Trends and current status of general thoracic surgery in Japan revealed by review of nationwide databases
Introduction
Large scale data from thousands of cases are required to precisely evaluate medical treatments and compare outcomes among different modalities. In the field of thoracic malignancy, the tumor, node, and metastasis (TNM) staging system proposed by the Union for International Cancer Control (UICC) is based on analyses of global databases, while clinical studies using national or international databases are also now common. In Japan, several nationwide general thoracic surgery databases have been established. In the present study, the current status of nationwide databases of Japanese cases is reviewed.
Japanese associations that maintain nationwide databases of thoracic disease and their relationships
Several academic societies in Japan are focusing on thoracic diseases, including the development of nationwide databases executed by each society or in collaboration with several others. The features of these associations and databases are summarized in Table 1. Japanese Association of Thoracic Surgery (JATS) is the leading society for cardiovascular and general thoracic surgery in Japan and approximately 40% of its members are primarily involved in general thoracic surgery. The JACS is an organization of general thoracic surgeons and the representative society for lung, mediastinum, pleura, and diaphragm surgery. Most of their members also belong to JATS.
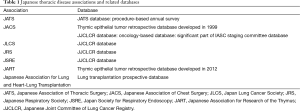
Full table
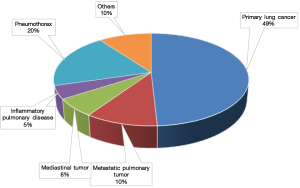
JATS maintains its own database, while JATS and JACS collaboratively administer the Japanese Board of General Thoracic Surgeons, which enables JATS to review all thoracic operations performed throughout Japan. JATS has conducted an academic survey to determine the numbers of surgical procedures and operative mortality since 1986 (1), which shows that the total number of general thoracic surgery cases in 1986 was 15,544 and steadily increased to reach 75,306 in 2013, a 4.8-fold increase during that 28-year period. The proportion of diseases treated in 2013 is shown in Figure 1.
The Japan Lung Cancer Society (JLCS), Japanese Respiratory Society (JRS), and Japan Society for Respiratory Endoscopy (JSRE) consist of clinicians of all specialties related to thoracic disease. JACS, JLCS, JRS, and JSRE established the Japanese Joint Committee of Lung Cancer Registry (JJCLCR), which manages the Japanese Lung Cancer Registry, a nationwide database. JJCLCR has conducted five nationwide database projects since 1994, most of which are retrospective collections of surgically treated cases, as shown in Table 2, with data from a total of 50,949 patients stored there. In addition, the JJCLCR database includes information showing detailed long-term outcome results for each patient, which enables oncological analysis of treatments performed for lung cancer.
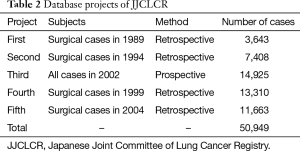
Full table
JACS and the Japanese Association for Research of the Thymus (JART) have established retrospective databases of cases of thymic epithelial tumors. Furthermore, the Japanese Association for Lung and Heart-Lung Transplantation is also keeping a registry of clinical data of all patients who undergo lung transplantation or heart-lung transplantation in Japan.
Current status of surgery for lung cancer
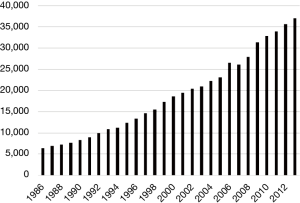
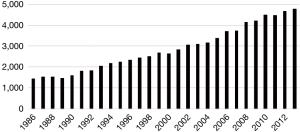
According to the JATS database, lung cancer surgery occupies 49.1% of surgical procedures and is the most common target of general thoracic surgery in Japan. The annual trend for number of patients receiving surgery for primary lung cancer is shown in Figure 2. The number of operations increased from 6,421 in 1986 to 37,008 in 2013, a 5.76-fold increase during those 28 years.
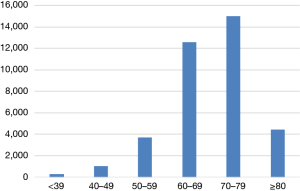
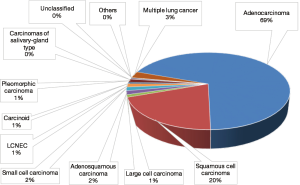
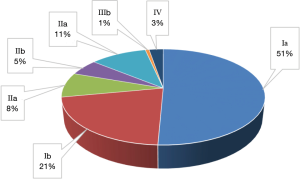
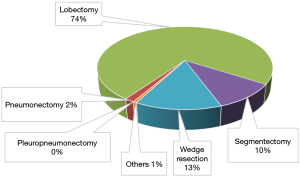
The most recent JATS survey of the characteristics of lung cancer surgery was conducted in 2013 (1) and age distribution shown by those findings is presented in Figure 3. The most prevalent age group was 70 to 79 years and patients at least 70 years old occupied 52.2% of the entire population. Pathological types are shown in Figure 4, with adenocarcinoma by far the most common histology occupying nearly 70%, followed by squamous cell carcinoma. Each of the other histological types encompasses less than 2% of all cases. Pathological stages are shown in Figure 5 and the operative procedures employed are noted in Figure 6. The 30-day mortality rates according to operative procedure are presented in Table 3.
