Lung cancer resection with concurrent off-pump coronary artery bypasses: safety and efficiency
Introduction
Coronary heart disease (CHD) and lung cancer are among the leading causes of death in China (1,2). In clinical practice, the incidence of patients having both diseases has markedly increased in the past 20 years. It has been reported that approximately 10% of lung cancer patients also had symptoms of CHD (3). Treating patients with lung tumors and concurrent severe CHD is a challenge for thoracic surgeons because these patients face great cardiac risk if pulmonary resection is done without myocardial revascularization. Performing both of these procedures during a single operation may eliminate associated delay in lung cancer treatment (4). Previously, surgeons avoided performing heart and lung surgery simultaneously because of the risk of excessive bleeding associated with cardiopulmonary bypass (CPB) with heparinization. The reoperation rate for these combined procedures was nearly 10%. The 5-year survival rate after concomitant cardiac and lung cancer surgery was also much less than expected (5). In last decade, off-pump coronary artery bypass (OPCAB) grafting has become more popular in clinical practice. Recently, several publications have indicated that a combined OPCAB and lung resection may be feasible (6-9). However, the results of this procedure were only reported in a limited number of patients. Beginning in 2003 we began to evaluate new techniques to improve this combined operation, including thoracoscopy. We present our findings from these cases of patients who underwent combined cardiothoracic procedures in our hospital.
Methods
Between 2003 and 2014, 34 patients underwent simultaneous OPCAB and lobectomy in the Departments of Cardiac Surgery and Thoracic Surgery at the Beijing Anzhen Hospital, Capital Medical University. Patients were considered for inclusion if they had severe CHD diagnosed through angiocardiography and resectable lung cancer. This study was conducted in accordance with the Helsinki declaration and with approval from the Ethics Committee of Beijing Anzhen Hospital. Written informed consent was obtained from all participants.
Patient demographics
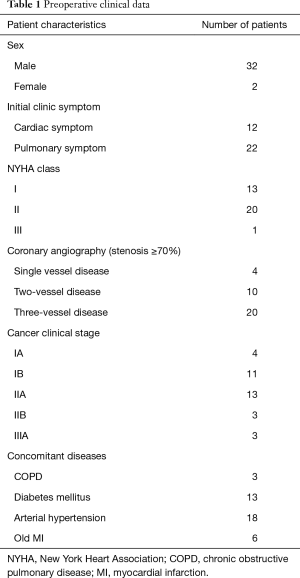
A total of 32 males and 2 females were included in this study. Mean age was 65.8±6.7 years (range, 54–77 years). Twenty-two patients were referred to our service after presenting with initial symptoms of pulmonary disease. Aside from physical examination and blood chemistries, routing evaluation of lung cancer included computed tomography (CT), fiberoptic bronchoscopy or CT-guided transthoracic needle biopsy, abdominal CT or ultrasonography, pulmonary function testing, brain CT or magnetic resonance imaging (MRI), bone scan, positron emission tomography-computed tomography (PET-CT) if necessary, 12-lead electrocardiogram (ECG), and echocardiography if patients had a history of high blood pressure and hyperlipidemia or aged more than 50 years old. In cases with questionable ischemia heart disease, catheterization of the coronary artery was performed. Only lung cancer patients with at least 70% narrowing in at least one coronary artery were recruited into this study. The remaining 12 patients had initial symptoms of CHD, were admitted to our cardiovascular medicine department, and lung nodules were later found by routine chest X-ray or CT during preoperative evaluation for OPCAB. Six of these patients had a history of myocardial infarction (MI). Clinical lung cancer staging was based on pathologic findings, chest CT, or results of PET, and most patients had stage I or stage II disease (TNM staging system in accordance with the New International System for Staging Lung Cancer). The majority of the patients had two- or three-vessel disease with class I or class II cardiac function (New York Heart Association, NYHA). The most common concomitant diseases were arterial hypertension, diabetes, and chronic obstructive pulmonary disease (COPD). A summary of the preoperative clinical data is presented in Table 1.
