
A preliminary study of modified inflatable mediastinoscopic and single-incision plus one-port laparoscopic esophagectomy
Highlight box
Key findings
• Our secondary modification of inflatable mediastinoscopic esophagectomy improves cervical esophageal mobilization and reduces abdominal trauma by introducing single-incision plus one-port technique.
What is known and what is new?
• Esophageal malignancies have a high morbidity rate worldwide, and inflatable mediastinoscopic and laparoscopic approaches are an emerging area of interest in the treatment of esophageal cancer.
• Building on the primary modification of the inflatable mediastinoscopic technique, we conducted a secondary modification, incorporating innovative surgical instruments. This significantly enhanced the safety and efficiency of the procedure.
What is the implication, and what should change now?
• Our modification introduced an innovative enhancement for traditional inflatable mediastinoscopic esophagectomy procedure, potentially broadening its surgical application.
Introduction
Esophageal cancer is the sixth leading cause of cancer-related death and the eighth most common cancer worldwide (1). The highest incidence rates have been recorded in Eastern Asia and Southern and Eastern Africa (1-4). The therapeutic arsenal against esophageal cancer encompasses an array of strategies, including radiotherapy, chemotherapy, immunotherapy, and surgery. Among these modalities, surgery has a crucial role, due to its high efficacy (5,6). Given the anatomical location of the esophagus along the median line of the body, the surgical approaches for treating esophageal cancer are intricate and diverse. Historically, open techniques, notably including the classical “McKeown” procedure, have held sway in the landscape of esophageal cancer surgery (7,8). Presently, minimally invasive esophagectomy has gained wide acceptance. Nonetheless, surgeons still need to perform separate operations on the cervical, thoracic (thoracoscopic), and abdominal (laparoscopic) regions (9-11).
Inflatable mediastinoscopy combined with laparoscopic esophagectomy was pioneered by Professor Yoshifumi Ikeda in Japan in 2011 (12), and was first performed by Professor Qingdong Cao in China in 2016 (13). The first mediastinoscopic esophagectomy at the Second Affiliated Hospital of Naval Medical University was performed in 2017 (14,15). Since then, we have introduced a primary modification, marked by two key enhancements: (I) extended esophageal mobilization. Departing from the previous practice of mobilizing the esophagus only down to the carina of the trachea, we extended this mobilization distally to the level of the lower pulmonary vein or the diaphragmatic esophageal fissure. This modification alleviates the challenges associated with laparoscopic upward mobilization; and (II) an altered approach for lymphadenectomy: traditionally, subcarinal lymph node resection was performed using an abdominal approach. However, we redefined this procedure by shifting the approach to the cervical incision, thereby augmenting the feasibility of lymphadenectomy. This primary modification has yielded favorable outcomes and progressively gained acceptance among our peers in the field (16-18).
Over the past 3 years, we have introduced a secondary modification to the procedure by introducing the single-incision plus one-port (SI + 1) laparoscopic technique and enhancing the surgical instruments. The secondary modification mainly targets the abdominal phase of the operation. For the cervical phase, our focus remains on improving the surgical instruments. The objective of our secondary modification is to further actualize the concept of “reducing ports” building on the previous concept of “reducing fields”.
Implemented through the incorporation of a single-incision laparoscopic operative approach, our secondary modification procedure aims to minimize abdominal trauma. Additionally, through the innovation of surgical instruments, we have optimized exposure in the posterior mediastinal region. Nevertheless, the question of whether this method yields superior surgical outcomes compared to traditional approaches remains unanswered. The current study aimed to assess the efficacy and safety of the secondary modified procedure. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-309/rc).
