Clinical statistics analysis on the characteristics of pneumoconiosis of Chinese miner population
Introduction
Pneumoconiosis is one of the most common diseases in the miners, which is characterized by the progressive and irreversible pathologic features. The main cause of this disease is the excessive inhalation of dust in working process, which can lead to repeated inflammation, progressive pulmonary fibrosis, reducing the patients’ survival time, lung function failure and eventually cause death (1).
Epidemiological investigation on the global lung diseases showed that the prevalence of pneumoconiosis ranked the top of occupational lung diseases, especially in developing countries, where this phenomenon is more serious (2). Chinese is one of populations exposed to dust most widely with the highest prevalence of pneumoconiosis every year (3,4). According to the reports of 2014 National Occupational Disease published by National Health and Family Planning Commission (NHFPC) of the People’s Republic of China, there were 29,972 new cases of occupational lung diseases diagnosed in 2014, 90% of which was pneumoconiosis, namely 26,873 cases. When classified by types of jobs, coal mining, washing industry and non-ferrous metal mining industry were ranked the top three with 11,396 cases, 2,935 cases and 4,408 cases, respectively, accounting for 62.52% of all new diseases (5). The direct economic loss for the country reached 8 billion per year, and the indirect economic losses even reached 20 billion (6,7).
However, the pneumoconiosis is still not curable as there is no effective treatment or control drug to slow down the disease progression. Currently the most effective way to retard the disease is prevention. Studies have shown that reducing the worker’s daily breathing concentration of dust can effectively reduce the chance of suffering from pneumoconiosis (8,9). According to the rules of American Conference of Governmental Industrial Hygienists (ACGIH), they defined the dangerous levels of work conditions by a clear principle on working hours and dust concentration. And more specifically, the dangerous levels were different from each type of dust because the maximum allowable levels were different (10,11). The methods currently applied to control the concentration of dust are: technological innovation, wet field operations, ventilation dust, individual protective equipment, occupational health management, health education, monitoring and inspection (12).
With the rapid development of economy and industry, and the insufficient protection of the environment, there are more than 6 million underground mining workers under the threat of Pneumoconiosis in China (13). So the financial burden for initiating preventive efforts is extremely serious (14). Therefore, it is very essential to learn the basic condition of pneumoconiosis patients, effectively find out the characteristics of Chinese miners’ pneumoconiosis, and develop effective treatment strategies to prevent and control this illness.
In this study, we have collected patient information of 118 clinical cases from the Taihe Hospital. We analyzed the clinical data of pneumoconiosis patients by using the statistical methods of the Chi-square test, the multilayer Chi-square test and the risk ratio (RR) test, and identified the characteristics of this disease to develop useful prevention and treatment strategies for the clinical patient care.
Methods
Basic subjects
According to the diagnostic criteria of pneumoconiosis (15,16), 118 pneumoconiosis patients (117 males and 1 female) from Taihe Hospital were retrospective analyzed since 2010, and 50 (42.4%) of coal miners, 19 (16.1%) of gold miners, 12 (10.2%) of mixer of both and 37 (31.4%) of other miners were included. According to lung imaging diagnosis of pneumoconiosis patients (16), there were 18 (15.3%) patients in stage I, 83 (70.3%) in stage II, and 17 (14.4%) in stage III, who were diagnosed when first admitted to Taihe hospital. We also classified these patients into different groups: groups according to age, <50 years old of 83 (70.3%) and >50 years old of 35 (29.7%); groups according to smoking history, 55 (46.6%) of smokers and non-smokers of 63 (53.4%). In addition, they were divided by dust exposure time: 16 (13.6%) <3 years, 17 (14.4%) between 3–5 years, 41 (34.7%) between 5–10 years, and 44 (37.3%) >10 years. Among them, except one patient without any treatment, 15 (12.7%) of these patients were treated with drugs specifically used for pneumoconiosis, 22 (18.6%) of them were subjected to lung lavage therapy, and combination of both treatments applied to other 80 (67.8%) patients. The study protocol was approved by the Department of ethnics committee, Shiyan Taihe Hospital (ID: 2016001-1) and was conducted in accordance with the Helsinki Declaration of 1964 (revised 2008).
