
Modified surgical incision suturing technique in uniportal video-assisted thoracoscopic pulmonary resection
Highlight box
Key findings
• Modified surgical incision suturing technique can promote rapid postoperative recovery in patients after pulmonary resection.
What is known and what is new?
• Modified surgical incision suturing technique can reduce the chance of incision infection and splitting, reduce the severity of postoperative incision scar formation, and promote early healing.
• This study improved the suture method of conventional surgical incision in order to reduce the probability of wound infection and dehiscence, promote early healing, and reduce the severity of postoperative wound scar, thereby enhancing the postoperative rapid recovery of patients.
What is the implication, and what should change now?
• We have improved the conventional surgical incision suture method, which can reduce postoperative incision pain, the severity of surgical scars and the chance of infection and dehiscence. Furthermore, it can improve the aesthetic appearance of the incision and have favorable effects on the physical and mental health of patients. Our study demonstrated that the modified surgical incision suture method can be safely and effectively applied to the incision suture of uniportal thoracoscopic pulmonary resection.
Introduction
In recent years, with the continuous development of minimally invasive approach and spreading of enhanced recovery after surgery (ERAS), the application of video-assisted thoracoscopic surgery (VATS) in thoracic surgery is becoming increasingly widespread (1). To date, uniportal thoracoscopic surgery is one of the most used surgical techniques. Compared with traditional thoracotomy and multi-hole thoracoscopic surgery, uniportal thoracoscopic surgery can minimize the surgical trauma, reduce the probability of intercostal nerve injury, reduce the pain of posterior incision, and shorten the postoperative recovery time, thus enabling rapid recovery (2,3).
In recent years, with the rapid development of the economy and society, the progress of medicine, and the improvement of living standards, people’s aesthetic desires have been continuously increasing. Patients and their families are no longer simply satisfied with the effect of the surgical treatment; the healing of postoperative wounds has gradually become a concern. At present, single-hole thoracoscopic surgery technology is widely used in major medical centers and chest-specialized hospitals for the treatment of lung diseases. However, the uniportal surgery method focuses on one incision, and all surgical instruments need to pass through the same hole, resulting in repeated extrusion and tissue damage of the surgical incision. At the same time, thermal burns may result from open chest and closed chest electrocoagulation hemostasis. Furthermore, the chest tube is placed through the uniportal incision at the end of the surgical procedure. The above factors can lead to poor or delayed healing of the surgical incision, infection and cracking. These factors can cause varying degrees of harm to the physiology and psychology of patients (4,5).
The traditional discontinuous vertical mattress suture is the most commonly used suture method for thoracic surgical incision (6), but the high tension of this method may lead to a number of wound healing problems such as wound dehiscence and wound infection. Therefore, we have improved this suture method in order to reduce the probability of wound infection and dehiscence, promote early healing, and reduce the severity of postoperative wound scarring, thus promoting a rapid postoperative recovery of patients. The purpose of this study is to explore the clinical efficacy of a modified surgical incision suture technique applied to uniportal thoracoscopic pulmonary resection. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1968/rc).
Methods
In this retrospective study, 151 patients who were admitted to our Department of Thoracic Surgery at the North District of Suzhou Municipal Hospital and underwent pulmonary resection from January 2019 to October 2021 were included. All operations were completed by the same surgeon and assistant. The surgical incisions were divided into two groups according to different sutures, including 77 cases in the modified group and 74 cases in the conventional group, of which 72 cases were male and 79 cases were female, 71 cases were lobotomies, and 80 cases were sublobar resections. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Suzhou Municipal Hospital (No. KL901425), and all patients signed the informed consent form.
Case inclusion criteria: (I) age ≥18 years old, regardless of gender; (II) surgical procedures including pulmonary sleeve resection, lobectomy, segmental lung resection, and pulmonary wedge resection; (III) cardiopulmonary function and other preoperative tests to tolerate this operation; (IV) uniportal thoracoscopic surgery.
Case exclusion criteria: (I) preoperative examination and cardiopulmonary function assessment showed that the patient could not tolerate the surgery; (II) body mass index (BMI) >28 kg/m2; (III) intraoperative uniportal thoracoscopy was converted to multi-port thoracoscopy or thoracotomy; (IV) patients with previous history of keloid.