Full table
Surgical procedure
Combined thoracic and cardiac surgery was performed with myocardial revascularization carried out first. For some patients, the partial lung resection or biopsy was performed through a median sternotomy before the cardiac procedure by wedge lung resection or fine needle puncture if the diagnosis of the lung nodule was not ascertained. If this biopsy was found to be negative, the patient was excluded from this study. Lobectomy was then performed through either the initial incision or a secondary incision.
Specifically, following the biopsy in some lung cancer patients, coronary artery revascularization was carried out through a sternotomy approach. An Octopus system (Medtronic, Inc.) was used for cardiac stabilization. In most cases, the left internal thoracic artery (LITA) was used to bypass the left anterior descending artery (LAD). Saphenous vein bypass grafts were used to revascularize the other coronary arteries. Lobectomies were then performed with or without the assistance of thoracoscope. Branches of the pulmonary vein, pulmonary artery, and bronchial division were dissected separately and ligated or stapled (Auto Suture Co.). Then lymph nodes of hilus and mediastinal were dissected and pleural chest tubes and mediastinal drains were positioned (6). In the early combined cases, cardiac and lung procedures were performed through two separate incisions (sternotomy and thoracotomy). A lateral thoracotomy or muscle-sparing incision was used for standard lung resection and dissection of the lymphnodes. Patient position was changed from supine to lateral decubitus after the cardiac procedure. In the more recent cases, two incisions were only required for complicated tumor resections. Most lobectomies in this series were performed through sternotomy with assistance of the thoracoscope. The thoracoscope and video-assisted throacoscopic surgery (VATS) instruments were used mainly for mediastinal lymphadenectomy through two separate small incisions at the fourth and seventh intercostal spaces near the midaxillary line (7-10). Single thoracotomy was only used for patients with single vessel disease where the long nodule was on the same side, such as LAD disease with left lung cancer or right coronary artery (RCA) narrowing with right lung malignancy.
Postoperative follow-up
Patients had scheduled follow-up visits 30 days, 3 months, and 6 months postoperatively, and then every 6 months until the second postoperative year. Then the follow-up visits were performed every year. The first follow-up visit included EKG and antero-posterior and lateral chest X-rays. The follow-up visits at 3 and 6 months postoperative included EKG, echocardiography, abdominal ultrasound, and chest CT. Thereafter, follow-up visits also included bone scans and brain MRI.
Statistical analysis
Statistical analyses were performed using SPSS 13.0. Parameters related to postoperative outcome are displayed using descriptive statistics. Survival curves are drawn using the Kaplan-Meier method.
Results
Postoperative outcome
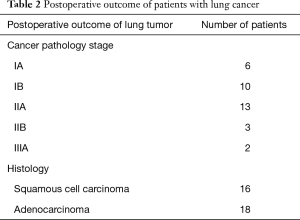
In total, 34 patients with non-small cell lung cancer were included in this study (Table 2). All the patients survived the operation and there were no deaths or new incidences of MIs observed during the perioperative period. Mean operative time 294.8±64.3 minutes. The mean hospital stay was 17.4±6.8 days.
Full table
Thirty-three patients were extubated on the second postoperative day. No patients required mechanical circulatory support. Two patients developed lung infections and one of them developed respiratory failure that required prolonged mechanical ventilation through tracheal tube by tracheotomy. Three patients needed several bronchoscopic aspirations for development of atelectasis. Five patients developed cardiac arrhythmias, including atrial fibrillation in three and ventricular ectopic beats in two patients. All 5 of these patients recovered after receiving intravenous infusions of amiodarone at 5 μg∙kg−1∙min−1. No perioperative or postoperative MIs were observed via ECG or elevation of serum myocardial enzymes. All patients were given infusions of dopamine (3–5 μg∙kg−1∙min−1) and nitroglycerin (2–5 μg∙kg−1∙min−1) until the third postoperative day. In most cases, oral aspirin was administered beginning on the second postoperative day.