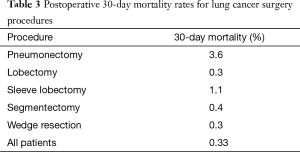
Full table
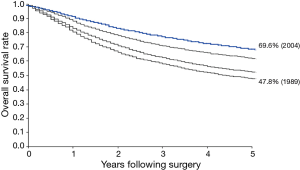
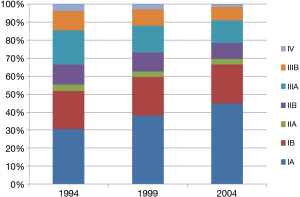
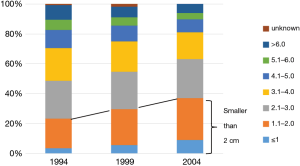
Long-term outcomes of lung cancer surgery can be obtained by analysis of the JJCLCR database (2). Overall survival rates of lung cancer patients who underwent surgical treatment in 1989, 1994, 1999, and 2004 are shown in Figure 7. The 5-year overall survival rate of the entire patient population in 2004 was 69.6%, which improved from 47.8% over the previous 15 years. Trends for pathological stage and tumor size are shown in Figures 8 and 9, respectively. The proportions of early stage disease and small tumors are growing, resulting in a recent increase in limited resection cases.
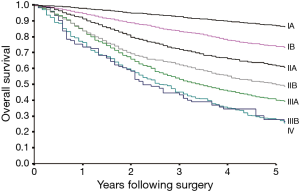
Overall survival rates in association with pathological stage in patients who underwent surgery in 2004 are shown in Figure 10. Also, the 5-year survival and rates of recurrence for each pathological stage are shown in Table 4. Tumor relapse was observed in 19.8% of all patients. The 5-year survival rate was as high as 86.8% in stage IA patients, though 12.3% of those experienced tumor recurrence. In patients with stage IIB or greater disease, the rate of relapse was more than 50%.
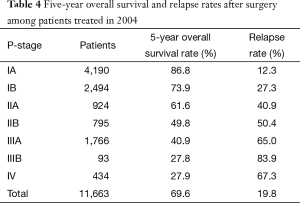
Full table
The JJCLCR databases were submitted to the staging committee of the International Association for Study of Lung Cancer (IASLC) and detailed data from 47,306 patients were utilized to propose version 8 of the UICC TNM classification in 2015 (3). Also, a project to build a retrospective database of patients surgically treated in 2010 is currently undergoing and the outcomes of surgical treatments in more recent cases will be revealed in 2017. In addition, a prospective database project of non-surgically treated patients in Japan is also being developed. Patients with a diagnosis of unresectable primary lung cancer were enrolled in 2012 and final outcomes are currently being analyzed. This project is expected to elucidate the effectiveness of novel molecular target therapies introduced since 2000.
Clinical study of lung cancer using nationwide databases
Clinical studies using JJCLCR databases are presently being performed. Based on results of analyses of 11,663 patients who underwent surgery in 2004, we reported outcomes of those with both clinical N2 and pathological N2 disease (4), the oncological significance of visceral pleural invasion (5), survival of patients with pathological T3 according to the invaded organ (6), survival of patients with pathological T4 according to the invaded organ (7), survival according to adenocarcinoma subtype (8), outcomes of patients younger than 50 years in comparison with older patients (9), outcome of surgical treatment for small cell lung cancer (10), the significance of intraoperative pleural lavage cytology findings (11), and outcome of surgical treatment in cases with pleural dissemination and malignant pleural effusion (12).
Databases of thymic epithelial tumors and clinical study
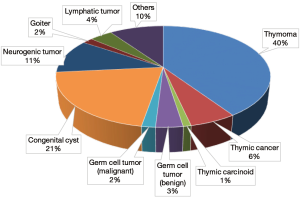
According to the JATS database, the entire number of mediastinal tumors surgically treated throughout Japan in 2013 was 4,780 (1) and the proportions of tumors in those cases is shown in Figure 11. Thymoma was most commonly encountered among surgically treated mediastinal tumors and the annual trend for number of thymic epithelial tumors is shown in Figure 12.