Observation subjects
To learn the pathological characteristics of pneumoconiosis, manifold investigation and observation were included in this study: overall survival (OS), Activities of Daily living (ADLs, a term used in healthcare refer to people’s daily self-care activities, which was classified into two phases in this research: living independently and living with help) (17), smoking history, syndromes including concurrent tuberculosis, concurrent hemoptysis, pneumothorax and Broncho-pulmonary infection cases. Patients signed an informed consent, and their other personal information will not be published to protect patient privacy.
Diagnostic criteria
According to the China National pneumoconiosis diagnostic criteria, pneumoconiosis patients should have dust exposure history records and appropriate chest X-ray examination (18).
Statistical analysis
Because the diagnosis time could not correspond to the real disease time, the initial exposure time to dust was used as a statistical target. All the statistical analysis procedures were performed by using SPSS 22.0 (SPSS Institute, Inc., Chicago, IL, USA). Differences between different groups of patients were accessed by using Chi-square tests assuming variances. In addition, a further analysis was performed by the multilayer Chi-square test to confirm the conditional independence with the Breslow-Day value. P values of less than 0.05 (2 tailed) are considered significantly different (19,20). Finally, the risk assessment of patients was predicted by using the RR test, and it is considered statistical significance as the ratio deviated from 1, more deviation and more difference.
Results
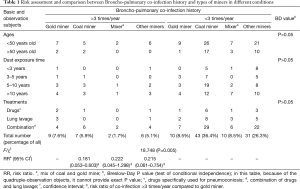
We compared types of miners with different syndromes including concurrent tuberculosis, concurrent hemoptysis, pneumothorax and Broncho-pulmonary infection by using Chi-square tests, and we found that gold miners are liable to cause Broncho-pulmonary co-infection with Chi-square value 18.748 and the P value <0.001 (Table 1). Moreover, a further risk assessment predicted that the risk of gold miners suffered from Broncho-pulmonary co-infection was almost 5 times more than other types of miners (Table 1). In addition, we compared various types of miners with Broncho-pulmonary co-infection in different conditions of multiple factors, including ages, dust exposure time and therapeutic methods by using multilayer Chi-square test, which showed no statistical significance with P>0.05 (Table 1).
Full table
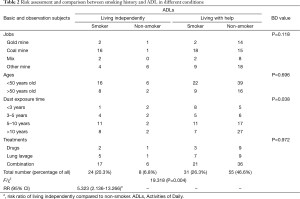
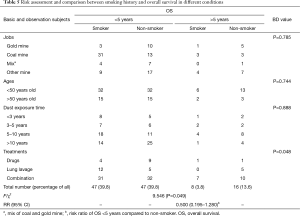
Because of its specificity, smoking has been one of the key elements of clinical concern in lung diseases. Statistical analysis exhibited that lung functions of smokers declined faster with the increasing smoking years compared to the non-smokers (21,22). Due to excessive dust exposure, progressive pulmonary fibrosis and pulmonary failure are easily appeared in miner patients following pathological changes. To determine whether smoking could worsen pneumoconiosis of miners, we analyzed the clinical data of smoking history and their ADLs. However, unexpectedly, the smoking miners displayed a better ADLs compared to non-smokers, which showed 19.318 of Chi-square score and less than 0.001 of P value (Table 2). About 20.3% (24/118) of smokers lived independently compared to 6.8% (8/118) of non-smoking miners, which showed significantly different by using Chi-square tests. Moreover, the risk assessment exhibited non-smokers had 5 times more risk with worse ADLs compared to smokers (Table 2). We found that this connection was associated with the dust exposure time with P<0.05, analyzed by a further multilayer Chi-square test in various conditions, including jobs, ages, dust exposure time and treatments (Table 2). An additional risk assessment indicates that the increasing risk of non-smoking miners occurred as the increasing time exposed to dust (Table 3). The RR value was rising sharply year by year, which was up to 15.429 after exposing to dust more than 10 years, whereas it was only 0.313 when exposure time was less than 3 years.
