gradual alleviation of acute pain and the progressive restoration of patients’ physiological function. The HADS scores exhibited a higher magnitude compared to the preoperative scores in both groups, potentially attributable to various factors including surgical pain, discomfort arising from the presence of postoperative drainage tubes, and the occurrence of complications. This study highlighted the potential influence of CT-guided localization on short-term (within a 2-week period) postoperative anxiety and depression. Although the participants in the study did not display any clinically significant anxiety or depression-related behavior, it was noted that patients in the CT-guided localization group exhibited higher scores on the HADS compared to those in the ENB-guided localization group at both 1 day and 2 weeks after surgery. The findings indicated that the temporary elevation of HADS score subsequent to CT-guided hook-wire localization implies a potential correlation between the distress caused by percutaneous lung puncture and the subsequent development of anxiety or depression in patients. The potential psychological impact resulting from the puncture procedure should not be disregarded, and the evaluation of its potential risk factors assumes crucial significance in aiding surgeons to optimize patient management.
The majority of prior research has primarily examined the effectiveness and safety of CT-guided localization compared to ENB-guided localization (23,26). Nevertheless, the correlation between pain and postoperative anxiety or depression remains inadequately explored. Our study not only scrutinized the impact and safety of CT-guided and ENB-guided localization, but also extended the understanding of the prognosis associated with these two localization methods by evaluating perioperative complications and postoperative pulmonary function. Simultaneously, the HADS scores revealed that the cohort undergoing CT-guided localization exhibited a potential vulnerability to anxiety and depression in contrast to the cohort undergoing ENB-guided localization. This enables us to comprehensively investigate the effects of the two localization methods on the physiological and psychological aspects of patients from various angles. It has been reported that bronchoscopic labeling is superior to other techniques in patients with multiple nodules because it is less invasive and saves time (27). The promotion of hybrid operating rooms also presents potential for improved application prospects of ENB-guided localization. During clinical practice, certain patients may favor this method of preoperative localization due to its reduced pain, invasiveness, and enhanced comfort. However, it is important to note that this localization technique necessitates a longer learning curve, skilled endoscopists for its execution, and incurs higher costs. Consequently, we assert that both localization methods possess their own set of advantages and disadvantages.
Our study has several limitations: (I) this study was a retrospective single-center study and the results may have been affected by selection bias; (II) the incidence of CT-guided localization complications in this study was higher than that in other centers, which may be caused by differences in clinical operation, and more sample size is still needed to support the findings; (III) longitudinal changes in anxiety and depression in postoperative patients were not assessed; (IV) the HADS score is a self-evaluation questionnaire, and there may be assessment bias; (V) our study represents the clinical experience of a single center, and further prospective studies with a large sample size are needed to verify our clinical conclusions; and (VI) the different anesthesia methods used in the two positioning procedures may introduce bias in the assessment of postoperative anxiety and depression. However, the CT-guided localization method and ENB localization method described in this study are widely implemented in the majority of hospitals worldwide, while the implementation of CT-guided localization under general anesthesia remains challenging. Although comparative studies under these conditions may have inherent biases, they can still contribute to clinical decision-making and maintain consistency with clinical practice.
Conclusions
ENB-guided localization and CT-guided hook-wire localization can effectively identify solitary pulmonary nodules. ENB localization has fewer complications, lower incidence of adverse events. The HADS score suggested that the ENB-guided localization group had less effect on postoperative anxiety or depression than the CT-guided localization group, suggesting that this is a promising, safe, and feasible method for isolated pulmonary nodule removal of VATS that is more acceptable to patients.
Acknowledgments
Funding: This study was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1351/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1351/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1351/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1351/coif). T.X. reports funding from the 2023 Postgraduate Research & Practice Innovation Program of Jiangsu Province (No. SJCX23_1670). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the institutional review board of the First Affiliated Hospital of Soochow University (ethical approval No. 2023293) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- Lancaster HL, Heuvelmans MA, Oudkerk M. Low-dose computed tomography lung cancer screening: Clinical evidence and implementation research. J Intern Med 2022;292:68-80. [Crossref] [PubMed]