The first retrospective database of thymic epithelial tumors in Japan was developed by JACS in 2000 (13,14), for which clinical data of 1,320 patients with thymic epithelial tumors treated between 1990 and 1994 were collected. At that time, it was the largest scale study in the world and provided important findings. For example, debulking surgery was revealed to contribute to longer survival in invasive thymoma, but not thymic carcinoma cases. Furthermore, details regarding lymphogenous metastasis of thymic epithelial tumors was first revealed.
A second database project was initiated by JART in 2012, which is a retrospective collection of thymic epithelial tumor cases surgically treated during the 20-year period between 1991 and 2010. This JART database has been submitted to the IASLC staging committee as part of the global project for proposal of TNM classification of thymic epithelial tumors (15-17).
Recently, several novel findings related to these rare tumors have been reported following analysis of the JART databases. The members of JART reported the prognostic significance of the number of pleural dissemination lesions in Masaoka stage IVA thymoma cases (18), implications of post-operative radiation therapy (PORT) for thymoma and thymic carcinoma in patients with Masaoka stage III disease (19), the significance of an extended thymectomy for Masaoka stage I thymoma as compared to a simple thymectomy (20), the outcomes of surgery for stage III thymoma and prognostic significance of chest wall invasion (21), outcomes of surgical treatment for recurrent tumors (22), outcomes of surgery for thymic carcinoma (23), and the characteristics of myasthenia gravis associated with a thymic epithelial tumor (24).
China and South Korea have also established new associations with specific focus on thymic tumors and started their own database projects. Databases generated in East Asian countries have greatly contributed to the proposal for TNM classification of thymic epithelial tumors (15).
Lung transplantation in Japan
The Japanese Association for Lung and Heart-Lung Transplantation has developed a prospective nationwide database of lung transplantation in Japan, which contains clinical data collected from 466 patients who received lung transplantation or heart-lung transplantation from 1998 to 2015. Of those, lung transplantations from brain-dead and living related donors were performed in 283 and 181 cases, respectively. The operative procedure in brain-dead donor lung transplantation was single lung transplantation in 150 and bilateral double lung transplantation in 133 patients. Furthermore, heart-lung transplantation was performed in two patients. The 5-year overall survival rate in brain-dead donor single lung transplantation cases was 70.2%, while that in brain-dead double lung transplantation was 75.1% and in living related donor lung transplantation was 71.7%.
Concluding remarks
Nationwide databases in Japan are contributing to elucidation of trends and current status of general thoracic surgery cases. Detailed information obtained from a large-scale database is helpful for evaluation of treatment strategies, especially in cases of rare disease. In addition, international collaborative studies can be promoted by development of global database projects. Thus, additional nationwide as well as global large-scale database studies are expected, which will contribute to further improvements in clinical medicine.
Acknowledgements
The author appreciates all the Japanese institutes for sincere cooperation in nation-wide database projects.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Committee for Scientific Affairs, The Japanese Association for Thoracic Surgery, Masuda M, et al. Thoracic and cardiovascular surgery in Japan during 2013: Annual report by The Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 2015;63:670-701. [Crossref] [PubMed]
- Sawabata N, Miyaoka E, Asamura H, et al. Japanese lung cancer registry study of 11,663 surgical cases in 2004: demographic and prognosis changes over decade. J Thorac Oncol 2011;6:1229-35. [Crossref] [PubMed]
- Rami-Porta R, Bolejack V, Giroux DJ, et al. The IASLC lung cancer staging project: the new database to inform the eighth edition of the TNM classification of lung cancer. J Thorac Oncol 2014;9:1618-24.
- Yoshino I, Yoshida S, Miyaoka E, et al. Surgical outcome of stage IIIA- cN2/pN2 non-small-cell lung cancer patients in Japanese lung cancer registry study in 2004. J Thorac Oncol 2012;7:850-5. [Crossref] [PubMed]
- Kawase A, Yoshida J, Miyaoka E, et al. Visceral pleural invasion classification in non-small-cell lung cancer in the 7th edition of the tumor, node, metastasis classification for lung cancer: validation analysis based on a large-scale nationwide database. J Thorac Oncol 2013;8:606-11.