Methods
Clinical data and grouping
We conducted a retrospective analysis of 38 patients who underwent inflatable mediastinoscopy combined with laparoscopic radical esophagectomy for esophageal cancer at the Minimally Invasive Thoracic Surgical Center of the Second Affiliated Hospital of Naval Medical University between March 2020 and March 2023. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee board of Naval Medical University (No. 2023SL053) and informed consent was taken from all the patients. The inclusion criteria were defined as follows: (I) a preoperative diagnosis of resectable esophageal cancer; (II) the absence of severe cardiac, pulmonary, or cerebral disorders that would contraindicate surgery; and (III) no history of previous thoracic or abdominal surgeries. The patients were enrolled consecutively in the study. The patients were stratified into two groups based on the surgical procedures: Group A, which comprised 21 patients who underwent traditional mediastinoscopy combined with multi-port laparoscopy; and Group B, which comprised 17 patients who underwent a modified secondary mediastinoscopy combined with “SI + 1” laparoscopy. Data on surgical outcomes, including the operating time, blood loss, extent of lymph node dissection, and occurrence of postoperative complications were collected. Anastomotic leaks were diagnosed using the following criteria: (I) clinical manifestation: evident leakage of gastrointestinal contents into the wound; (II) radiological examination: upper gastrointestinal contrast studies or CT scans indicating leakage of contrast material outside the gastrointestinal tract into the wound, cervical or mediastinal tissue spaces.
Surgical procedure
Traditional mediastinoscopy combined with multi-port laparoscopic esophagectomy (Group A)
Cervical procedure
The patient underwent tracheal intubation with a single-lumen tube and was positioned supine. A 4-cm longitudinal incision was made on the anterior border of the left sternocleidomastoid muscle for the cervical procedure. The surgeon liberated the cervical esophagus, placed an incision protector, inserted a multiple-instrument access port, and then introduced CO2 gas. Exploration was conducted using a conventional 5-mm rigid endoscope (Rubina, Karl Storz, Germany). To free the esophagus, a single-arm mediastinal retractor (Kangji, Hangzhou, China) and a 44-cm LigaSure Maryland Divider (LF1944, Covidien, USA) were employed. Thus, the mobilization of esophagus was extended as far as possible down to the level of the lower pulmonary vein or diaphragmatic hiatus, and the subcarinal lymph nodes were dissected.
Abdominal procedure
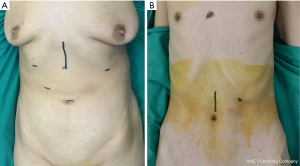
The patient was positioned head-up with a 30-degree tilt to the right side. The operation procedures from the abdomen and the neck were performed sequentially by a single surgeon. A 1-cm exploratory port was positioned on the right side of the umbilicus. The first auxiliary port (0.5 cm) was positioned 1 cm down the intersection of the right mid-clavicular line and the lower edge of the rib arch. The primary operation port (1.2 cm) was positioned at the midpoint between the umbilicus and the first auxiliary port. The second auxiliary port (0.5 cm) was placed 4 cm below the intersection point of the rib arch and left mid-clavicular line, while the third auxiliary port was positioned beneath the subxiphoid process using a 5-mm trocar (Figure 1). The procedure employed a Harmonic Scalpel (Ethicon, NJ, USA) or a Maryland Divider for the release of the greater curvature, followed by the lesser curvature. The left gastric artery was dissected using a vascular linear stapler, and the diaphragmatic hiatus was opened to allow for the dissection of lymph nodes in the lower mediastinum. A 5-cm incision was then made below the xiphoid process to facilitate the creation of the gastric conduit. Following the abdominal surgery, the gastric conduit was elevated to the neck through the thoracic cavity, and anastomosis was performed. Finally, routine jejunostomy was performed.
Secondary modified mediastinoscopy combined with “SI + 1” laparoscopic esophagectomy (Group B)
Cervical procedure
The patient was intubated using a single-lumen endotracheal tube and positioned supine. A 4-cm longitudinal incision was made along the anterior border of the left sternocleidomastoid muscle. Subsequently, the cervical esophagus was freed, and an incision protecter was inserted. Finally, the multiple-instrument access port was inserted (Figure 2A). Surgical exploration was conducted using a 5-mm Olympus flexible endoscope (ENDOEYE FLEX LTF-S190-5, Olympus, PA, USA; Figure 2B). CO2 gas was introduced. Ultra-long five-leaf forceps (Kangji, China; Figure 2C) and a 44-cm Maryland Divider were employed to free the esophagus as distally as possible, to the level of the lower pulmonary vein or the diaphragmatic hiatus. Additionally, the subcarinal lymph nodes were dissected.