- Finley RJ, Mayo JR, Grant K, et al. Preoperative computed tomography-guided microcoil localization of small peripheral pulmonary nodules: a prospective randomized controlled trial. J Thorac Cardiovasc Surg 2015;149:26-31. [Crossref] [PubMed]
- Suzuki K, Nagai K, Yoshida J, et al. Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest 1999;115:563-8. [Crossref] [PubMed]
- Cornella KN, Repper DC, Palafox BA, et al. A Surgeon's Guide for Various Lung Nodule Localization Techniques and the Newest Technologies. Innovations (Phila) 2021;16:26-33. [Crossref] [PubMed]
- Park CH, Han K, Hur J, et al. Comparative Effectiveness and Safety of Preoperative Lung Localization for Pulmonary Nodules: A Systematic Review and Meta-analysis. Chest 2017;151:316-28. [Crossref] [PubMed]
- Liu B, Gu C. Expert consensus workshop report: Guidelines for preoperative assisted localization of small pulmonary nodules. J Cancer Res Ther 2020;16:967-73. [Crossref] [PubMed]
- Folch EE, Bowling MR, Pritchett MA, et al. NAVIGATE 24-Month Results: Electromagnetic Navigation Bronchoscopy for Pulmonary Lesions at 37 Centers in Europe and the United States. J Thorac Oncol 2022;17:519-31. [Crossref] [PubMed]
- Cui F, Liu J, Du M, et al. Expert consensus on indocyanine green fluorescence imaging for thoracoscopic lung resection (The Version 2022). Transl Lung Cancer Res 2022;11:2318-31. [Crossref] [PubMed]
- Huang X, Zhang TZ, Li GH, et al. Prevalence and correlation of anxiety and depression on the prognosis of postoperative non-small-cell lung cancer patients in North China. Medicine (Baltimore) 2020;99:e19087. [Crossref] [PubMed]
- Deng L, Chen B. Two-scale assessment of anxiety and depression in postoperative non-small cell lung cancer patients: their prevalence, risk factors, and prognostic potency. Ir J Med Sci 2023;192:2613-9. [Crossref] [PubMed]
- Kong L, Gao L, Zhang H, et al. Does Preoperative Hookwire Localization Influence Postoperative Acute and Chronic Pain After Video-Assisted Thoracoscopic Surgery: A Prospective Cohort Study. J Pain Res 2023;16:21-32. [Crossref] [PubMed]
- Michaelides A, Zis P. Depression, anxiety and acute pain: links and management challenges. Postgrad Med 2019;131:438-44. [Crossref] [PubMed]
- Weinstock T, Kidambi P, Channick CL, et al. Implementation of Lung Cancer Screening Programs with Low-Dose Computed Tomography in Clinical Practice. Ann Am Thorac Soc 2016;13:425-7. [Crossref] [PubMed]
- Walter JE, Heuvelmans MA, Bock GH, et al. Characteristics of new solid nodules detected in incidence screening rounds of low-dose CT lung cancer screening: the NELSON study. Thorax 2018;73:741-7. [Crossref] [PubMed]
- Bertolaccini L, Fornaro G, Ciani O, et al. The Impact of Surgical Experience in VATS Lobectomy on Conversion and Patient Quality of Life: Results from a Comprehensive National Video-Assisted Thoracic Surgical Database. Cancers (Basel) 2023;15:410. [Crossref] [PubMed]
- Xin N, Wu X, Chen Z, et al. A new preoperative localization of pulmonary nodules guided by mixed reality: a pilot study of an animal model. Transl Lung Cancer Res 2023;12:150-7. [Crossref] [PubMed]
- Hu L, Gao J, Chen C, et al. Comparison between the application of microcoil and hookwire for localizing pulmonary nodules. Eur Radiol 2019;29:4036-43. [Crossref] [PubMed]
- Martínez Criado Y, Pérez Bertólez S, Cabello Laureano R, et al. CT-guided methylene blue labelling to locate a pulmonary nodule before thoracoscopic resection. Cir Esp 2014;92:139-41. [Crossref] [PubMed]
- Klinkenberg TJ, Dinjens L, Wolf RFE, et al. CT-guided percutaneous hookwire localization increases the efficacy and safety of VATS for pulmonary nodules. J Surg Oncol 2017;115:898-904. [Crossref] [PubMed]
- Zhang J, He J, Chen J, et al. Application of indocyanine green injection guided by electromagnetic navigation bronchoscopy in localization of pulmonary nodules. Transl Lung Cancer Res 2021;10:4414-22. [Crossref] [PubMed]
- Mariolo AV, Vieira T, Stern JB, et al. Electromagnetic navigation bronchoscopy localization of lung nodules for thoracoscopic resection. J Thorac Dis 2021;13:4371-7. [Crossref] [PubMed]
- Tian Y, Wang C, Yue W, et al. Comparison of computed tomographic imaging-guided hook wire localization and electromagnetic navigation bronchoscope localization in the resection of pulmonary nodules: a retrospective cohort study. Sci Rep 2020;10:21459. [Crossref] [PubMed]
- Yoshida Y, Inoh S, Murakawa T, et al. Preoperative localization of small peripheral pulmonary nodules by percutaneous marking under computed tomography guidance. Interact Cardiovasc Thorac Surg 2011;13:25-8. [Crossref] [PubMed]
- Qin W, Ge J, Gong Z, et al. The incidence and risk factors of acute pain after preoperative needle localization of pulmonary nodules: a cross-sectional study. Transl Lung Cancer Res 2022;11:1667-77. [Crossref] [PubMed]
- Yang YL, Li ZZ, Huang WC, et al. Electromagnetic navigation bronchoscopic localization versus percutaneous CT-guided localization for thoracoscopic resection of small pulmonary nodules. Thorac Cancer 2021;12:468-74. [Crossref] [PubMed]
- Anayama T, Hirohashi K, Miyazaki R, et al. Near-infrared dye marking for thoracoscopic resection of small-sized pulmonary nodules: comparison of percutaneous and bronchoscopic injection techniques. J Cardiothorac Surg 2018;13:5. [Crossref] [PubMed]