Full table

Full table
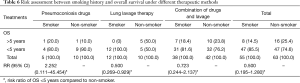
Next, we studied the connection between smoking history and other co-infection diseases, including concurrent tuberculosis, concurrent hemoptysis, pneumothorax and Broncho-pulmonary infection. As a result, our analysis indicates that the probability of smoking miners suffered from Broncho-pulmonary co-infection was less than non-smoking miners with Chi-square value 8.044 and P<0.01 (Table 4). About 16.1% (19/118) of smoking miners co-infected with Broncho-pulmonary, showing a significantly different compared to 4.2% (5/118) of non-smokers, which was not related with other factors, such as jobs, ages and treatments (Table 4). A further risk assessment revealed that the RR of smoking patients suffered from Broncho-pulmonary co-infection was 0.232 times of non-smokers, which indicated that non-smokers may be susceptible to this co-infection. However, this result is quite different from the common sense that smoking and dust exposure can increase the probability of lung infection. Therefore, we further analyzed the conditions independence on this result by using multilayer Chi-square test, as dust exposure time played a critical role in the relationship between ADLs and smoking history (Tables 2,3). Although, there was no statistical significance on the condition of different dust exposure time, the trend still showed that with the increasing dust time, the non-smokers would have more probability to get Broncho-pulmonary co-infection (data not shown).

Full table
Finally, expectedly, smoking history exhibited a deteriorating effect to OS with 9.546 of Chi-square value and P<0.05 (Table 5), comparing 3.8% of smoking patients with 13.6% of non-smokers when OS time was more than 5 years. Moreover, the RR indicated that the non-smokers had 2 times of probability to reach more than 5 years of OS compared to smokers (Table 5). Further multilayer Chi-square tests revealed that the link between smoking history and OS was associated with therapeutic methods (Table 5). An additional risk assessment showed that pneumoconiosis drugs were more beneficial to the smokers for extending OS with RR of 2.252 (Table 6), implying that these drugs may have side effects to non-smokers and the drugs therapy may be not appropriate to them. Conversely, lung lavage therapy was better to non-smokers with RR of 0.500 (Table 6). Therefore, these results suggested that the patients with the smoking history should select pneumoconiosis drugs therapy alone, and non-smokers should choose lung lavage therapy alone.
Full table
Full table
Discussion
In 1987, China enacted and implemented a principle entitled “Pneumoconiosis disease prevention and disease control of the People’s Republic of China”, and in 2001 another principle was promulgated: “Occupational disease prevention and control of the People’s Republic of China” (23). Although the laws permit the acceptable dust concentration of 1 mg/m3 and provide the methods to reduce dust concentration, the prevalence of pneumoconiosis in China has not yet significantly reduced due to the rapid economic and industrial development. Therefore, understanding of the characteristics of pneumoconiosis is particularly critical to effectively control the progress of the pneumoconiosis. Here we compared and analyzed the clinical data of 118 pneumoconiosis cases from the Taihe Hospital, which included all kinds of patients with different treatment options, co-infection history, age, dust exposure times, smoking history, working condition and ADLs.
Compared to other types of miners, gold miners are liable to cause Broncho-pulmonary co-infection (Table 1). Therefore, it is important to strictly control the dust concentration especially in the gold mine area, build and raise self-protection awareness of miners, and increase the chances of physical examination, which will be helpful to lower the morbidity of pneumoconiosis as well as medical expenses. In traditional Chinese medicine science, the pneumoconiosis is considered as a type of chronic diseases, and the dust as a dryness factor could block the main and collateral channels of lung, ultimately leading to the Qi and Yin deficiency in the body. Consequently, to investigate the treatment of Chinese medicine will be beneficial to invigorate the primordial Qi and Yin and improve physical health, such as Bu Zhong Yi Qi formula, Sha Shen Mai Dong formula (24) and tetrandrine (25).
Smoking is one of the common factors leading to pneumonia. The relationship between pneumoconiosis and smoking history could be a critical factor affecting the medical advice and treatments (26). Unexpectedly (27), our analytical data indicated that there was a negative correlativity between smoking history and Broncho-pulmonary co-infection, which showed that the probability of smoking miners suffered from Broncho-pulmonary co-infection was less than non-smoking miners (Table 4) which was concerned with the dust exposure time factor. Moreover, if the dust exposure time was less than 3 years, non-smokers kept better ADLs than the smoking miners. Reversely, as the increasing time exposed to dust, there was an increasing risk of non-smoking miners (Table 3). Unfortunately, the smoking miners’ OS was still shorter than non-smokers (Table 5), in accordance with smoking reducing life time (28). Interestingly, pneumoconiosis drugs could only extend the smokers’ OS, but not the non-smoking miners’ (Table 6). One possibility is that these drugs could relieve the lung failure due to smoking and have side effects on non-smokers. Therefore, compared to these different treatments, we recommended that the patients with the smoking history should select pneumoconiosis drugs therapy alone, and non-smoking patients should choose lung lavage therapy alone without pneumoconiosis drugs.