Abdominal procedure
The patient was placed in a head-up position and tilted 30 degrees to the right side. A 5-cm incision was made above the umbilicus. A multiple-instrument access port was then inserted. An approximately 1-cm incision was made on the intersection of left mid-clavicular line and rib arch, serving as the auxiliary operating port (Figure 3). Using a Harmonic Scalpel or Maryland Divider, we first freed the greater curvature followed by the lesser curvature. The left gastric artery was dissected with a vascular linear stapler. Subsequently, we opened the diaphragmatic hiatus and dissected the lymph nodes of the inferior mediastinum. After releasing the stomach, we removed the multiple-instrument access port and created a gastric conduit through the single incision. The esophagogastric reconstruction and jejunostomy procedures were performed in the same manner as in Group A.

Statistical analysis
The primary outcome of this trial is defined as the successful mobilization of the esophagus to the level of the esophageal hiatus, which is a pivotal parameter in the context of mediastinoscopic esophagectomy. Based on our experience, the success rate using the traditional (primary modification) method is approximately 40%. With the innovation of instruments, the targeted success rate for the secondary modified procedure is 85%. The sample size was calculated using the SAS 9.4 (SAS Institute Inc., NC, USA) sample size calculation model. We employed a comparative study design, and adopted a 1:1 allocation ratio for the two groups. The significance level (α) was set at 0.05 for a two-sided test, with a test power (1−β) of 0.80. The variance estimation was performed using the normal approximation algorithm, resulting in a sample size of 17 per group.
The statistical analysis was conducted using SPSS 23.0 (IBM Corporation, NY, USA) software. The normally distributed continuous data are presented as the mean ± standard deviation. Group comparisons were performed using the t-test for two groups and an analysis of variance for multiple groups. If the overall variance was not uniform, a non-parametric test was applied. The categorical data are presented as the count and percentage, and group comparisons were performed using the chi-square test. Statistical significance was defined as a P value <0.05.
Results
Based on the surgical procedures performed, the patients were classified into two groups. Group A comprised 21 patients who underwent traditional mediastinoscopy combined with multi-port laparoscopy, while Group B comprised 17 patients who underwent a modified secondary mediastinoscopy combined with “SI + 1” laparoscopy. The patients had an average age of 67±7.2 years, and 24 were male and 14 were female. Preoperative gastroscopic pathology confirmed squamous carcinoma, with nine cases located in the upper thoracic region, 20 cases in the mid-thoracic region, and nine cases in the lower thoracic region. The clinical data for both groups are set out in Table 1.
Table 1
| Characteristics | Group A (n=21) | Group B (n=17) | P value |
|---|---|---|---|
| Age (years) | 65±7.3 | 68±7.0 | 0.26 |
| Sex, male | 14 (66.7) | 10 (58.8) | 0.62 |
| Smoking history | 5 (23.8) | 9 (52.9) | 0.06 |
| Drinking history | 8 (38.1) | 10 (58.8) | 0.20 |
| Malignant-tumors history | 3 (14.3) | 2 (11.8) | 0.82 |
| Concomitant diseases | |||
| Hypertension | 9 (42.9) | 5 (29.4) | 0.39 |
| Diabetes | 7 (33.3) | 4 (23.5) | 0.51 |
| BMI (kg/m2) | 21.2±2.4 | 20.6±2.4 | 0.44 |
| Tumor location | 0.28 | ||
| Upper | 5 (23.8) | 4 (23.5) | |
| Middle | 13 (61.9) | 7 (41.2) | |
| Lower | 3 (14.3) | 6 (35.3) | |
| ASA Physical Status Classification | 0.91 | ||
| I | 9 (42.9) | 8 (47.1) | |
| II | 10 (47.6) | 8 (47.1) | |
| III | 2 (9.5) | 1 (5.9) | |
| Neoadjuvant chemotherapy | 1 (4.8) | 1 (5.9) | 0.88 |
| Neoadjuvant radiation | 0 (0) | 0 (0) | >0.99 |