Summary of the performed surgeries
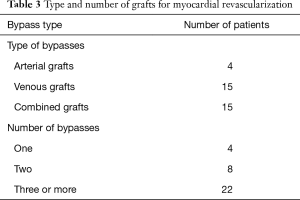
All patients underwent myocardial revascularization prior to lung resection. The average number of anastomosed coronary vessels was 2.4. Approximately 1/3 of the mammary arteries were used as free grafts. Details of the type and the number of anastomosed vessels are presented in Table 3.
Full table
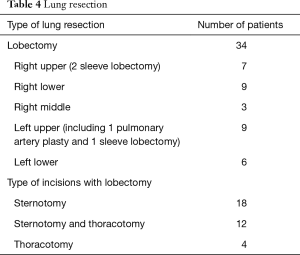
In all 34 patients, 18 underwent lobectomy and lymphadenectomy with or without the assistance of thoracoscopy through a sternotomic approach, 12 underwent lobectomy and lymphadenectomy through a lateral thoractomy approach following myocardial revascularization via sternotomy, 3 patients underwent bypass to the LAD and left lobectomy through a left thoracotomy, and 1 patient underwent bypass to the RAC and right lobectomy through a right thoracotomy. The type and the number of lung resections are detailed in Table 4.
Full table
Lung resection
Outcome of postoperative follow-up
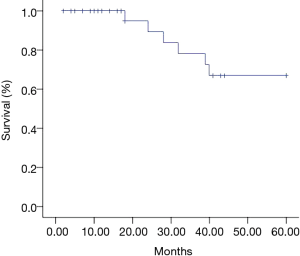
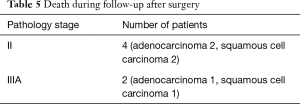
As of December 31, 2014, the overall follow-up period varied from 5 to 60 months, with an average of 30.2±20.1 months. Cancer recurrence occurred in 7 patients, 6 of them died during the follow-up period, with 4 patients developing distant metastases and two having local cancer recurrence (two N2 patients died during the first two postoperative years). All details of death are shown in Table 5. Four patients developed distant metastases and 2 had local recurrence. The remaining patients showed no evidence of tumor recurrence. Survival curves of all patients were drawn using the Kaplan-Meier method and the 3- and 5-year survival rates were 75% and 67%, respectively (Figure 1).
Full table
Discussion
In China, both the incidence of CHD and lung cancer are increasing. The numbers of coronary artery bypass grafts performed at our hospital increased from 833 to 4,613 between 2003 and 2015. More than 80% of these cases were OPCAB. Over 10,000 cases of percutaneous coronary intervention (PCI) were performed at our institution in 2015, while more than two hundred lung cancer resections are performed annually in our thoracic department. Typically, thoracic surgeons take the lead in decision making on operative treatment for patients who have both lung cancer and severe ischemic heart disease. In these cases, it is important to correct the severe ischemic symptoms in order to avoid MI caused by surgical trauma (11). Three solutions of therapeutic procedure are currently available in clinical practice: coronary angioplasty and/or stent placement before lung resection, simultaneous coronary artery bypass grafting (CABG) and lung resection (combined operation), and CABG followed by lung resection (two-stage operation).
Coronary angioplasty and stenting have been shown to be safe and effective in treating patients with coronary diseases (12). Limitations and risks exist for these procedures. Patients with left main coronary artery disease or three-vessel disease should not generally be considered for PCI. We also believed that PCI may increase the risk of postoperative bleeding related to antithrombotic medication for patients who received subsequent lobectomy (13). In fact, several lung cancer patients who also had single or double vessel coronary artery disease received PCI, and then underwent lung resection one month later in our department in recent years. Combined PCI with lung resection for these patients still remained controversial. However, in this group more than 2/3 of the patients were not considered to have indications for PCI.
