Application of non-invasive mechanical ventilation in an asthmatic pregnant woman in respiratory failure: a case report
Introduction
The efficiency of non-invasive mechanical ventilation (NIV) has been proven, especially in cases of chronic obstructive pulmonary disease (COPD) presenting in hypercarbic respiratory failure (1). However, its use in hypoxic respiratory failure is controversial (1-5), and there is no consensus on its use in pregnant women. Similarly, the use of NIV during an asthma attack is also controversial. Herein, we report a case of a 28-year-old female patient in her 16th week of pregnancy who presented during an asthma attack with community-acquired pneumonia, which led to hypoxic respiratory failure. She recovered with the use of NIV along with medical treatment. This case is worth discussing since it included two controversial clinical conditions, and explains how they can be successfully treated.
Case report
A 28-year-old female patient in the 16th week of pregnancy who was using bronchodilators due to asthma suffered an influenza infection 1 week before presentation. Her signs had been mild at first but were increased with severe coughing that produced yellowish phlegm. Shortness of breath followed, which became severe during the use of acidic cleaning detergents directly before presentation to the emergency department. On physical examination, she was fully conscious and cooperative, tachypneaic (38 breaths/min), tachycardic (110 beats/min) and her ABP was 120/70 mmHg. There were rough bilateral respiratory sounds, widely scattered rhonchi and inspiratory rales in the left lower lung field. In the obstetrical consultation, the uterine height was compatible with a 16-week pregnancy and the fetal cardiac sounds were normal.
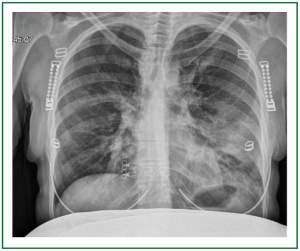
Arterial blood gas analysis revealed hypoxia and hypocapnia, with a PaO2/FiO2 ratio of 250, and the APACHE II score was calculated as 20. The arterial blood gas values are summarised in Table 1. On the posteroanterior (PA) chest X-ray, consolidation was observed in the left lower zone along with an air bronchogram (Figure 1). Sinus tachycardia was found to be compatible with left ventricular function on an electrocardiogram.
Table 1
| Time | VS mode | pH | PaCO2 (mmHg) | PaO2 (mmHg) | HCO3 (mmol/L) | SO2 (%) | PsO2 (%) |
|---|---|---|---|---|---|---|---|
| ER | 15 L/min, nasal O2 | 7.33 | 34 | 42 | 18 | 75 | 68 |
| H0, ICU | 15/5 cmH2O FiO2%50 |
7.35 | 33 | 52 | 18 | 85 | 85 |
| H2nd | 20/5 cmH2O FiO2%60 |
7.36 | 32 | 76 | 18.5 | 95 | 95 |
| H6th | 20/5 cmH2O FiO2%50 |
7.4 | 31 | 68 | 19.8 | 93.7 | 95 |
| H10th | 20/5 cmH2O FiO2%50 |
7.4 | 29 | 71 | 18 | 94 | 95 |
| H18th | 20/5 cmH2O FiO2%50 |
7.43 | 27 | 68 | 18.2 | 94.2 | 96 |
| H27th | 20/5 cmH2O FiO2%50 |
7.39 | 32 | 100 | 20.1 | 97 | 98 |
| H32nd | 10 L/min O2 | 7.42 | 26 | 130 | 17 | 99 | 99 |
| H54th | 2 L/min O2 | 7.37 | 34 | 57 | 20 | 90 | 94 |
Abbreviations: ER, Emergency room; H, Hour; ICU, Intensive care unit; psO2,oxygen saturation with pulse oximeter; VS, Ventilatory support.
Complete blood count showed white blood cell count 22.0, CRP 10.5, haemoglobin 13 g/dL and haematocrit 38%.
