
Simultaneous bilateral spontaneous pneumothorax with congenital pleuro-pleural communication
Introduction
Spontaneous pneumothorax is rarely life-threatening, although patients with simultaneous bilateral pneumothorax may deteriorate rapidly, sometimes due to bilateral tension pneumothorax. The cause of simultaneous bilateral pneumothorax varies, and 34-58% of cases are associated with underlying lung disease. A single pleural space can lead to severe bilateral pneumothorax after heart-lung transplantation, major cardiothoracic surgery with median sternotomy, or esophageal surgery (1), and is sometimes called “iatrogenic buffalo chest”, in reference to the single pleural cavity of the North American buffalo. Congenital communication between pleural cavities has also been reported (2). Non-standard diagnostic and therapeutic strategies may be necessary for pneumothorax with pleuro-pleural communication. We report a patient with pleuro-pleural communication who underwent surgical treatment.
Case report
A previously healthy 35-year-old man without a history of smoking presented with left chest pain. Chest X-ray showed simultaneous bilateral pneumothorax. The pneumothorax was large on the right side (≥3 cm apex-to-cupola distance) and small on the left (<3 cm). He was clinically stable. Chest computed tomography (CT) scans revealed small bullae on both lungs. A small air space between the esophagus and aorta was also observed, suggesting pleuro-pleural communication, as confirmed later (Figure 1A). The patient consented to bilateral bullectomy.
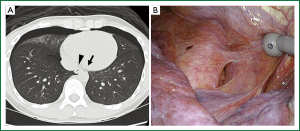
Video-assisted thoracoscopic surgery was planned first on the right side which had the large pneumothorax, and a chest tube was inserted into the left side in the operating room and showed no evidence of air leaks. During the right thoracoscopy, water that was poured to test for air leaks was observed escaping from the right pleural cavity to the left-side chest tube. Pleuro-pleural communication was suspected but not detected. Staple bullectomy and coverage with a polyglycolic acid sheet and fibrin glue were performed for the bulla on the right middle lobe and then for the bullae on the left upper lobe. Repeated inspection revealed a 2-cm-long pleural window posterior to the inferior pulmonary ligament, between the aorta and esophagus (Figure 1B). The window was packed with a polyglycolic acid sheet and fibrin glue and covered using a collagen patch coated with human fibrinogen and thrombin. The postoperative course was uneventful.
Discussion
Simultaneous bilateral spontaneous pneumothorax with congenital pleuro-pleural communication has been reported in four patients, including the present patient (2). Although congenital pleuro-pleural communication has been regarded as rare, as many as nine patients have been reported (if suspected cases are included). In addition to pneumothorax, a common pleural cavity with communication along the anterior mediastinum was accidentally diagnosed in a 3-year-old boy who had undergone surgical treatment for funnel chest (3). Although not confirmed by surgery, congenital pleuro-pleural communication was suspected in three patients who suffered bilateral pneumothorax after unilateral thoracic puncture due to insertion of a central venous catheter (4) or percutaneous needle biopsy (5,6). Another patient, an 18-year-old female, was reported to have bilateral pneumothorax that resolved after insertion of a single chest tube, although suspected pleuro-pleural communication was not detected during surgery (7).
Reported sites of congenital pleuro-pleural communication were the anterior mediastinum in two patients and the lower middle mediastinum in three (2,3). Among the three patients with middle mediastinal communication, two (including the present patient) had similar pleural windows located between the aorta and esophagus (2). The other one patient had a wide defect of the middle mediastinal septum, from the tracheal carina to the diaphragm, and had a history of surgical treatment for Tetralogy of Fallot and a complete defect in the left pulmonary artery. A wide defect in the middle mediastinal septum has also been seen in patients with horseshoe lung, a rare anomaly characterized by fusion of the posterobasal portions of the both lungs, behind the pericardial reflection, or sometimes behind the esophagus (8). Lower middle mediastinal communication should be carefully inspected during surgery.
Among the surgically treated four patients with congenital pleuro-pleural communication, insertion of a single chest tube resolved bilateral pneumothorax in three patients (2). Pleuro-pleural communication was suspected preoperatively in one patient, and perioperatively in three patients, because poured water escaped into the contralateral chest tube. Unilateral bullectomy and closure of the pleuro-pleural communication were performed in two patients, and bilateral surgery was performed in the other two patients. Closure of the pleuro-pleural communication is essential to prevent recurrence of bilateral pneumothorax. Although we performed the closure by covering, direct suture is a recommended alternative. Parietal pleurectomy has been reported to obliterate the anterior mediastinal window.
Congenital pleuro-pleural communication should be considered in cases of simultaneous bilateral primary spontaneous pneumothorax. Radiologic examination after insertion of a single chest tube may yield diagnostic clues. In addition, the anterior and lower middle mediastinum should be carefully inspected. Closure of the pleuro-pleural communication is essential to prevent fatal bilateral recurrence.
Acknowledgements
We thank David Kipler for his editorial review of this manuscript.
Disclosure: The authors declare no conflict of interest.
References
- Eguchi T, Hamanaka K, Kobayashi N, et al. Occurrence of a simultaneous bilateral spontaneous pneumothorax due to a pleuro-pleural communication. Ann Thorac Surg 2011;92:1124-6. [PubMed]
- Yamada S, Yoshino K, Inoue H. Simultaneous bilateral spontaneous pneumothorax with pleural window communicating with bilateral pleural spaces. Ann Thorac Surg 2008;85:1434-6. [PubMed]
- Barauskas V, Kilda A. Common pleural cavity in combination with pectus excavatum. Medicina (Kaunas) 2004;40:565-8. [PubMed]
- Pazos F, Masterson K, Inan C, et al. Bilateral pneumothoraces following central venous cannulation. Case Report Med 2009;2009:745713.
- Yamaura H, Inaba Y, Sato Y, et al. Bilateral pneumothorax after unilateral transthoracic puncture. J Vasc Interv Radiol 2007;18:793-5. [PubMed]
- Gruden JF, Stern EJ. Bilateral pneumothorax after percutaneous transthoracic needle biopsy. Evidence for incomplete pleural fusion. Chest 1994;105:627-8. [PubMed]
- Hartin DJ, Kendall R, Boyle AA, et al. Case of the month: Buffalo chest: a case of bilateral pneumothoraces due to pleuropleural communication. Emerg Med J 2006;23:483-6. [PubMed]
- Männer J, Jakob C, Steding G, et al. Horseshoe lung: report on a new variant—“inverted” horseshoe lung--with embryological reflections on the formal pathogenesis of horseshoe lungs. Ann Anat 2001;183:261-5. [PubMed]