CABG with CPB has been widely shown to be an effective procedure in patients with severe ischemic heart disease for several decades, but CPB may activate systemic inflammatory response syndrome, impair the immune response, deplete complement system factors, and cause lymphopenia, neutropenia, pulmonary sequestration of polymorphonuclear cells, and/or suppression of natural killer cells (14,15). Although some cases do occur, there is no conclusive evidence to suggest that CPB has an effect on stimulating tumor growth or accelerating spread of malignancy in these patients. Various studies have indicated the advantages of avoiding the use of CPB, which include reduced pulmonary dysfunction, decrease amount of transfused blood, shorter hospital and/or intensive care unit stay, and a decreased incidence of postoperative complications (16). Several publications have reported the results of combined OPCAB with lung resection. In these studies, patients usually had early stage lung cancer with one or two coronary artery disease. Despite the small number of patients in these studies, all reported that the combined procedure was feasible and safe with no additional complications (7-9). Compared to a two-stage operation, a one-stage procedure has potential advantages including a single induction of general anesthesia, a single incision for simple lung resections, shorter overall hospital stay, reduced cost of treatment, and no delay in the treatment of the lung cancer.
In the combined procedure, timing and sequence of the surgical steps should be carefully considered. The main goal of a combined cardiothoracic operation is to avoid perioperative myocardial ischemia, thus OPCAB should be performed first (17). In the first nine patients in this study, we performed a combined OPCAB and lung resection through two incisions (sternotomy and thoracotomy or muscle-sparing incision). However, the combined surgical interventions completed through two incisions led to a longer operative time and more severe postoperative pain compared to one incision. In order to improve this, we amended the procedure so that the lung resection was performed through the same sternotomic incision—a technique reported as early as 1975 (18). Urschel and Razzuk even considered median sternotomy as a standard approach for pulmonary surgery including lung cancer resection (19). In their study, patients receiving median sternotomy for lung resection had reduced operative time, postoperative pain, and hospital stay when compared to patients who underwent a lateral thoracotomy (19). Certainly, it is unconventional to perform lung resections through the sternotomy approach, especially the left lower lobectomy (20). Limited exposure of the chest form sternotomy may cause technical difficulty in resecting the lung and mediastinal lymphnodes, especially if both internal thoracic arteries are implanted. We suggest the use of only one mammary artery on the contralateral side and sequential implantation of venous grafts bypassed to diseased vessels. On the other hand, the usage of the thoracoscope may also help resolve these problems.
During the last ten years, the thoracoscope has been used extensively in thoracic surgery. Various studies have indicated many advantages of VATS lobectomy compared to open lobectomy, including reduced pulmonary dysfunction, decreased amount of transfused blood, and shorter hospital and/or ICU stays, as well as a decreased incidence of postoperative complications in early stage lung cancer (21,22). In the present series, we successfully performed 18 lobectomies through a sternotomy approach with the help of thoracoscopy, including 2 left lower lobectomies. The thoracoscopic-assistance provides a magnified image of the surgical field, especially of the back of hilar and mediastinum. However, for complicated procedures, such as bronchial sleeve resection or severe adhesion to the chest cavity, resection through sternotomy may be difficult and time-consuming. Thus, in three cases we performed combined interventions for complicated resections using sternotomy and muscle-sparing thoracotomy incisions. Regardless of whether VATS or an open approach is utilized, lymphadenectomy is important for exact staging and may improve postoperative survival. Although there is significant debate on the extent of lymph node dissection, we agree with Miller and colleagues who concluded that radical systematic mediastinal lymphadenectomy is advantageous (10).
In the present study, there were 2 respiratory complications (5.9%) and 5 cardiac arrhythmias (14.7%). These complication rates following combined surgery were comparable to those reported by Lamy et al. in their randomized controlled trial of 4,752 patients at 79 centers in 19 countries (23). They compared 30-day outcomes between OPCAB and CABG and found that the complication rates of respiratory and atrial fibrillation following OPCAB were 5.9% and 18.3%, respectively (23). It is notable that the lung resection after OPCAB did not increase overall complications in our study.
Although the 5-year survival benefit is only 4–5%, platinum-based adjuvant chemotherapy is considered the standard treatment for resectable lung cancer staging II to IIIA. In view of the potential risk of chemotherapy for these patients who underwent combined surgery, only 5 patients (including 2 who were N2 positive) herein received chemotherapy of platinum plus Gemcitabine (Gemzar) or Docetaxel (Taxotere) within 2 months following surgery. All of these patients completed 3–4 cycles of chemotherapy and tolerated it well.