- Kawaguchi K, Miyaoka E, Asamura H, et al. Modern surgical results of lung cancer involving neighboring structures: a retrospective analysis of 531 pT3 cases in a Japanese Lung Cancer Registry Study. J Thorac Cardiovasc Surg 2012;144:431-7. [Crossref] [PubMed]
- Watanabe S, Asamura H, Miyaoka E, et al. Results of T4 surgical cases in the Japanese Lung Cancer Registry Study: should mediastinal fat tissue invasion really be included in the T4 category? J Thorac Oncol 2013;8:759-65. [Crossref] [PubMed]
- Sakurai H, Asamura H, Miyaoka E, et al. Differences in the prognosis of resected lung adenocarcinoma according to the histological subtype: a retrospective analysis of Japanese lung cancer registry data. Eur J Cardiothorac Surg 2014;45:100-7. [Crossref] [PubMed]
- Inoue M, Okumura M, Sawabata N, et al. Clinicopathological characteristics and surgical results of lung cancer patients aged up to 50 years: the Japanese Lung Cancer Registry Study 2004. Lung Cancer 2014;83:246-51. [Crossref] [PubMed]
- Takei H, Kondo H, Miyaoka E, et al. Surgery for small cell lung cancer: a retrospective analysis of 243 patients from Japanese Lung Cancer Registry in 2004. J Thorac Oncol 2014;9:1140-5. [Crossref] [PubMed]
- Kameyama K, Okumura N, Miyaoka E, et al. Prognostic value of intraoperative pleural lavage cytology for non-small cell lung cancer: the influence of positive pleural lavage cytology results on T classification. J Thorac Cardiovasc Surg 2014;148:2659-64. [Crossref] [PubMed]
- Iida T, Shiba M, Yoshino I, et al. Surgical Intervention for Non-Small-Cell Lung Cancer Patients with Pleural Carcinomatosis: Results From the Japanese Lung Cancer Registry in 2004. J Thorac Oncol 2015;10:1076-82. [Crossref] [PubMed]
- Kondo K, Monden Y. Therapy for thymic epithelial tumors: a clinical study of 1,320 patients from Japan. Ann Thorac Surg 2003;76:878-84; discussion 884-5. [Crossref] [PubMed]
- Kondo K, Monden Y. Lymphogenous and hematogenous metastasis of thymic epithelial tumors. Ann Thorac Surg 2003;76:1859-64; discussion 1864-5.
- Detterbeck FC, Stratton K, Giroux D, et al. The IASLC/ITMIG thymic epithelial tumors staging project: proposal for an evidence-based stage classification system for the forthcoming (8th) edition of the TNM classification of malignant tumors. J Thorac Oncol 2014;9:S65-S72. [Crossref] [PubMed]
- Nicholson AG, Detterbeck FC, Marino M, et al. The IASLC/ITMIG thymic epithelial tumors staging project: proposal for the T component for the forthcoming(8th) edition of the TNM classification of malignant tumors. J Thorac Oncol 2014;9:S73-S80. [Crossref] [PubMed]
- Kondo K, Van Schil P, Detterbeck FC, et al. The IASLC/ITMIG Thymic Epithelial Tumors Staging Project: proposals for the N and M components for the forthcoming (8th) edition of the TNM classification of malignant tumors. J Thorac Oncol 2014;9:S81-7. [Crossref] [PubMed]
- Okuda K, Yano M, Yoshino I, et al. Thymoma patients with pleural dissemination: nationwide retrospective study of 136 cases in Japan. Ann Thorac Surg 2014;97:1743-8. [Crossref] [PubMed]
- Omasa M, Date H, Sozu T, et al. Postoperative radiotherapy is effective for thymic carcinoma but not for thymoma in stage II and III thymic epithelial tumors: the Japanese Association for Research on the Thymus Database Study. Cancer 2015;121:1008-16. [Crossref] [PubMed]
- Nakagawa K, Yokoi K, Nakajima J, et al. Is Thymomectomy Alone Appropriate for Stage I (T1N0M0) Thymoma? Results of a Propensity-Score Analysis. Ann Thorac Surg 2016;101:520-6. [Crossref] [PubMed]
- Yamada Y, Yoshino I, Nakajima J, et al. Surgical Outcomes of Patients With Stage III Thymoma in the Japanese Nationwide Database. Ann Thorac Surg 2015;100:961-7. [Crossref] [PubMed]
- Hishida T, Nomura S, Yano M, et al. Long-term outcome and prognostic factors of surgically treated thymic carcinoma: results of 306 cases from a Japanese Nationwide Database Study. Eur J Cardiothorac Surg 2016;49:835-41. [Crossref] [PubMed]
- Mizuno T, Okumura M, Asamura H, et al. Surgical management of recurrent thymic epithelial tumors: a retrospective analysis based on the Japanese nationwide database. J Thorac Oncol 2015;10:199-205. [Crossref] [PubMed]
- Nakajima J, Okumura M, Yano M, et al. Myasthenia gravis with thymic epithelial tumour: a retrospective analysis of a Japanese database. Eur J Cardiothorac Surg 2016;49:1510-5. [Crossref] [PubMed]