In conclusion, the smoking history and dust exposure time play important roles in the progression of pneumoconiosis. However, the stage of disease as another factor need to be excluded if we want to confirm this conclusion. Co-infections often happened in stage III of pneumoconiosis, but the most patients admitted to the hospital were in stage II. Hence, we need to collect more stage III patients and observe their condition. Moreover, we will further focus on finding out the biological factors that may change the possibility of co-infection ratio in the different dust exposure time.
To date, there is no available treatment for pneumoconiosis provided by any institution or randomized controlled trail (RCT). The research on this disease is almost about the prevalence, risk assessment and clinical experiments. Dr. Wang chose six different Chinese medicine formulas to treat the pneumoconiosis, and observed the patients relief from the symptoms (24). Dr. Tao divided pneumoconiosis into four syndromes and gave different formulas. The two results above suggested that their therapies had efficacy, however, their experiments did not use randomized control method and not evaluated by statistical analysis. More probable, it is essential to set up a pneumoconiosis clinical research criterion to further study and treat this disease.
Here we found the fundamental properties of pneumoconiosis, but we still have a long way to go to prevent and control this disease, and the discovery of effective drugs and other efficient treatments appear especially important. Patients of stage II were dominated in this retrospective study, so further validation analyzes with more populations of other stages are needed to confirm our findings. In addition, more mechanism and functional study is needed to promote drugs development in the future.
Acknowledgements
Funding: This work was supported by Macau Science (021/2013/A1), Technology Development Found (005/2014/AMJ), National Natural Science Foundation of China (81270092), Educational Commission of Hubei Province of China (D20152104) and Science and technology Program of Shiyan, China (15Y20).
Footnote
Conflicts of Interest: The authors have no conflict of interest to declare.
Ethical Statement: The study protocol was approved by the Department of ethnics committee, Shiyan Taihe Hospital (ID: 2016001-1) and was conducted in accordance with the Helsinki Declaration of 1964 (revised 2008). Patients signed an informed consent, and their other personal information will not be published to protect patient privacy.
References
- Chen W, Liu Y, Wang H, et al. Long-term exposure to silica dust and risk of total and cause-specific mortality in Chinese workers: a cohort study. PLoS Med 2012;9:e1001206. [Crossref] [PubMed]
- Pingle S. Occupational safety and health in India: now and the future. Ind Health 2012;50:167-71. [Crossref] [PubMed]
- Antao VC, Petsonk EL, Sokolow LZ, et al. Rapidly progressive coal workers' pneumoconiosis in the United States: geographic clustering and other factors. Occup Environ Med 2005;62:670-4. [Crossref] [PubMed]
- Han L, Han R, Ji X, et al. Prevalence Characteristics of Coal Workers' Pneumoconiosis (CWP) in a State-Owned Mine in Eastern China. Int J Environ Res Public Health 2015;12:7856-67. [Crossref] [PubMed]
- China NHaFPCotPsRo. The National Occupational Disease Report of 2014. Ministry of Land and Resources of the People's Republic of China; 8, DEC, 2015. Available online: http://www.mlr.gov.cn/xwdt/jrxw/201512/t20151208_1390898.htm
- Shi ZC. Whole lung lavage for treatment of pneumoconiosis. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2010;28:481. [PubMed]
- Xia Y, Liu J, Shi T, et al. Prevalence of pneumoconiosis in Hubei, China from 2008 to 2013. Int J Environ Res Public Health 2014;11:8612-21. [Crossref] [PubMed]
- Shen F, Yuan J, Sun Z, et al. Risk identification and prediction of coal workers' pneumoconiosis in Kailuan Colliery Group in China: a historical cohort study. PLoS One 2013;8:e82181. [Crossref] [PubMed]
- Petsonk EL, Rose C, Cohen R. Coal mine dust lung disease. New lessons from old exposure. Am J Respir Crit Care Med 2013;187:1178-85. [Crossref] [PubMed]
- Torres Rey CH, Ibañez Pinilla M, Briceño Ayala L, et al. Underground coal mining: relationship between coal dust levels and pneumoconiosis, in two regions of Colombia, 2014. Biomed Res Int 2015;2015:647878.