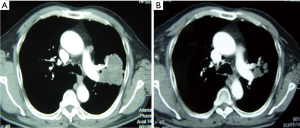
We also used chemotherapy for local advanced lung cancer (squamous cell carcinoma) in two patients with three-vessel disease before the combined procedure. In one patient with cancer involving left main pulmonary artery, we tried to avoid doing a pneumonectomy (Figure 2), and in the second patient, the left lower lobe tumor was very close to the opening of the bronchus of upper lobe. These two patients were given two cycles of platinum with Gemzar. After chemotherapy, the tumors shrank markedly in both cases and they subsequently underwent combined operations, one with a left upper lobectomy and angioplasty of pulmonary artery, and the other with a left lower lobe sleeve resection. These two patients continued receiving chemotherapy for four cycles. As of 4-year follow-up, both patients have not has any tumor recurrence. We believe that systemic therapy may play a role in improving the long-term survival in select patients following concomitant surgery. The overall 5-year survival rate for our patients was satisfactory and very similar to the general surgical outcome of lung cancer at 60–80% for stage I and 40–60% for stage II (24).
This study is limited by its prospective, and not randomized controlled design as well as the relative small number of patients. Most patients preferred a one-stage surgical intervention. As it was not possible to establish a control group in this setting, we can only definitively conclude that the combined procedure is safe, based on observed complication data, and technically feasible. While surgical decision-making should be centered on patients’ specific needs, we believe that suitable candidates for this procedure are patients with early-stage non-small cell lung cancer (stage I to II). Patients with N2 positive disease should not be considered because of the generally poor results of surgical treatment in these patients. Extensive and severe adhesions in the chest cavity or complicated lung resections, such as those requiring bronchial sleeve resection and vascular plastic procedures, may not be suitable for simultaneous operations through a sternotomy approach. Furthermore, patients with a history of recent MI within the previous 30 days, unstable haemodynamics, and/or serious regional wall motion abnormalities, are not suitable for this procedure (25).
Conclusions
Combined OPCAB and pulmonary resection for early-stage lung cancer patients with concurrent severe CHD is a relatively safe and effective treatment with satisfactory long-term survival rates. Additionally, this procedure is a safe option in patients with three-vessel disease who are usually not candidates for preoperative PCI.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was conducted in accordance with the Helsinki declaration and with approval from the Ethics Committee of Beijing Anzhen Hospital (NO. 2013016X). Written informed consent was obtained from all participants.
References
- Jiang G, Wang D, Li W, et al. Coronary heart disease mortality in China: age, gender, and urban-rural gaps during epidemiological transition. Rev Panam Salud Publica 2012;31:317-24. [Crossref] [PubMed]
- Chen PC, Muo CH, Lee YT, et al. Lung cancer and incidence of stroke: a population-based cohort study. Stroke 2011;42:3034-9. [Crossref] [PubMed]
- Ciriaco P, Carretta A, Calori G, et al. Lung resection for cancer in patients with coronary arterial disease: analysis of short-term results. Eur J Cardiothorac Surg 2002;22:35-40. [Crossref] [PubMed]
- Chassot PG, Delabays A, Spahn DR. Preoperative evaluation of patients with, or at risk of, coronary artery disease undergoing non-cardiac surgery. Br J Anaesth 2002;89:747-59. [Crossref] [PubMed]