Surgical methods (Figure 1)
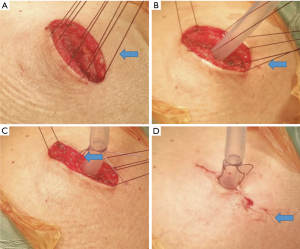
All patients were placed under intravenous compound general anesthesia, with double-lumen tracheal intubation, in the lateral healthy-side-down position, and the surgical incision was selected between the fourth or fifth ribs (length 3–5 cm) in the anterior axillary line. Surgical procedures included lobectomy, wedge resection, or segmental resection. After the intrathoracic operation, the modified group received the improved surgical incision suture technology to suture the surgical incision. The specific process was as follows: surgical incision of adequate subcutaneous and muscular layers was strictly hemostatic, and excessive burns to the skin and subcutaneous fat layer were avoided as much as possible. A large circular needle #7 silk suture (SA86G, ETHICON, New York, USA) was interrupted to close the lateral muscle layer at the rib level, avoiding suturing the intercostal muscle. The thoracoscope was placed to make sure that the surgical incision was free of bleeding and the chest tube was placed to expand the lung and then the thoracoscope was withdrawn, and the #7 silk suture was tied to close the muscular layer. The subcutaneous fat layer and deep fascia were sutured with #4 silk sutures (SA85G, ETHICON) in large circular needles, and double sutures were feasible in obese patients. The adipose tissue and deep fascia near the chest tube were closed and tightened with 2-0 absorbable sutures, followed by knotting the thread at 0.5 cm from the skin and fixing the chest tube. The single head barbed absorbable suture was used for intradermal suture, and the head end could be tied with silk thread to avoid slipping into the skin. During suturing, the suture could be gradually tightened to enable the skin to have a certain retraction tension. The suture to the chest tube could be closed to the chest tube, but care was taken to avoid excessively surrounding the chest tube. At the end of suture, the needle could be inserted under the skin to a distance of 2–3 cm, and a suture of 3–5 cm could be left. The suture could be tightened gradually so that the skin retained a certain retraction tension, and the suture could be tightened to the chest tube but with care taken to avoid overly surrounding the chest tube. In the control group, the intra-thoracic surgical operation was the same as that of the modified group, and the surgical incision was closed with a large circular needle and #7 silk suture to intermittently close the lateral muscle layer at the rib level and avoid suturing the intercostal muscle. The thoracoscope was inserted to make sure that the surgical incision was free of bleeding, the chest tube was placed to expand the lung, and then the thoracoscope was withdrawn. A #7 silk thread was tied to close the muscle layer, 2-0 absorbable sutures (VCP345H, ETHICON) were used to close the knot and tighten the knot, after which the thread was tied at 0.5 cm from the skin and the chest tube was fixed. A #4 silk thread with large circular needle was used to close the subcutaneous fat layer and deep fascia, and #4 silk thread with large circular needle was used to close the skin layer.
Postoperative management
All patients returned to the thoracic surgery ward after extubation. On the first day after surgery, bedside chest radiographs were performed to check the pulmonary expansion and the accumulation of blood and air in the chest cavity; on the second day after surgery, a routine blood analysis was performed, and patients were encouraged to get out of bed early. The discharge criteria included chest tube removal without complications, and normal results in the postoperative blood routine.
Postoperative incisional pain score
The visual analogue scale (VAS) (7) was used to score the pain of the postoperative surgical incision. The VAS is a linear scoring method that uses a scale of 0–10 mm, with 0 indicating no pain and 10 indicating the most severe pain. Patients were asked to mark the severity of pain on the scale according to their perception of pain in the surgical incision and to measure the distance from the starting point to the mark as a score: the higher the score, the more severe the pain.
Postoperative incision healing and scar scoring
Postoperative surgical incision scars were assessed using the Vancouver scar scale (VSS) (8), which is the most widely used scar evaluation scale in clinical studies and provides extensive objective information, mainly including vascular distribution status, tenderness, pigmentation, and height; the lowest score is 0, representing normal skin; the highest score is 13, representing the worst scar condition. The questionnaire was completed by professional medical staff of thoracic surgery after one month of operation. When the healing level of the surgical incision is grade B, we consider the wound to be infected (8).
Statistical analysis
Data were analyzed using the software SPSS 25.0 (IBM Corp., Armonk, NY, USA), and measurement data conforming to a normal distribution were expressed as mean ± standard deviation () and compared between groups using the independent samples t-test; measurement data not conforming to a normal distribution were expressed as median and interquartile spacing {M [P25, P75]} and compared using the Wilcoxon rank sum test; the count data were expressed as frequencies or percentages, and the standard chi-square test was used for comparison between groups. The test level was set at 0.05, and P<0.05 was considered a statistically significant difference.