In the intensive care unit, the patient was placed on mask O2 at 14 L/min, and her oxygen saturation was measured as 85% with pulse oximetry. She was administered NIV with IPAP: 15, EPAP: 5 cm H2O, FiO2: 50% (BiPAP Vision, Philips Respironics, The Netherlands). Oxygen saturation reached 90% at the fourth hour. The pressures were gradually increased, and the saturation reached 96% at the 10th hour of treatment. The patient was prescribed ampicillin 4 g, after which Streptococcus mitis was cultured from the sputum, and was found to be susceptible to ampicillin.
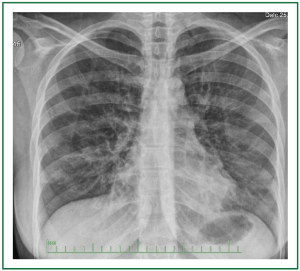
Intermittent NIV was applied for a total of 27 h with the first 16 h being continuous. The oxygen requirements of the patient significantly decreased 48 h after admission to intensive care. The saturation was 95% when 3 L/min O2 was administered with a nasal cannula. The leukocyte count and CRP decreased, and her respiratory and cardiac rates normalised. On thoracic auscultation, rales persisted in the left lower zone, but the rhonchi had significantly regressed in all zones. A regression was observed on PA chest X-ray (Figure 2). The patient was deemed sufficiently stable to be transferred out of intensive care.
Discussion
NIV is a form of ventilatory support that is increasingly used in patients in hypercarbic respiratory failure (1,2). However, there is still no consensus on its use in hypoxic respiratory failure (4). Nevertheless, a growing number of studies have demonstrated that NIV prevents the need for intubation and decreases mortality and hospitalisation time when it is used in hypoxic respiratory failure (1,3,5). The primary goal of the use of NIV is to restore the gas exchange and reduce the respiratory workload without intubation.
Asthma is the most common disease leading to complications during pregnancy (6). It affects 3-12% of pregnant women worldwide, and its prevalence in this subset is increasing (7). Asthma may improve, worsen or remain unchanged during pregnancy. The worsening of asthma during pregnancy has been associated with the patient previously being asthmatic, discontinuation of inhaled corticosteroids, and viral infections, to which pregnant women are more prone due to changes in cell-mediated immunity. This may be one of the main underlying causes of asthma attacks (7-9). Severe attacks requiring hospitalisation may be seen during all stages of pregnancy, but they often occur at 21-24 weeks. Attacks requiring hospitalisation occur in 1.6% of asthmatic pregnant women, while 12.6% of these women present to emergency departments (9). Also, intubation is eight times more likely to be difficult in pregnant women than in non-pregnant women (10). Soft tissue oedema makes the airway anatomy invisible, increasing the risk for hypoxaemic cardiac arrest and pulmonary aspiration. Therefore, NIV administered under close monitoring may be life-saving in cases of respiratory failure in pregnant women, as demonstrated here.
Treatment of asthmatic pregnant women requires special consideration to protect the foetus from hypoxic injury. Hormones such as progesterone and β-human chorionic gonadotropin cause changes in the respiratory system during pregnancy, such as the height of the diaphragm, which rises approx. 2 cm due to changes in the anteroposterior and transverse diameter of the rib cage in response to increased respiratory stimulation. This factor must be considered in NIV implementation, and lower pressures must be used in the initial stages to avoid dynamic hyperinflation and reduce the respiratory workload (6).
The objective in pregnant women with respiratory failure is to provide efficient oxygenation and simultaneously implement mechanical ventilation to protect the lungs.
In spite of these data, there are few case reports of NIV implementation (10-14). In these series, NIV successfully prevented the need for intubation and decreased hospitalisation time. In four cases with acute chest syndrome due to sickle-cell anaemia, Al-Ansari et al. successfully applied NIV and stated that its implementation under close monitoring in hypoxic respiratory failure in pregnant women would shorten hospitalisation and ICU times (11). Banga et al. managed acute respiratory distress and hypoxic respiratory failure that had developed due to community-acquired pneumonia in a pregnant woman similar to our case with 3 days of NIV, after which the patient was transferred to the ward on the third day (12). In our patient, NIV was implemented for 27 h, after which she was disconnected from the ventilator and taken to the ward. Several studies have reported that early NIV implementation is beneficial in pneumonia cases and ARDS, but there is still no consensus on this issue (1-4).
