Penetrating thoracic injury with retained foreign body: can video-assisted thoracic surgery take up the leading role in acute management?
Introduction
Thoracotomy has long been considered the standard approach for exploration in times of thoracic injuries, as it was believed to allow the fullest visualization of injuries, retrieval of foreign bodies, control of bleeding, and resection of damaged lung tissue. However, as video-assisted thoracic surgery (VATS) has been established as the standard approach to most elective thoracic operations with excellent safety profile, it also has a significant role in the emergency management of trauma patients (1,2).
Retained foreign bodies after penetrating thoracic injury pose technical challenges to VATS surgeons. We report three cases of successful use of complete VATS as the first-line approach to exploration and retrieval of retained foreign bodies.
Case presentation
Case 1: where is the blade?
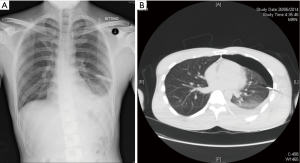
A 27-year-old man was injured by a cutter knife over the left lateral chest wall close to the axilla. He presented with stable haemodynamics with satisfactory oxygen saturation in room air. There was a 3 cm deep chest wall laceration but no foreign body was found. Chest X-ray showed a radio-opacity conforming the shape of a blade and mild left pleural effusion (Figure 1A). Chest drain was inserted yielding 180 mL blood-stained pleural fluid with no air leak. Computed tomography scan showed a hyperdense foreign body in left upper lobe of lung (Figure 1B). An emergency standard 3-port VATS was performed. A rusted cutter blade of 5.5 cm length with sharp ends penetrated partially into the left upper lobe (Figure 2). The blade was removed via the anterior utility port with protection, leaving a 1 cm laceration over the corresponding lobe. Wedge resection of the left upper lobe including the laceration was done using endostaplers. Residual clots were removed, and the pleural cavity was irrigated with 5 litres of warm saline. The total operative time was 45 minutes. Patient had an uneventful post-operative recovery. Chest drain was removed 2 days after the operation and he was discharged on the same day.
Case 2: the fragment of the porcelain vase traveled too far in
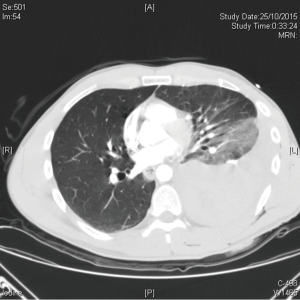
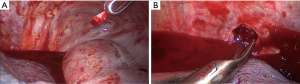
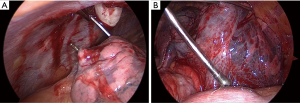
A 41-year-old man tripped and fell after getting drunk, with direct left chest wall impact onto a porcelain vase. He presented with shock and desaturation. Two deep wounds were found over posterolateral left chest wall. Chest X-ray showed haemopneumothorax and subcutaneous emphysema. Computered tomography scan revealed left haemothorax and a hyperdense foreign body over paraspinal soft tissue (Figure 3). Chest drain was inserted yielding 1,400 mL fresh blood. After successful fluid resuscitation and blood transfusion, an emergency exploration was performed using standard 3-port VATS approach. After removal of 1 litre of blood clots, a 1-cm foreign body (likely a fragment of the broken vase) was discovered within the blood clots at the left costophrenic angle (Figure 4A), and it was removed with protection. An arterial bleeder from the left 9th intercostal artery from the posterior penetrating wound was identified (Figure 4B), and it was controlled with metal clips and cauterization. There were no obvious lung lacerations, and underwater tests demonstrated no air leak from the left lung. The total operative time was 90 minutes. Patient recovered uneventfully. Chest drain was removed 3 days after the operation, and patient was discharged on the same day.
Case 3: a fortunate man who unfortunately survived from a suicide
A 37-year-old man, was found drunk and committed suicide in a warehouse. Collateral history suggested that patient fired multiple nails, using a pressurized air stapler, directed to the left chest. On arrival to the emergency department, his blood pressure was 160/110 mmHg, pulse rate was 110 bpm, SpO2 was 100% in room air. Three entry wounds were noted near the left nipple, but no exit wound was found elsewhere. Chest X-ray showed multiple fine nails entered the left lung field but did not traverse the heart shadow (Figure 5A,B); no pneumothorax or pleural effusion were evident. Echocardiogram showed no pericardial effusion or foreign body inside cardiac chambers. Contrast computed tomography scan of the thorax showed all the nail were distant from major cardiovascular structures, and all the nails penetrated into the lingular segment and the lower lobe of the left lung (Figure 5C).
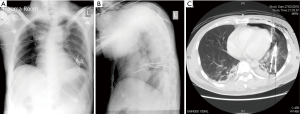
Emergency operation using 2-port VATS was performed after stabilization in the intensive care unit. Four out of eight nails penetrated through the lingular segment and extended into the left lower lobe (Figure 6A); eight nails embedded within the left lower lobe with big intraparenchymal haematoma. The pericardium was intact and there was no haemopericardium. There was no bleeding from the intercostal vessels. The nails in the lingular segment were removed and the lingular segment was resected. As the left lower lobe was destroyed by the nails with formation of a large intraparenchymal haematoma (Figure 6B), a lobectomy (including the remaining eight nails) was performed subsequently, using single staple technique for division of the left lower lobe bronchus and pulmonary artery to minimize manipulation of the lung, and separate division of left inferior pulmonary vein. The pleural cavity was irrigated with 7 litres of warm water. Under-water test detected no air leak, and the residual left upper lobe re-expanded fully under direct vision. The total operative time was 85 minutes.