Results
Comparison of general clinical data between the two groups of patients
From January 2019 to October 2021, the patients were divided into a modified group (77 cases) and a conventional group (74 cases) according to the different incisional sutures, among which 72 were male patients and 79 were female patients, 71 were lobectomies and 80 were sublobar resections (including lung segment and lung wedge resections), and the detailed clinical data of the two groups are shown in Table 1.
Table 1
| Characteristics | Group A (n=74) | Group B (n=77) | t | P value |
|---|---|---|---|---|
| Gender | 2.368 | 0.124 | ||
| Male | 40 (54.1) | 32 (41.6) | ||
| Female | 34 (45.9) | 45 (58.4) | ||
| Age, year | 54.47±17.16 | 55.73±14.22 | −0.490 | 0.625 |
| Smoking | 0.522 | 0.470 | ||
| Yes | 12 (16.2) | 16 (20.8) | ||
| No | 62 (83.8) | 61 (79.2) | ||
| Surgical site | 0.088 | 0.767 | ||
| Left | 29 (39.2) | 32 (41.6) | ||
| Right | 45 (60.8) | 45 (58.4) | ||
| Hypertension | 0.854 | 0.356 | ||
| Yes | 18 (24.3) | 14 (18.2) | ||
| No | 56 (75.7) | 63 (81.8) | ||
| Diabetes | 0.005 | 0.943 | ||
| Yes | 6 (8.1) | 6 (7.80) | ||
| No | 68 (91.9) | 71 (92.2) | ||
| Heart disease | 1.157 | 0.282 | ||
| Yes | 3 (4.1) | 1 (1.3) | ||
| No | 71 (95.9) | 76 (98.7) | ||
| Duration of surgery, minutes | 112.05±49.17 | 113.18±56.29 | 0.389 | 0.896 |
| Intraoperative blood loss, mL | 48.14±72.07 | 47.32±65.48 | 0.072 | 0.946 |
| Chest tube duration, days | 3.26±1.81 | 3.14±1.79 | 0.388 | 0.699 |
| BMI, kg/m2 | 22.80±3.00 | 23.39±3.62 | 1.101 | 0.273 |
| Postoperative drainage, mL | 390.95±319.17 | 410.71±306.18 | −0.388 | 0.698 |
Data are presented as n (%) or mean ± standard deviation. Group A, conventional group; group B, modified group; BMI, body mass index.
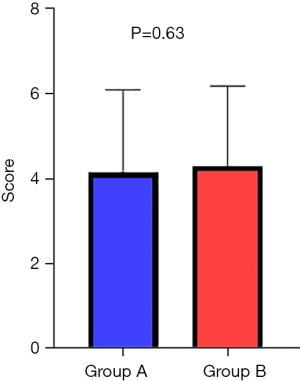
Comparison of postoperative incisional pain scores between two groups of patients
The postoperative incisional pain score was 4.149 in the group with conventional incisional sutures and 4.299 in the group with modified incisional sutures, with no statistical difference between the two groups (P=0.63), as shown in Figure 2.
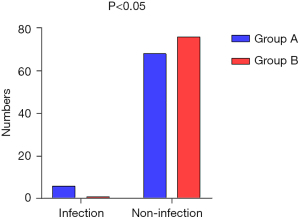
Comparison of incisional infection rates between two groups of patients
The incidence of incisional infection was 6.7% (5/74) in group A and 1.3% (1/77) in group B. The incidence of incisional infection in group A was lower than that in group B, and the difference was statistically significant (P<0.05), as shown in Figure 3.
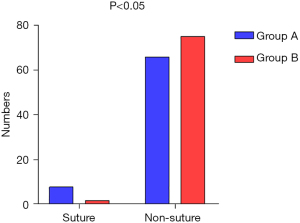
Comparison of the secondary suture rate between the two groups of patients
The incidence of secondary incision sutures was 9.4% (7/74) in group A and 2.6% (2/77) in group B. The incidence of secondary incision sutures in group A was lower than that in group B, and the difference was statistically significant (P<0.05), as shown in Figure 4.
Comparison of postoperative incision scar scores between the two groups of patients
The postoperative scar score was 5.543 in the incision conventional suture group and 4.853 in the incision modified suture group, and the scar score of the incision modified suture group was better than that of the incision conventional suture group, and the difference between the two groups was statistically significant (P=0.03), as shown in Figure 5.

