Nuss procedure for repair of pectus excavatum after failed Ravitch procedure in adults: indications and caveats
Introduction
For decades symptomatic patients underwent open correction of pectus excavatum (PE) using the technique described by Ravitch et al. (1) or modifications of this original approach. With the development of the minimally invasive approach for PE repair by Nuss et al. (2) the Ravitch technique was more and more displaced. Numerous studies have demonstrated the efficacy and safety of the Nuss procedure as primary treatment for PE, not only in children, but also in young adults (3,4). Although both techniques are still widely used for the correction of PE, the Nuss approach is mainly preferred in children due to its lesser invasiveness (3). Recurrence rate after open repair of PE using the Ravitch technique has been reported to be between 2% and 37% (5-10). In addition a substantial number of unreported cases must be assumed, since most patients with recurrence seek a second opinion and revision at another centre. Possible reasons for recurrent disease after open repair are numerous, including primary repair before completion of teenage growth, insufficient surgical technique (e.g., insufficient strut support, premature strut removal), malunion and many more. Several techniques including open approaches, minimally invasive as well as hybrid techniques have been described for repair of recurrent PE, with minimally invasive techniques being predominantly used in children and young adults only (6-11). Aim of the present series was to investigate the efficacy and safety of the minimally invasive Nuss procedure for repair of recurrent PE after prior Ravitch surgery in adults.
Methods
After institutional review board approval (Mayo Clinic, Arizona) and after obtaining informed consent from all patients (Inselspital Bern) a retrospective review of all patients undergoing minimally invasive repair for recurrent PE after failed Ravitch repair between July 2007 and August 2014 was performed. While the primary operations took place in different outside hospitals, 6 patients were referred to University Hospital Bern and 14 patients to Mayo Clinic Arizona for repair of recurrent PE. In the present series two patients from Bern and one Patient operated at Mayo did show sternal malunion on CT scan but without significant clinical sternal instability. At Mayo patients with malunion and severe sternal instability were routinely scheduled for a hybrid procedure and thus excluded from the study. The patients’ charts were reviewed including information and notes from the patient’s initial surgery at outside institutions if available. Follow-up visits were scheduled 3 months after the Nuss procedure, followed by yearly controls until bar removal around 3 years after its implantation and 3 months after bar removal to evaluate the final result.
Surgical technique
The operative technique for minimally invasive repair of recurrent PE was similar to the technique for primary PE correction. Intravenous antibiotic prophylaxis was administered approximately 30 min before the procedure. General anesthesia with double-lumen intubation was performed and the patient was put in a supine position. A 5 mm port was placed in the right midaxillary line for the thoracoscope and when adhesions were present, as seen in most of the patients, additional carbon dioxide insufflation up to 8 mmHg pressure was administered. Two bilateral 3- to 4-cm incisions were made at the inferolateral pectoral borders. For patients at Mayo Clinic, forced sternal elevation was used prior to dissection of the mediastinum. An incision was placed on either sides of sternum and the perforating tips of bone clamp attached. The clamp is then attached to the Rultract® Retractor (Rultract Inc., Cleveland, OH, USA) and sternum elevated (12). For take down of adhesions electrocautery was introduced through another 5 mm port on the right side. A Lorentz dissector was then passed from right to left under the sternum in order to exit through the contralateral intercostal interspace. An Ethibond ribbon (Bern) or FiberWire® (Mayo) was then attached to the dissectors end to guide the placement of the custom formed implant bar. The bar was then rotated into its final position and one or two stabilizers were attached to the pectus bar end. At Mayo all bars underwent bilateral fixation with FiberWire® (Arthrex Inc., Naples, FL, USA) around the underlying ribs. In total two or three bars were placed depending on the achieved correction of the deformity and the estimated optimization of the correction by the use of an additional bar. In the end of the procedure a 24 French chest tube was inserted through one of the 5 mm trocar incisions on the right side and connected to an underwater seal.
Results
In our cohort of 20 patients, the gender ratio was 3:1 with 15 male and 5 female patients. The mean age at primary surgery was 21 years (range, 2–50 years), while it was 31.1 years (range, 18–52 years) for redo. In 9 patients the Ravitch repair involved retrosternal placement of a supportive strut bar, which was removed after an average time of 13 months (range, 6–24 months).
One out of the 20 patients initially suffered from a combined PE/carinatum deformity, whereas the remaining 19 patients suffered from isolated excavatum deformity.
The initial HI (prior to any surgical intervention) was only available in 5 patients and was in the range of 4.5–22.2 (mean: 9.1), except for the patient with combined deformity, who showed a HI of 1.5.