This case contained some clinical features that should be emphasised. First, it demonstrated that viral infections may induce an asthma attack and facilitate pneumonia. Also, discontinuation of inhaled steroids can lead to hyper-reactivity of the airway towards respiratory tract irritants. As a result, the patient developed an asthma attack and lobar pneumonia with hypoxic respiratory failure. Since reduction of the respiratory workload was impossible with medical therapy at this stage, NIV was required, which avoided intubation and its resultant complications.
In conclusion, pneumonia may worsen hypoxia in a pregnant woman in asthma attack. Efficient monitoring and NIV with controlled increases in pressure can eliminate the need for intubation and can overcome acute hypoxic respiratory failure. Since NIV has been utilised in a very limited number of cases, this report is considered a successful clinical contribution.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Ferrer M, Esquinas A, Leon M, et al. Noninvasive ventilation in severe hypoxemic respiratory failure: a randomized clinical trial. Am J Respir Crit Care Med 2003;168:1438-44. [PubMed]
- Organized jointly by the American Thoracic Society, the European Respiratory Society, the European Society of Intensive Care Medicine, and the Société de Réanimation de Langue Française, et al. International Consensus Conferences in Intensive Care Medicine: noninvasive positive pressure ventilation in acute Respiratory failure. Am J Respir Crit Care Med 2001;163:283-91.
- Wysocki M, Antonelli M. Noninvasive mechanical ventilation in acute hypoxaemic respiratory failure. Eur Respir J 2001;18:209-20. [PubMed]
- Keenan SP, Mehta S. Noninvasive ventilation for patients presenting with acute respiratory failure: the randomized controlled trials. Respir Care 2009;54:116-26. [PubMed]
- Gupta D, Nath A, Agarwal R, et al. A prospective randomized controlled trial on the efficacy of noninvasive ventilation in severe acute asthma. Respir Care 2010;55:536-43. [PubMed]
- Elsayegh D, Shapiro JM. Management of the obstetric patient with status asthmaticus. J Intensive Care Med 2008;23:396-402. [PubMed]
- Murphy VE, Clifton VL, Gibson PG. Asthma exacerbations during pregnancy: incidence and association with adverse pregnancy outcomes. Thorax 2006;61:169-76. [PubMed]
- Murphy VE, Gibson PG, Smith R, et al. Asthma during pregnancy: mechanisms and treatment implications. Eur Respir J 2005;25:731-50. [PubMed]
- Cydulka RK, Emerman CL, Schreiber D, et al. Acute asthma among pregnant women presenting to the emergency department. Am J Respir Crit Care Med 1999;160:887-92. [PubMed]
- Bassani MA, de Oliveira AB, Oliveira Neto AF. Noninvasive ventilation in a pregnant patient with respiratory failure from all-trans-retinoic-acid (ATRA) syndrome. Respir Care 2009;54:969-72. [PubMed]
- Al-Ansari MA, Hameed AA, Al-jawder SE, et al. Use of noninvasive positive pressure ventilation during pregnancy: case series. Ann Thorac Med 2007;2:23-5. [PubMed]
- Banga A, Khilnani GC. Use of non-invasive ventilation in a pregnant woman with acute respiratory distress syndrome due to pneumonia. Indian J Chest Dis Allied Sci 2009;51:115-7. [PubMed]
- Hutter DA, Berkowitz R, Davis SE 3rd, et al. Application of continuous positive airway pressure in hypoxemic acute respiratory failure associated with diastolic dysfunction in pregnancy. Congest Heart Fail 2006;12:174-5. [PubMed]
- Mohapatra PR, Dutt N, Khanduri S, et al. Noninvasive ventilation in acute respiratory failure due to H1N1 influenza. Lung India 2011;28:49-51. [PubMed]