| Pathological type | 0.82 | ||
| SCC | 18 (85.7) | 15 (88.2) | |
| AC | 3 (14.3) | 2 (11.8) | |
| T | 0.55 | ||
| 1 | 14 (66.6) | 14 (82.4) | |
| 2 | 5 (23.8) | 3 (17.6) | |
| 3 | 1 (4.8) | 0 (0) | |
| 4 | 1 (4.8) | 0 (0) | |
| N | 0.70 | ||
| 0 | 18 (85.6) | 14 (82.3) | |
| 1 | 1 (4.8) | 1 (5.9) | |
| 2 | 1 (4.8) | 2 (11.8) | |
| 3 | 1 (4.8) | 0 (0) | |
| M | >0.99 | ||
| 0 | 21 (100.0) | 17 (100.0) | |
| 1 | 0 (0) | 0 (0) | |
| Pathological stage | 0.71 | ||
| I | 15 (71.4) | 12 (70.6) | |
| II | 4 (19.0) | 3 (17.6) | |
| III | 1 (4.8) | 2 (11.8) | |
| IV | 1 (4.8) | 0 (0) | |
| Residual tumor classification | 0.65 | ||
| R0 | 18 (85.7) | 15 (88.2) | |
| R1 | 2 (9.5) | 2 (11.8) | |
| R2 | 1 (4.8) | 0 (0) | |
| Length of stay (days) | 19.5±7.5 | 20.3±8.0 | 0.68 |
| 30-day complications | 5 (23.8) | 4 (23.5) | 0.98 |
Continuous data are presented as the mean ± standard deviation. Categorical data were expressed as counts and percentages. Group A: traditional mediastinoscopy combined with multi-port laparoscopy; Group B, modified secondary mediastinoscopy combined with “SI + 1” laparoscopy. AC, adenocarcinoma; ASA, American Society of Anesthesiologists; BMI, body mass index; SCC, squamous cell carcinoma; SI + 1, single-incision plus one-port.
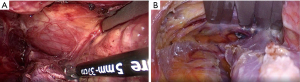
Inflatable mediastinoscopy combined with laparoscopic esophagectomy was successfully performed on all the patients, and conversion to thoracotomy was not required in any case. No mortality was recorded. There was no statistically significant difference in the operation time between the two groups (207±21 min for Group A, 209±15 min for Group B, P=0.75; see Table 2). In relation to the duration of abdominal surgery, the average surgical time for the laparoscopic procedure in the traditional multi-port group was 44 min, while that in the “SI + 1” group was 47 minutes. No statistically significant difference was observed between the two groups. The application of the flexible endoscope and the five-leaf forceps contributed to better mediastinal exposure in Group B (Figure 4). As a result, in Group A, the esophagus of nine patients was successfully mobilized to the level of the diaphragm (42.9%), while in Group B, this number increased to 15 patients (88.2%). A statistically significant difference was observed between the two groups (P=0.004). Intraoperative bleeding was measured at 15±6 mL in Group A and 14±5 mL in Group B, and there was no statistically significant difference between the two groups (P>0.05). The number of resected lymph nodes averaged 19±4 in Group A and 20±2 in Group B, and there was no statistically significant difference between the two groups (P>0.05).
Table 2
| Surgical outcomes | Group A (n=21) | Group B (n=17) | P value | OR (95% CI) |
|---|---|---|---|---|
| Operation time (min) | 207±21 | 209±15 | 0.75 | |
| Time for the laparoscopic procedure (min) | 44±5 | 47±6 | 0.09 | |
| Number of successful esophageal mobilizations to the level of the diaphragm | 9 (42.9) | 15 (88.2) | 0.004 | 10 (1.809–55.284) |
| Blood loss (mL) | 15±6 | 14±5 | 0.73 | |
| Number of resected lymph nodes | 19±4 | 20±2 | 0.20 | |
| Lymph node ratio (%) | 4±11 | 4±11 | 0.87 |
Continuous data are presented as the mean ± standard deviation. Categorical data were expressed as counts and percentages. Group A: traditional mediastinoscopy combined with multi-port laparoscopy; Group B, modified secondary mediastinoscopy combined with “SI + 1” laparoscopy. OR, odds ratio; CI, confidence interval; SI + 1, single-incision plus one-port.
Among the patients, four in Group A and two in Group B experienced postoperative recurrent laryngeal nerve paralysis. Notably, none of the patients developed postoperative lung infections or chylothorax. There were two cases of anastomotic leakage in Groups A and B, respectively (Table 3).