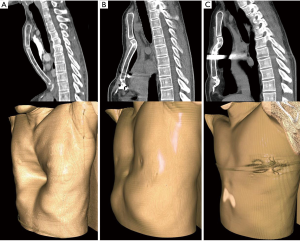
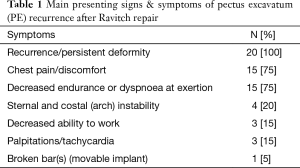
More than half of the patients presented either with persistent disease (n=6) after Ravitch (Figure 1) or early recurrence within the first year after primary surgery (n=4). In the remaining patients recurrence was either becoming evident immediately after strut removal (n=5) or it was slowly progressive over several [5–10] years (n=5). An interesting finding was that in only two of the six patients with persistent disease a supportive retrosternal strut was placed. The patients’ main presenting symptoms are listed in Table 1.
Full table
The mean time between primary Ravitch procedure and redo surgery was 10.5 years (range, 0.25–47 years). For the 6 patients treated in Bern, mean Haller index after final bar removal was 2.52 (range, 2.1–2.9) compared to 4.7 (range, 3.1–7.85) before re-do after Ravitch. Bar removal was performed after a mean time of 4.3 years (range, 3–5.8 years). At Mayo the mean time between Nuss procedure and removal was 3.2 years (range, 1–4.2 years), but unfortunately before and after Haller indices were not available for most patients.
Mean number of implanted bars during redo surgery was 1.95 (range, 1–3). In Bern either one (n=5) or two (n=1) stabilizers were used, whereas at Mayo stabilizers were not routinely used and the bar was rather secured with FiberWire around the ribs. The average time between re-do and final bar removal was 3.5 years (range, 1.1–5.8 years).
All patients were successfully repaired using a modified minimally invasive Nuss technique. No major intra- or postoperative complications occurred. Compared to a primary Nuss procedure which usually takes around 30–45 min, the duration of the secondary operation was significantly prolonged with a mean procedure duration of 138 min (range, 52–308 min) in Bern and 165 min (range, 60–308 min) for the Mayo group, respectively. Due to previous surgery almost all patients (n=18; 90%) required dissection of adhesions up to some degree.
In a few patients additional manoeuvres such as costal wedge-osteotomy (n=1) or osteophyte-excision (n=1) had to be performed. Mean hospital stay was 7.8 days (range, 4–11 days). Only one patient suffered from a mild complication in form of a local wound fistula, which was excised at the time of final bar removal 3 years after the Nuss procedure.
Postoperative follow-up
Average follow-up after redo surgery was 41.8 months (range, 8–76 months).
In 13 patients final bar removal was performed after a mean time of 3.6 years (range, 1.1–5.8 days).
The remaining 7 patients have not yet progressed through bar removal, but X-rays show a stable result without any signs of bar displacement so far.
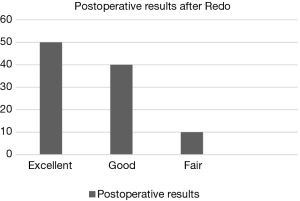
During follow-up patients were also asked to assess the final result after redo surgery, which is depicted in Figure 2. The classification was divided into four different groups: “excellent” if the preoperative symptomatology has disappeared and the chest appeared normal; “good” if preoperative symptoms were resolved and the thoracic deformity has substantially improved to a satisfying level; “fair” if pain was a persistent problem and/or if patients weren’t completely satisfied with the cosmetic result although the deformity has been markedly improved; and “failed” if the symptoms persisted or got worse and the deformity persisted or recurred again.
Concerning the two patients with fair results: one of them still suffers from recurrent pain episodes after the highly severe PE deformity with a HI of 22.2, finally corrected to an acceptable result with a HI of 2.9. The second patient initially underwent Ravitch for combined PE/PC deformity and suffered from chronic pain since the first procedure. Even after redo and finally removal of all 3 Nuss bars chronic pain is still a major problem, although the deformity shows an acceptable cosmetic result. No result was considered a failure.
Discussion
Recurrence of PE after open repair is not an uncommon problem, occurring in up to more than a third of operated patients (5). Main possible reasons, which might have resulted in early recurrence in the present series, were missing or insufficient strut support and premature strut removal. Slowly progressive recurrence over years can occur when correction is performed before completion of teenage growth, and recurrence which is observed after strut removal is usually a sign of malunion with sternal instability. However, independent from the underlying cause of recurrent disease, redo surgery can be rather challenging. For example pleuropulmonary adhesions complicated surgery to some extent in all of our patients. This problem may be overcome by insertion of an additional assistant trocar, CO2-insufflation into the pleural cavity and/or bilateral thoracoscopy in selected cases. Forced sternal elevation is another helpful tool that can be used in order to improve visualization and facilitate the procedure in these difficult cases (12).