Discussion
With the development of VATS, pulmonary surgery has evolved from traditional open surgery to minimally invasive thoracoscopic surgery, and from multi-port to uniportal surgery, reducing the surgical trauma (9). As surgeons’ attention is mainly focused on surgical techniques and intra-thoracic operations, it is easy to neglect the healing of surgical incisions. In this study, the incision suturing method of single-port thoracoscopic lung surgery was improved to significantly improve the aesthetics of the surgical incision and reduce scar formation, which can be safely and effectively used for this purpose.
The formation of a postoperative surgical incision scar is a normal physiological process of post-traumatic healing of human tissue (10). During this process, normal skin tissue is replaced by pathological tissue with poor morphology and texture. Scar tissue is mainly composed of crisscross collagen fiber bundles. If these fiber bundles proliferate excessively, a series of problems affecting the appearance or function of the body could develop, such as destruction of the body surface morphology, dysfunction of joint function and activity, and even developmental disorders. At the same time, patients may experience a great psychological trauma, leaving them prone to depression, anxiety and social avoidance (4,11), which seriously reduces the quality of life of patients after surgery. Therefore, the healing of a postoperative wound should be paid more attention to by surgeons. Atkinson et al. (12) found that after breast reduction, for incisions with high tension, strengthening and closing with tensile glue can reduce the generation of scar tissue compared with the blank control group, indicating that tension promotes the production of a large amount of collagen, which leads to the formation of scarring. Ogawa et al. (13) also showed that distal tension reduction can disperse the tension of the wound margin remotely and even to the fascial layer, which is conducive to reducing the formation of scar. The wound healing and scar score of the modified group in this study were better than those of the conventional group. The reason may be that the single-head barbed absorbable suture used in this study can reduce the incision tension and the severity of postoperative incision scarring (4).
There are many clinical scales to evaluate linear scarring, the most representative of which are: VSS (14), VAS (15), and Patient and Observer Scar Assessment Scale (POSAS) (16). The VSS is the most widely used scar assessment scale in clinical research and provides much objective information, including vascular distribution status, tenderness, pigmentation, and height; the lowest score is 0, which represents normal skin, and the highest score is 13, which represents the worst scar condition. Previous studies have shown that the VSS can better assess the healing of postoperative incisions (8,14). Thus, we used this method to evaluate linear scarring in our study.
There are increased complications for poorly healed infected wounds. The minimally invasive surgical incisions can appear to crack, ooze, and especially heal with excessive scar growth, thus aggravating the patient’s postoperative pain, affecting the aesthetics of the incision, and bringing a series of negative effects on the patient’s physical and mental health. Through the summary of the previous related literature, we found that the causes of the above incisional healing defects are as follows: (I) minimally invasive surgery, especially uniportal surgery, increased the chance of burns, postoperative aseptic necrosis, fat liquefaction and can lead to incision healing delay because of the surgical incision of blood leakage, especially during the deep muscle hemostasis. (II) The increase in the number of surgical instruments inserted through the single-hole causes pressure and friction on the incision tissue, resulting in local ischemic necrosis and affecting wound healing (17). (III) The retention of chest tubes can affect incision healing. At the same time, the traditional suture incision appears as a “centipede” surgical scar after healing, which affects the aesthetics. In this regard, we have improved the surgical suture method. In the early stage, we used 3-0 absorbable sutures to close the surgical incision and tightened the absorbable sutures on both sides during extraction, which also achieved good results, but this method has the following shortcomings: (I) #3 absorbable sutures may become snagged on the lateral orifice of the chest tube during extraction, resulting in difficulty in extraction and painful incision. (II) Although the incision is closed by double pulling and tightening of the sutures, poor closure of the incision may still occur, resulting in poor healing. In this regard, we replaced the 3-0 absorbable suture with a single barbed absorbable suture, which has the following advantages: the improved suture method brings more parallel pressure by continuously suturing the subcutaneous layers horizontally, evenly dispersing the suture tension in each layer, which helps to reduce pain and promote incision healing (18).
There are also some limitations in this study. First, this study did not conduct a detailed study of the psychological satisfaction of patients. Second, the sample size of this study is small, and there may be data bias for grouping surgical incisions with different suture methods. Third, this study is a retrospective study with a single center and small sample. As a result, there may be deviation that needs to be supported by a multi-center and large sample prospective study.