Table 3
| Postoperative complications | Group A (n=21) | Group B (n=17) | P value | OR (95% CI) |
|---|---|---|---|---|
| Recurrent laryngeal nerve paralysis | 4 (19.0) | 2 (11.8) | 0.54 | 0.567 (0.091–3.546) |
| Anastomotic leaks | 2 (9.5) | 2 (11.8) | 0.82 | 1.267 (0.159–10.074) |
| Pulmonary complications | 0 | 0 | ||
| Chylothorax | 0 | 0 | ||
| Anastomotic stenosis | 0 | 0 |
Categorical data were expressed as counts and percentages. Group A: traditional mediastinoscopy combined with multi-port laparoscopy; Group B, modified secondary mediastinoscopy combined with “SI + 1” laparoscopy. OR, odds ratio; CI, confidence interval; SI + 1, single-incision plus one-port.
Discussion
Minimally invasive techniques have now emerged as a primary modality for treating esophageal cancer, with the goal of achieving radical resection while minimizing postoperative complications (19). Currently, thoraco-laparoscopic esophagectomy is the predominant approach among the minimally invasive procedures. In recent years, there has been increasing discussion about the potential use of the inflatable mediastinoscopic approach as an option for esophagectomy (20,21). Mediastinoscopic esophagectomy does not require opening of the chest, repositioning or involvement of the lungs, has a shorter operative time, less blood loss, and less postoperative morbidity, while ensuring oncological safety and the reliability of lymph node dissection (22). This approach is particularly suitable for patients with severe pleural adhesion or those with poor respiratory function. In our previous research, we made a primary modification, mainly focusing on the cervical procedures. Building on these refinements, we are currently concentrating on optimizing the abdominal steps to further reduce patient trauma (14). As a result, we introduced the concepts of “field reduction” and “port reduction”, bringing about a transition from the traditional “three-field” (cervical, thoracic, and abdominal) surgical approach to a “two-field” (cervical and abdominal) modality. This modification reduces the traditional 11 ports required for cervical, thoracic, and abdominal surgery to four ports for cervical and abdominal surgery, thus further minimizing the surgical trauma. It is also observed that this modification significantly increases the success rate of esophageal mobilization to the esophageal hiatus from the neck and maintains the efficiency of lymph node dissection. Traditionally, due to inadequate instrumentation, the length of esophagus that could be mobilized downward from the neck was limited. This often necessitated completing the dissection of para-esophageal and subcarinal lymph nodes through an abdominal approach, which was comparatively difficult and less effective. Therefore, mobilizing the esophagus and performing lymph node dissection from the neck is considered an ideal approach. Techniques involved in our secondary modification simplify abdominal procedure, negates the need for difficult thoracic manipulation through abdominal approach, and potentially improves thoracic lymphadenectomy outcomes by offering better access and visibility, particularly overcoming the challenges associated with dissection from the carina to the lower pulmonary veins.
The first mediastinoscopic esophagectomy in Shanghai was performed in June 2017 at our hospital. Since then, we have introduced a primary modification. In this primary modification, the dissection of mediastinal lymph nodes, including the sub-carinal lymph nodes and those along the bilateral recurrent laryngeal nerves, was performed via the cervical approach. The esophagus was mobilized downward as far as the instruments could reach to reduce the difficulty of mobilizing the lower thoracic segment of the esophagus through the abdominal approach. In our secondary modification, the cervical procedure was performed in a similar manner to the primary modification. However, the secondary modification was primarily facilitated by the application of advanced surgical instruments. First, we replaced the original trocar made by a surgical glove with a multiple-instrument access port, which facilitated the surgical procedure. Notably, this multiple-instrument access port can also be used in single-port abdominal procedures, thereby saving costs. Second, we adopted Olympus’s 5-mm flexible endoscope (ENDOEYE FLEX LTF-S190-5), which is longer than the standard 5-mm rigid endoscope (Rubina, Karl Storz), and is flexible at the front end, providing a better field of view. This is particularly advantageous for lower mediastinal procedures and lymph node dissection. Third, we used ultra-long five-leaf forceps, which overcome the limitations of the traditional mediastinal retractor in lower mediastinal procedures. These forceps adequately expose the mediastinum and significantly increase the length of the mobilized esophagus from the cervical incision. Through their application, the mobilization of the esophagus in almost every case was able to be extended to the level of the diaphragm.