In the present series correction in all patients was successfully performed using the minimally invasive Nuss technique. It has to be noted that none of the abovementioned patients suffered from severe sternal instability in form of a “floating sternum” due to malunion. In such cases often more extensive open or combined approaches are necessary to achieve an acceptable and durable result of correction (11). For the three patients in the present series with malunion and only slight sternal instability, the Nuss technique was adequate for repair.
In our opinion the Nuss procedure is a good approach for recurrence of PE after open repair for two main reasons: first, there is no need to re-open the scarred region of the anterior chest wall which usually would include extensive dissection, because the Nuss technique allows to approach the deformity from the other side (i.e., from inside). Second, the pectus bar itself is strong enough to adequately correct the deformity and at the same time withstand the inward pressure of the sternum, even in adult patients with scarred and thus stiffer chest wall. In comparison to primary Nuss in PE patients, the procedure in these patients is clearly more challenging, especially due to adhesions between lung and chest wall as well as between the mediastinum and the sternum, respectively. This did not only lead to prolonged operating times, but also may increase the risk of complications such as bleeding and air leak. Fortunately this was not a major problem in our patients. Nevertheless meticulous care has to be taken not to injure any vital structures and other authors also have suggested extended draping for surgery including the groins to allow rapid emergent access to the femoral vessels in case of an emergency (11).
Main limitation of this study is that the study cohort did not at all consist of a homogeneous group of patients. Due to the nature of the problem, every single patient has his or her own distinct history of the initial deformity, of how it was surgically treated, of how the outcome was and of what his or her expectations were. This also brings up the importance of a thorough education of the patient, not only about the extent of surgery and potential complications, but also on the expectations of the final result after a redo correction.
As demonstrated in the present series, minimally invasive correction of recurrent PE after open repair is a valid treatment option in experienced centres, not only in children as previously described (5,6), but also in adults as shown by the present study. Although the procedure is usually more challenging, mostly due to intrathoracic adhesions, good results can be achieved and complications can be minimized with meticulous surgical technique. In case of severe sternal instability due to malunion, a hybrid approach is preferred, which allows the placement of a Nuss bar with concomitant open fixation of the sternum (11).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by institutional review board (Mayo Clinic, Arizona) and written informed consent was obtained from all patients.
References
- Ravitch MM. The Operative Treatment of Pectus Excavatum. Ann Surg 1949;129:429-44. [Crossref] [PubMed]
- Nuss D, Kelly RE Jr, Croitoru DP, et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998;33:545-52. [Crossref] [PubMed]
- Johnson WR, Fedor D, Singhal S. Systematic review of surgical treatment techniques for adult and pediatric patients with pectus excavatum. J Cardiothorac Surg 2014;9:25. [Crossref] [PubMed]
- Hanna WC, Ko MA, Blitz M, et al. Thoracoscopic Nuss procedure for young adults with pectus excavatum: excellent midterm results and patient satisfaction. Ann Thorac Surg 2013;96:1033-6; discussion 1037-8. [Crossref] [PubMed]
- Croitoru DP, Kelly RE Jr, Goretsky MJ, et al. The minimally invasive Nuss technique for recurrent or failed pectus excavatum repair in 50 patients. J Pediatr Surg 2005;40:181-6; discussion 186-7. [Crossref] [PubMed]
- Redlinger RE Jr, Kelly RE Jr, Nuss D, et al. One hundred patients with recurrent pectus excavatum repaired via the minimally invasive Nuss technique--effective in most regardless of initial operative approach. J Pediatr Surg 2011;46:1177-81. [Crossref] [PubMed]
- Guo L, Mei J, Ding F, et al. Modified Nuss procedure in the treatment of recurrent pectus excavatum after open repair. Interact Cardiovasc Thorac Surg 2013;17:258-62. [Crossref] [PubMed]
- Ellis DG, Snyder CL, Mann CM. The 're-do' chest wall deformity correction. J Pediatr Surg 1997;32:1267-71. [Crossref] [PubMed]
- Wang L, Zhong H, Zhang FX, et al. Minimally invasive Nuss technique allows for repair of recurrent pectus excavatum following the Ravitch procedure: report of 12 cases. Surg Today 2011;41:1156-60. [Crossref] [PubMed]
- Miller KA, Ostlie DJ, Wade K, et al. Minimally invasive bar repair for 'redo' correction of pectus excavatum. J Pediatr Surg 2002;37:1090-2. [Crossref] [PubMed]
- Johnson KN, Jaroszewski DE, Ewais M, et al. Hybrid Technique for Repair of Recurrent Pectus Excavatum After Failed Open Repair. Ann Thorac Surg 2015;99:1936-43. [Crossref] [PubMed]
- Jaroszewski DE, Johnson K, McMahon L, et al. Sternal elevation before passing bars: a technique for improving visualization and facilitating minimally invasive pectus excavatum repair in adult patients. J Thorac Cardiovasc Surg 2014;147:1093-5. [Crossref] [PubMed]