Conclusions
We have improved the conventional surgical incision suture method, which can reduce postoperative incision pain, reduce the severity of surgical incision scars, improve the aesthetic appearance of the incision, reduce the chance of incision infection and dehiscence, promote early healing, and have favorable effects on patients. Our study demonstrated that the modified surgical incision suture method can be safely and effectively applied to the incision suture of uniportal thoracoscopic pulmonary resection, which promotes rapid postoperative recovery of patients and is worth promoting.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1968/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1968/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1968/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1968/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Suzhou Municipal Hospital (No. KL901425), and all patients signed the informed consent form.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yang HX, Woo KM, Sima CS, et al. Long-term Survival Based on the Surgical Approach to Lobectomy For Clinical Stage I Nonsmall Cell Lung Cancer: Comparison of Robotic, Video-assisted Thoracic Surgery, and Thoracotomy Lobectomy. Ann Surg 2017;265:431-7. [Crossref] [PubMed]
- Ahn S, Moon Y. A comparison of the short-term outcomes of simple and complex segmentectomy via uniportal video-assisted thoracoscopic surgery. J Thorac Dis 2023;15:5386-95. [Crossref] [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomes. Eur J Cardiothorac Surg. 2016;49:i37-i41. [Crossref] [PubMed]
- Namazi MR, Fallahzadeh MK, Schwartz RA. Strategies for prevention of scars: what can we learn from fetal skin? Int J Dermatol 2011;50:85-93. [Crossref] [PubMed]
- Kannan S, de Golian E, Lee N, et al. A Split-Scar Study Investigating the Effectiveness of Early Intervention With Electroabrasion on Improving the Cosmetic Appearance of Postsurgical Scars. Dermatol Surg 2020;46:1300-5. [Crossref] [PubMed]
- Zuber TJ. The mattress sutures: vertical, horizontal, and corner stitch. Am Fam Physician 2002;66:2231-6.
- Wang Z, Wang M, Wen S, et al. Types and applications of cough-related questionnaires. J Thorac Dis 2019;11:4379-88. [Crossref] [PubMed]
- Bagheri M, von Kohout M, Fuchs PC, et al. How to evaluate scar colour after burn injuries - A clinical comparison of the Mexameter® and the subjective scar assessment (POSAS/VSS). Burns 2023; [Crossref]
- Han D, Cao Y, Wu H, et al. Uniportal video-assisted thoracic surgery for the treatment of lung cancer: a consensus report from Chinese Society for Thoracic and Cardiovascular Surgery (CSTCVS) and Chinese Association of Thoracic Surgeons (CATS). Transl Lung Cancer Res 2020;9:971-87. [Crossref] [PubMed]
- Kerwin LY, El Tal AK, Stiff MA, et al. Scar prevention and remodeling: a review of the medical, surgical, topical and light treatment approaches. Int J Dermatol 2014;53:922-36. [Crossref] [PubMed]
- Gladstone HB, Berg D, McDonald M. Scar revision. Dermatol Res Pract 2010;2010:545796. [Crossref] [PubMed]
- Atkinson JA, McKenna KT, Barnett AG, et al. A randomized, controlled trial to determine the efficacy of paper tape in preventing hypertrophic scar formation in surgical incisions that traverse Langer's skin tension lines. Plast Reconstr Surg 2005;116:1648-56; discussion 1657-8. [Crossref] [PubMed]
- Ogawa R, Akaishi S, Huang C, et al. Clinical applications of basic research that shows reducing skin tension could prevent and treat abnormal scarring: the importance of fascial/subcutaneous tensile reduction sutures and flap surgery for keloid and hypertrophic scar reconstruction. J Nippon Med Sch 2011;78:68-76. [Crossref] [PubMed]
- Baryza MJ, Baryza GA. The Vancouver Scar Scale: an administration tool and its interrater reliability. J Burn Care Rehabil 1995;16:535-8. [Crossref] [PubMed]
- Duncan JAL, Bond JS, Mason T, et al. Visual analogue scale scoring and ranking: a suitable and sensitive method for assessing scar quality? Plast Reconstr Surg 2006;118:909-18. [Crossref] [PubMed]
- van de Kar AL, Corion LU, Smeulders MJ, et al. Reliable and feasible evaluation of linear scars by the Patient and Observer Scar Assessment Scale. Plast Reconstr Surg 2005;116:514-22. [Crossref] [PubMed]
- Çetin K, Sikar HE, Kocaoğlu AE, et al. Evaluation of intradermal absorbable and mattress sutures to close pilonidal sinus wounds with Limberg flap: a prospective randomized comparative study. Ann Surg Treat Res 2018;94:88-93. [Crossref] [PubMed]
- Minaev SV, Vladimirova OV, Kirgizov IV, et al. Multicenter study of the effectiveness of antiscar therapy in patients at different age periods. Khirurgiia (Mosk) 2020;51-8. [Crossref] [PubMed]