The use of single-incision thoracoscopic and laparoscopic techniques for esophagectomy was initially reported by scholars from Taiwan (23). However, there are currently no reports on the combined use of inflatable mediastinoscopy and single-incision laparoscopy for esophagectomy (24-26). We employed the “SI + 1” technique for gastric mobilization, and found that there was no significant difference in the operating time compared to that of the traditional multi-port technique and achieved adequate dissection of the lymph nodes. Compared with the traditional subxiphoid incision, which is extended following the laparoscopic procedure, the single incision made on the umbilicus did not impede the process of gastric mobilization. Additionally, this incision facilitated the creation of the gastric conduit and jejunostomy. Importantly, it is more convenient to create a jejunostomy through the umbilical incision than through the traditional subxiphoid incision. The additional “plus one port” (+1) on the left abdomen was employed to dissect the splenogastric ligament and served as the exit for jejunostomy tube. The incorporation of this “+1” port effectively reduces the overall complexity and operating time of the single-incision laparoscopic procedure. Through these modifications, the standard “11 ports in 3 fields” surgical approach could be streamlined into a more efficient “4 ports in 2 fields” technique.
This study had certain limitations. First, it was a single-center retrospective study with a relatively small sample size, which might have introduced selection bias in the case selection. It appears that way for 90% of the patients were stages I and II, 70% were stage I. 90% of the patients ASA was 1 and 2. Second, the present investigation focused on the short-term outcomes of mediastinoscopic esophagectomy, such as surgical outcomes and postoperative complications, and a longer-term follow-up of the surgical prognosis was lacking. Based on our previously published research, mediastinoscopic esophagectomy appears to yield similar clinical outcomes to traditional three-field surgery (14). In the current study, the lymph node dissection outcomes of the secondary modification group were comparable to those of the primary modification group, while the secondary modification method achieved improved exposure in the mediastinal field. This may provide some advantages to the conduct of this operation, and potentially improve short-term post-operative outcomes. However, due to the relatively short follow-up period, further research is required to gather additional post-operative data and relative outcomes.
Conclusions
In conclusion, the combined use of inflatable mediastinoscopy and the “SI + 1” laparoscopic approach for the treatment of esophageal cancer is both safe and effective. The use of a 5-mm flexible endoscope, ultra-long five-leaf forceps, and LigaSureTM Maryland forceps simplifies the process of mobilizing the esophagus through the cervical incision and dissecting the mediastinal lymph nodes. This refinement enhances the mediastinoscopic esophagectomy techniques, offering an improved method that could support the broader implementation of inflatable mediastinoscopic esophageal surgery.
Acknowledgments
Funding: This study received funding from
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-309/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-309/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-309/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-309/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee board of Naval Medical University (No. 2023SL053) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Morgan E, Soerjomataram I, Rumgay H, et al. The Global Landscape of Esophageal Squamous Cell Carcinoma and Esophageal Adenocarcinoma Incidence and Mortality in 2020 and Projections to 2040: New Estimates From GLOBOCAN 2020. Gastroenterology 2022;163:649-58.e2. [Crossref] [PubMed]
- Domper Arnal MJ, Ferrández Arenas Á, Lanas Arbeloa Á. Esophageal cancer: Risk factors, screening and endoscopic treatment in Western and Eastern countries. World J Gastroenterol 2015;21:7933-43. [Crossref] [PubMed]
- He F, Wang J, Liu L, et al. Esophageal cancer: trends in incidence and mortality in China from 2005 to 2015. Cancer Med 2021;10:1839-47. [Crossref] [PubMed]
- Zhu H, Ma X, Ye T, et al. Esophageal cancer in China: Practice and research in the new era. Int J Cancer 2023;152:1741-51. [Crossref] [PubMed]
- Waters JK, Reznik SI. Update on Management of Squamous Cell Esophageal Cancer. Curr Oncol Rep 2022;24:375-85. [Crossref] [PubMed]
- Kitagawa Y, Ishihara R, Ishikawa H, et al. Esophageal cancer practice guidelines 2022 edited by the Japan esophageal society: part 1. Esophagus 2023;20:343-72.