- Brutel de la Rivière A, Knaepen P, et al. Concomitant open heart surgery and pulmonary resection for lung cancer. Eur J Cardiothorac Surg 1995;9:310-3; discussion 313-4. [Crossref] [PubMed]
- Dyszkiewicz W, Jemielity MM, Piwkowski CT, et al. Simultaneous lung resection for cancer and myocardial revascularization without cardiopulmonary bypass (off-pump coronary artery bypass grafting). Ann Thorac Surg 2004;77:1023-7. [Crossref] [PubMed]
- Saxena P, Tam RK. Combined off-pump coronary artery bypass surgery and pulmonary resection. Ann Thorac Surg 2004;78:498-501. [Crossref] [PubMed]
- Schoenmakers MC, van Boven WJ, van den Bosch J, et al. Comparison of on-pump or off-pump coronary artery revascularization with lung resection. Ann Thorac Surg 2007;84:504-9. [Crossref] [PubMed]
- Dyszkiewicz W, Jemielity M, Piwkowski C, et al. The early and late results of combined off-pump coronary artery bypass grafting and pulmonary resection in patients with concomitant lung cancer and unstable coronary heart disease. Eur J Cardiothorac Surg 2008;34:531-5. [Crossref] [PubMed]
- Miller DL, Orszulak TA, Pairolero PC, et al. Combined operation for lung cancer and cardiac disease. Ann Thorac Surg 1994;58:989-93; discussion 993-4. [Crossref] [PubMed]
- Takamochi K, Oh S, Matsuoka J, et al. Risk factors for morbidity after pulmonary resection for lung cancer in younger and elderly patients. Interact Cardiovasc Thorac Surg 2011;12:739-43. [Crossref] [PubMed]
- Hernández JM, Fernández JF, Tenas MS, et al. Update on interventional cardiology. Rev Esp Cardiol (Engl Ed) 2012;65 Suppl 1:4-11. [PubMed]
- Kałuza GL, Joseph J, Lee JR, et al. Catastrophic outcomes of noncardiac surgery soon after coronary stenting. J Am Coll Cardiol 2000;35:1288-94. [Crossref] [PubMed]
- Ulicny KS Jr, Schmelzer V, Flege JB Jr, et al. Concomitant cardiac and pulmonary operation: the role of cardiopulmonary bypass. Ann Thorac Surg 1992;54:289-95. [Crossref] [PubMed]
- Partrick DA, Moore EE, Fullerton DA, et al. Cardiopulmonary bypass renders patients at risk for multiple organ failure via early neutrophil priming and late neutrophil disability. J Surg Res 1999;86:42-9. [Crossref] [PubMed]
- Rao V, Todd TR, Weisel RD, et al. Results of combined pulmonary resection and cardiac operation. Ann Thorac Surg 1996;62:342-6; discussion 346-7. [Crossref] [PubMed]
- Danton MH, Anikin VA, McManus KG, et al. Simultaneous cardiac surgery with pulmonary resection: presentation of series and review of literature. Eur J Cardiothorac Surg 1998;13:667-72. [Crossref] [PubMed]
- Meyer JM, Myburgh JA, Erasmus FR. Operative surgery of giant bilateral bullae of the lungs. S Afr Med J 1975;49:777-80. [PubMed]
- Urschel HC Jr, Razzuk MA. Median sternotomy as a standard approach for pulmonary resection. Ann Thorac Surg 1986;41:130-4. [Crossref] [PubMed]
- Voets AJ, Joesoef KS, van Teeffelen ME. Synchroneously occurring lung cancer (stages I-II) and coronary artery disease: concomitant versus staged surgical approach. Eur J Cardiothorac Surg 1997;12:713-7. [Crossref] [PubMed]
- Jheon S, Yang HC, Cho S. Video-assisted thoracic surgery for lung cancer. Gen Thorac Cardiovasc Surg 2012;60:255-60. [Crossref] [PubMed]
- Murthy S. Video-assisted thoracoscopic surgery for the treatment of lung cancer. Cleve Clin J Med 2012;79 Electronic Suppl 1:eS23-5.
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Off-pump or on-pump coronary-artery bypass grafting at 30 days. N Engl J Med 2012;366:1489-97. [Crossref] [PubMed]
- Gorenstein LA, Sonett JR. The surgical management of stage I and stage II lung cancer. Surg Oncol Clin N Am 2011;20:701-20. [Crossref] [PubMed]
- Ma XC, Ou SL, Zhang ZT, et al. Outcomes of combined pulmonary resection and off-pump coronary artery bypass grafting for patients with lung tumor and concurrent coronary heart disease. Zhonghua Yi Xue Za Zhi 2012;92:3134-6. [PubMed]