Patient had an uneventful post-operative recovery. Chest drain was removed 2 days after the operation, and he was discharged to a psychiatry hospital on post-operative day 3.
Discussion
VATS is currently a safe and feasible alternative to thoracotomy in the management of chest trauma (3) especially for haemodynamically stable patients. Its use was widely reported for management of retained haemothorax, persistent pneumothorax, empyema, and mediastinal or diaphragmatic exploration. However, there was only a handful of reports on the use of VATS for penetrating thoracic injuries with retained foreign bodies. Williams et al. published their series of three patients with review of the sparse literature in year 2006 (4). Since then only three isolated cases were reported in the literature concerning the use of VATS in penetrating chest trauma (5-7). There was also no discussion regarding the concomitant performance of lung resection after VATS exploration and foreign body retrieval.
Retained foreign bodies, especially those with sharp tips or edges, have to be dissected and removed with extra caution and meticulousness. Additional inadvertent injuries, especially to the heart and major pulmonary vessels, may occur during retrieval of the foreign body, or during manipulation or traction of lung tissue. VATS may be considered less safe, and therefore under-utilized. Firstly, there was great concern with the use of fine-tipped and lengthy endoscopic instruments and the strict requirement of excellent hand-eye coordination. Secondly, for thoracoscopic exploration, single-lung ventilation is the prerequisite, and this may not be feasible for all trauma patients. Anaesthesiologist experienced in single-lung ventilation (via bronchial blocker or double-lumen tube) is also essential. Thoracotomy can be performed without one-lung isolation, at the expense of more intraoperative blood loss and trauma, and the potential of missing significant pathologies or retained foreign bodies due to hindrance by the non-collapsed lung. The use of thoracoscope in exploration of the pleural cavity provides excellent view, especially over the apex and the costophrenic angles (as illustrated in case 2 while exploring for the broken fragment of the porcelain vase).
Thoracoscopic exploration by experienced VATS surgeons as the first line approach allows clear identification of intrathoracic injuries, control of active bleeders, blood clot evacuation, identification and safe retrieval of foreign bodies even for those with sharp edges or tips, and removal of damaged lung parenchyma with wedge resection or even lobectomy. As demonstrated in case 3, even the ‘extra’ minimally invasive approach (i.e., the 2-port VATS) could be performed, on experienced hands, to resect a lobe of the lung en bloc with retained foreign bodies. There was no clear advantage of conventional thoracotomy over VATS in these regards especially if the patient is stable haemodynamically. It is not justified to create additional major trauma to the chest wall via thoracotomy while VATS could have achieved the same effectiveness with much less tissue damage for the already ‘traumatized’ victims. In patients with relatively stable haemodynamics for which ‘damage-control’ thoracotomy was not urgently indicated, VATS provides a safe and minimally-invasive alternative.
In conclusion, for management of haemodynamically stable patient suffering from penetrating thoracic injury with retained foreign bodies, VATS offers a safe and minimally-invasive alternative to conventional thoracotomy. Meticulous attention should be paid especially for sharp foreign bodies to avoid inadvertent injury to the heart and major pulmonary vessels.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Casós SR, Richardson JD. Role of thoracoscopy in acute management of chest injury. Curr Opin Crit Care 2006;12:584-9. [Crossref] [PubMed]
- Manlulu AV, Lee TW, Thung KH, et al. Current indications and results of VATS in the evaluation and management of hemodynamically stable thoracic injuries. Eur J Cardiothorac Surg 2004;25:1048-53. [Crossref] [PubMed]
- Smith JW, Franklin GA, Harbrecht BG, et al. Early VATS for blunt chest trauma: a management technique underutilized by acute care surgeons. J Trauma 2011;71:102-5; discussion 105-7. [Crossref] [PubMed]
- Williams CG, Haut ER, Ouyang H, et al. Video-assisted thoracic surgery removal of foreign bodies after penetrating chest trauma. J Am Coll Surg 2006;202:848-52. [Crossref] [PubMed]
- Edil BH, Trachte AL, Knott-Craig C, et al. Video-assisted thoracoscopic retrieval of an intrapleural foreign body after penetrating chest trauma. J Trauma 2007;63:E5-6. [Crossref] [PubMed]
- Borgaonkar V, Borgaonkar V. Thoracoscopic retrieval of intra-parenchyamal foreign body of lung. Indian J Surg 2010;72:252-4. [Crossref] [PubMed]
- Dutta R, Kumar A, Das CJ, et al. Emergency video-assisted thoracoscopic foreign body removal and decortication of lung after chest trauma. Gen Thorac Cardiovasc Surg 2010;58:155-8. [Crossref] [PubMed]