- McKeown KC. Trends in oesophageal resection for carcinoma with special reference to total oesophagectomy. Ann R Coll Surg Engl 1972;51:213-39. [PubMed]
- Royston CM, Dowling BL. A combined synchronous technique for the McKeown three-phase oesophagectomy. Br J Surg 1976;63:122-4. [Crossref] [PubMed]
- Lehenbauer D, Kernstine KH. Robotic esophagectomy: modified McKeown approach. Thorac Surg Clin 2014;24:203-9. vii. [Crossref] [PubMed]
- Zhang Z, Rong B, Guo M. Uniportal Thoracoscopic McKeown Esophagectomy. Indian J Surg 2020;82:669-71. [Crossref] [PubMed]
- Till BM, Grenda TR, Okusanya OT, et al. Robotic Minimally Invasive Esophagectomy. Thorac Surg Clin 2023;33:81-8. [Crossref] [PubMed]
- Ikeda Y, Niimi M, Kan S, et al. Mediastinoscopic esophagectomy using carbon dioxide insufflation via the neck approach. Surgery 2001;129:504-6. [Crossref] [PubMed]
- Li GS. Prof. Qingdong Cao: single-port inflatable mediastinoscopy combined with laparoscopy for the radical treatment of esophageal cancer. J Thorac Dis 2016;8:E1108-9. [Crossref] [PubMed]
- Chen Z, Huang K, Wei R, et al. Transcervical inflatable mediastinoscopic esophagectomy versus thoracoscopic esophagectomy for local early- and intermediate-stage esophageal squamous cell carcinoma: A propensity score-matched analysis. J Surg Oncol 2022;125:839-46. [Crossref] [PubMed]
- Liu C, Chen Z, Wei R, et al. Intra-operative events and countermeasures during esophagectomy via transcervical incision inflatable single-port mediastinoscope combined with laparoscopy. J Thorac Dis 2021;13:133-9. [Crossref] [PubMed]
- Dabsha A, Elkharbotly I, Rahouma M. ASO Author Reflections: Mediastinoscope-Assisted Esophagectomy: An Innovative Minimally Invasive Technique for Esophageal Resection. Ann Surg Oncol 2023;30:4040-1. [Crossref] [PubMed]
- Song S, Shen C, Hu Y, et al. Application of Inflatable Video-Assisted Mediastinoscopic Transhiatal Esophagectomy in Individualized Treatment of Esophageal Cancer. Biomedicines 2023;11:2750. [Crossref] [PubMed]
- Wu M, Wang G, Sun X, et al. Inflatable Video-Assisted Mediastinoscopic Transhiatal Esophagectomy: A Learning Curve Study. J Gastrointest Surg 2023;27:2589-91. [Crossref] [PubMed]
- van der Sluis PC, Schizas D, Liakakos T, et al. Minimally Invasive Esophagectomy. Dig Surg 2020;37:93-100. [Crossref] [PubMed]
- Fujiwara H, Shiozaki A, Konishi H, et al. Perioperative outcomes of single-port mediastinoscope-assisted transhiatal esophagectomy for thoracic esophageal cancer. Dis Esophagus 2017;30:1-8. [Crossref] [PubMed]
- Fujiwara H, Shiozaki A, Konishi H, et al. Mediastinoscope and laparoscope-assisted esophagectomy. J Vis Surg 2016;2:125. [Crossref] [PubMed]
- Dabsha A, Elkharbotly I, Yaghmour M, et al. Novel Mediastinoscope-Assisted Minimally Invasive Esophagectomy for Esophageal Cancer: A Systematic Review and Meta-analysis. Ann Surg Oncol 2023;30:4030-9. [Crossref] [PubMed]
- Lee JM, Chen SC, Yang SM, et al. Comparison of single- and multi-incision minimally invasive esophagectomy (MIE) for treating esophageal cancer: a propensity-matched study. Surg Endosc 2017;31:2925-31. [Crossref] [PubMed]
- Hirano Y, Hattori M, Douden K, et al. Single-incision plus one port laparoscopic anterior resection for rectal cancer as a reduced port surgery. Scand J Surg 2012;101:283-6. [Crossref] [PubMed]
- Xin N, Wei R, Huang K, et al. Comparative study on short-term efficacy of single incision plus one (SI+1) port and multiportal 3D laparoscopic minimally invasive esophagectomy. J Gastrointest Oncol 2021;12:1277-84. [Crossref] [PubMed]
- Seo JW, Park KB, Chin HM, et al. Is single incision laparoscopic surgery (SILS) for gastric gastrointestinal stromal tumor (GIST) dependent on the location of the tumor? BMC Surg 2023;23:247. [Crossref] [PubMed]