- Guan HY, Zhang H, Su LP, et al. The study of the characteristics and influencing factors of pneumoconiosis among workers exposed to dusts in an iron mine. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2012;30:36-40. [PubMed]
- Shen F, Liu H, Yuan J, et al. Cost-Effectiveness of coal workers' pneumoconiosis prevention based on its predicted incidence within the Datong Coal Mine Group in China. PLoS One 2015;10:e0130958. [Crossref] [PubMed]
- Zhang M, Wang D, Zheng YD, et al. Analyses on the characteristics and the trends of pneumoconiosis notified between 1997 and 2009, in China. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2013;31:321-34. [PubMed]
- Liang Y, Xiang Q. Occupational health services in PR China. Toxicology 2004;198:45-54. [Crossref] [PubMed]
- Yu P, Xu H, Zhu Y, et al. An automatic computer-aided detection scheme for pneumoconiosis on digital chest radiographs. J Digit Imaging 2011;24:382-93. [Crossref] [PubMed]
- Guidelines for the use of the ILO International Classification of Radiographs of pneumoconioses, Revised edition 2011. In: Office GSIL, editor. Occupational Safety and Health Series, No 22 (Rev. 2011). 17 November 2011.
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179-86. [Crossref] [PubMed]
- Ding Q, Schenk L, Hansson SO. Occupational diseases in the people's Republic of China between 2000 and 2010. Am J Ind Med 2013;56:1423-32. [Crossref] [PubMed]
- Kuo HW, Chang CL, Lai JS, et al. Prevalence of and factors related to pneumoconiosis among foundry workers in central Taiwan. Sci Total Environ 1998;222:133-9. [Crossref] [PubMed]
- Wang M, Wang S, Song Z, et al. Associations of IL-4, IL-4R, and IL-13 gene polymorphisms in coal workers' pneumoconiosis in China: a case-control study. PLoS One 2011;6:e22624. [Crossref] [PubMed]
- Popović-Grle S, Pavicić F, Bicanić V. The effect of cigarette smoking on pulmonary diffusing capacity in asymptomatic smokers. Lijec Vjesn 1992;114:118-21. [PubMed]
- Omori H, Morimoto Y. Effects of smoking habits on pulmonary function. Cross-sectional and longitudinal studies in male subjects on medical check-up. Nihon Kokyuki Gakkai Zasshi. 2004;42:306-12. [PubMed]
- Mo J, Wang L, Au W, et al. Prevalence of coal workers' pneumoconiosis in China: a systematic analysis of 2001-2011 studies. Int J Hyg Environ Health 2014;217:46-51. [Crossref] [PubMed]
- Wang J, Jin L, Wang Z. Traditional Chinese Medicine discriminate treatment pneumoconiosis: analysis of 188 cases. China Foreign Medical Treatment 2008;27:3, 21.
- Liu C, Gong X, Xiao X, et al. Effects of tetrandrine combined with large volume whole lung lavage on the quality of life and oxidative stress of pneumoconiosis patients. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2014;32:219-21. [PubMed]
- Halldin CN, Reed WR, Joy GJ, et al. Debilitating lung disease among surface coal miners with no underground mining tenure. J Occup Environ Med 2015;57:62-7. [Crossref] [PubMed]
- Stämpfli MR, Anderson GP. How cigarette smoke skews immune responses to promote infection, lung disease and cancer. Nat Rev Immunol 2009;9:377-84. [Crossref] [PubMed]
- Crothers K, Griffith TA, McGinnis KA, et al. The impact of cigarette smoking on mortality, quality of life, and comorbid illness among HIV-positive veterans. J Gen Intern Med 2005;20:1142-5. [Crossref] [PubMed]


